Addiction and mental health problems can affect anyone, even the rich and famous. But if you’re used to a high standard of living, you might worry about giving up comfort during inpatient treatment. Celebrity rehab centers offer the perfect solution. These luxury facilities provide top-notch health care while maintaining the comforts you enjoy in daily life.
What Makes Celebrity Rehabs Special?
Celebrity rehabs combine effective treatment with luxury experiences. At these centers, you might go whale watching, take a sunset yacht ride, or enjoy skydiving adventures. Many look like high-end resorts or tropical getaways from the outside. But inside, they offer much more than a fancy vacation.
These facilities maintain strict privacy measures to protect their famous clients. Most have security teams, private rooms, and confidentiality agreements for all staff. Some centers don’t even have map listings, to keep their location secret from the public and media.
The best celebrity rehabs focus on both comfort and effective treatment. They employ highly qualified therapists, doctors, and support staff. Many offer personalized treatment plans tailored to your unique needs.
Celebrity Rehab Centers Around the World
You can find celebrity rehabs around the globe, with a wide variety of treatments and amenities. Whether you prefer the tropics, a mountain retreat, or a private island oasis, there’s most likely a treatment facility that meets your needs.

1. Exclusive Hawaii Rehab
This oceanside center prioritizes privacy with a gated residence hidden from the road. A security team guards the property 24/7. The center treats a maximum of 7 clients at once, offering 3 room options: shared, private with shared bathroom, or private with en suite.
Exclusive Hawaii Rehab offers naturopathic and holistic therapies for drug addiction and mental health. They provide nutritional counseling, IV therapies, and traditional Hawaiian Ho’oponopono sessions. Clients can keep up with work during recovery, with access to phones, laptops, and dedicated workspaces.
When you’re not in therapy, you can feed manta rays, take cooking classes, visit waterfalls, or simply relax on the beach.

2. Passages Malibu
Located on the sunny coast of Los Angeles County, Passages Malibu focuses heavily on individual therapy. Clients receive 60-80 hours of one-on-one therapy each month. Famous past clients include Mel Gibson, Andy Dick, and Stephen Baldwin.
Passages doesn’t use 12-Step methods. Instead, they see substance use disorder as a treatable condition with root causes that can be addressed. Their holistic approach includes hypnotherapy, acupuncture, and massage alongside traditional talk therapy.
The center offers shared or private rooms with access to lounge areas and multiple pools. On-site chefs prepare nutritious meals customized to your dietary needs.

3. Cirque Lodge
In the pristine nature of Utah, Cirque Lodge provides substance abuse and co-occurring disorder recovery in a lodge-style setting. Famous clients have included Cara Delevigne, Demi Moore, Lindsay Lohan, and Kirsten Dunst.
Cirque Lodge incorporates the 12 Steps along with other evidence-based therapies. They also offer unique experiential treatments like equine therapy. Clients enjoy private bedrooms with en suite bathrooms in a cozy environment.
The campus provides plenty of opportunities to enjoy nature, with stunning views and outdoor activities in the sunny Utah weather.

4. NEOVIVA
This Swiss rehab center operates discreetly within a hotel on Lake Lucerne. With no signage or staff uniforms, clients look just like any other hotel guest. Treatment sessions take place in a private section away from other guests.
NEOVIVA maintains a 1:3 staff-to-client ratio and treats just 5 clients at a time. Each private room overlooks the lake. Clients have access to all hotel amenities, including a sauna, restaurant, and outdoor pool. You can even bring your pet.
Their holistic approach includes wellness treatments like yoga, breath work, and Qigong. Weekend activities might include forest hikes, trips to nearby villages, and time at the famous lake.

5. AToN Center
Located on 10 acres in San Diego, AToN Center provides privacy and luxury. They offer both 12-Step and non-12-Step approaches. Their treatment combines evidence-based, holistic, and trauma-informed therapies.
Clients receive 4 hours of therapy daily, including 3 hours of group therapy and 1 hour of individual therapy sessions. Family therapy is available weekly. The center doesn’t restrict access to devices as long as they don’t interfere with treatment.
Holistic treatment options include weekly acupuncture, massage, personal training, yoga, and hypnotherapy. Clients can also enjoy hiking, painting classes, meditation, and Reiki energy healing.

6. Istana Bespoke Health
Istana takes privacy to the extreme by treating just one client at a time. They have locations in Ibiza, Bali, and Barbados, each offering a private villa for recovery. Family members can join if the treatment team agrees it would be helpful.
The program offers completely customized treatment using evidence-based approaches like cognitive behavioral therapy (CBT). Privacy measures include unmarked villas, private airport pickups, and staff trained in confidentiality.
Each client receives support from a butler, personal chef, and life coach, among others. Free-time activities include island tours, cooking classes, music making, and dance lessons.

