Have you ever found yourself procrastinating on something important, turning down a great opportunity, or saying something you didn’t mean—only to later ask, “Why did I do that?” If so, you’re not alone. Many of us engage in behaviors that quietly (or loudly) get in the way of our own goals, dreams, and wellbeing. This frustrating pattern is known as self-sabotage.
Self-sabotage doesn’t mean you’re broken or lazy. In fact, it often comes from a place of deep fear, learned survival strategies, or a nervous system trying to protect you—even when that protection causes harm. The good news? These patterns can be understood, challenged, and changed.
In this article, we’ll explore what self-sabotage is, why it happens, how to recognize it, and most importantly, what you can do to break the cycle. Whether you’re aware of your patterns or just starting to connect the dots, this article will help you move from your role as saboteur to protector.
What Is Self-Sabotage?
Self-sabotage refers to behaviors or thought patterns that hold us back from achieving our goals, often without us realizing it. These behaviors might seem helpful or necessary in the moment, but they tend to reinforce cycles of shame, avoidance, or fear.
Signs of Self-Sabotage
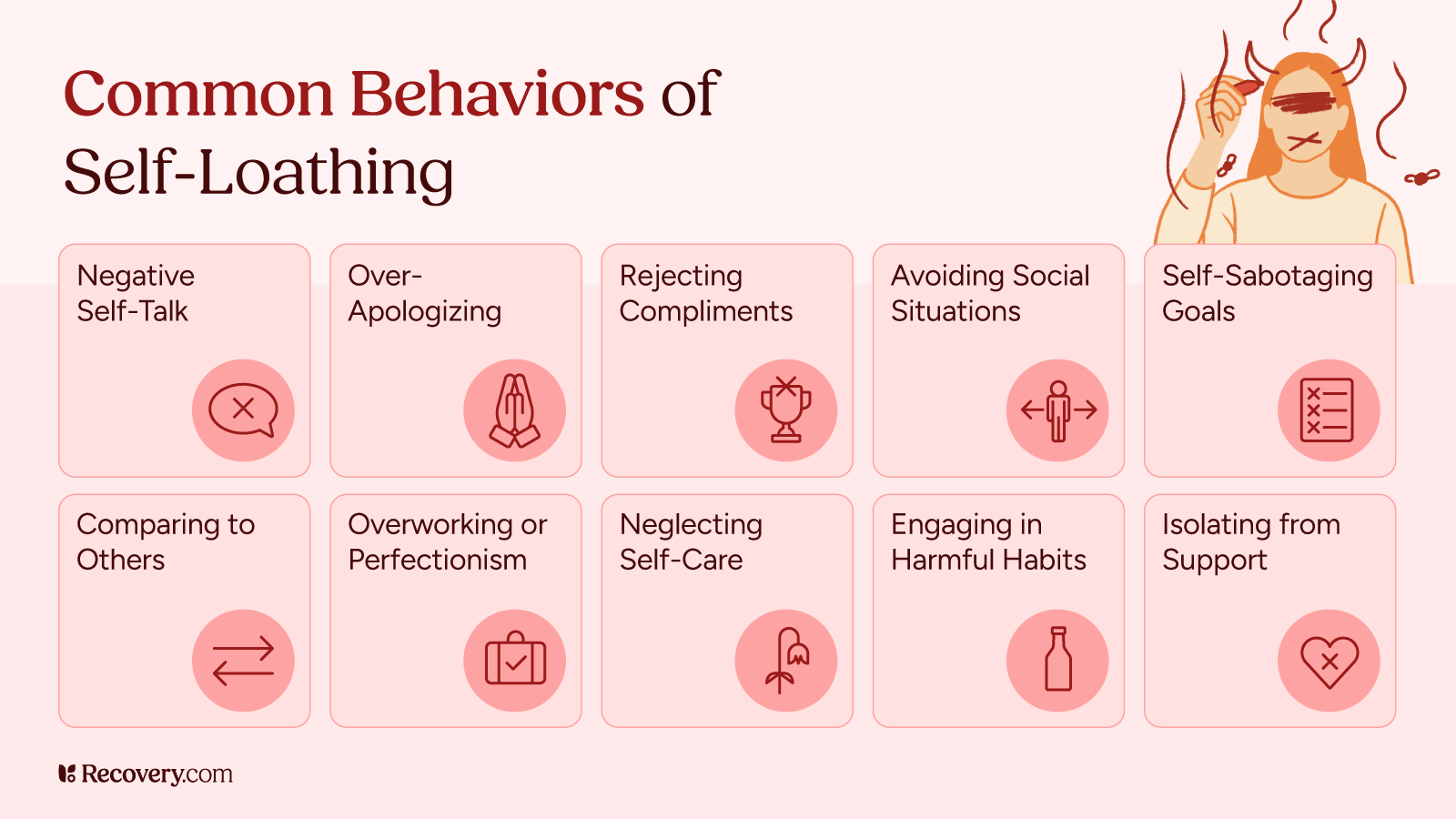