7. Clinic Les Alpes
A luxury chalet in the Swiss mountains, Clinic Les Alpes treats addiction, mental health disorders, eating disorders, burnout, and more. Their world-renowned practitioners create personalized treatment plans using advanced testing and assessments.
Clients enjoy private bedrooms and amenities like a sauna, swimming pool, mountain views, and a gym. Every aspect of treatment is tailored to individual needs, including nutritional care.
The stunning Alpine setting provides a peaceful backdrop for recovery, away from the pressures of public life.

8. Raindrum
Raindrum offers ultra-private mental health and addiction treatment in various settings. Clients choose between several private residences, either on the beach or in the countryside. All therapy takes place one-on-one, including talk therapy and personal training.
This center treats addiction along with co-occurring conditions like burnout, depression, and anxiety. They offer experiential therapies like surf therapy, equine therapy, dance, and photography, as well as creative options like art therapy, pottery, and language learning.
Treatment is completely individualized, with staff coming to your residence rather than meeting in a clinical setting. A full support team includes housekeepers and a personal chef.
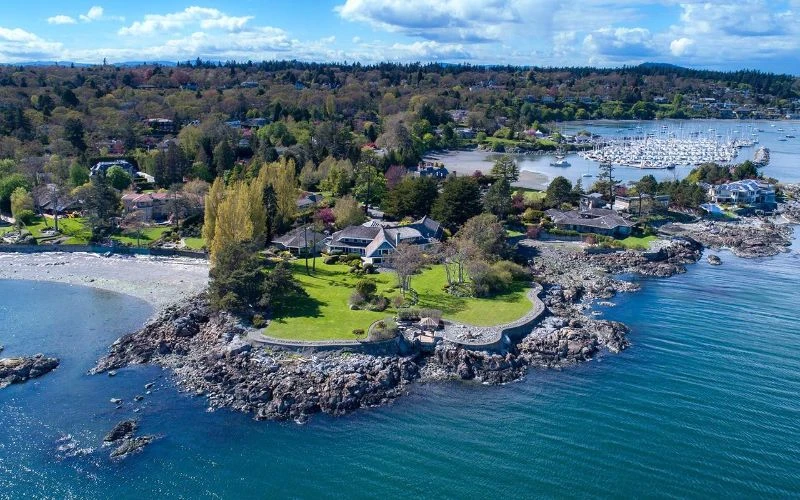
9. The Sanctuary Vancouver Island
This bespoke center offers high-end treatment for various needs. Beyond addiction and mental health, they focus on chronic pain management, post-operative care, and weight stabilizing.
The Sanctuary Vancouver Island combines evidence-based and alternative treatments, such as CBT with transcranial magnetic stimulation (TMS). More than 100 on-call specialists support your recovery process, from chiropractors to psychiatrists.
Clients stay in private residences on Vancouver Island near the shore, in the forest, or somewhere in between. Between sessions, you can enjoy meals from your personal chef, go whale watching, or explore by seaplane.
Finding Recovery as a Celebrity
Getting help for addiction doesn’t have to mean giving up luxury or privacy. These exclusive drug rehab centers prove you can heal while maintaining comfort and discretion.
The most effective addiction treatment centers combine evidence-based therapies with holistic approaches tailored to your needs. They maintain strict confidentiality via security measures, unmarked facilities, and staff training. And after treatment, you’ll take valuable coping skills with you, whether you’re heading back to the spotlight or to your private life.
Ready to start your journey back to well-being? Visit our collection of luxury treatment centers to find the perfect match for your needs and lifestyle.
FAQs
Q: How effective are celebrity rehab centers in treating addiction?
A: Celebrity rehab centers can be highly effective when they combine luxury with evidence-based treatments. They typically employ qualified professionals and maintain low client-to-staff ratios. Success rates vary by individual, but many clients find the personalized approach and comfortable environment help them engage better in treatment.
Q: What can I expect at a luxury rehab center?
A: Expect private accommodations, gourmet meals, and amenities like pools and spas. Treatment usually includes a combination of individual therapy, support groups, and holistic options like massage or acupuncture. Many centers allow access to phones and laptops, with recreational activities available. Low staff-to-client ratios ensure personalized care.
Q: How do I find the best celebrity alcohol rehab center?
A: Consider your needs, budget, and preferred location. Look for centers specializing in alcohol addiction with experienced, licensed staff and evidence-based approaches. Ask about detox if needed. Read reviews and ask questions about outpatient program options, privacy policies, and aftercare planning.
Q: How much does it cost to stay at a celebrity rehab center?
A: Mental health or substance abuse treatment costs at luxury rehabs typically range from $30,000 to $100,000+ per month, depending on the center and services provided.
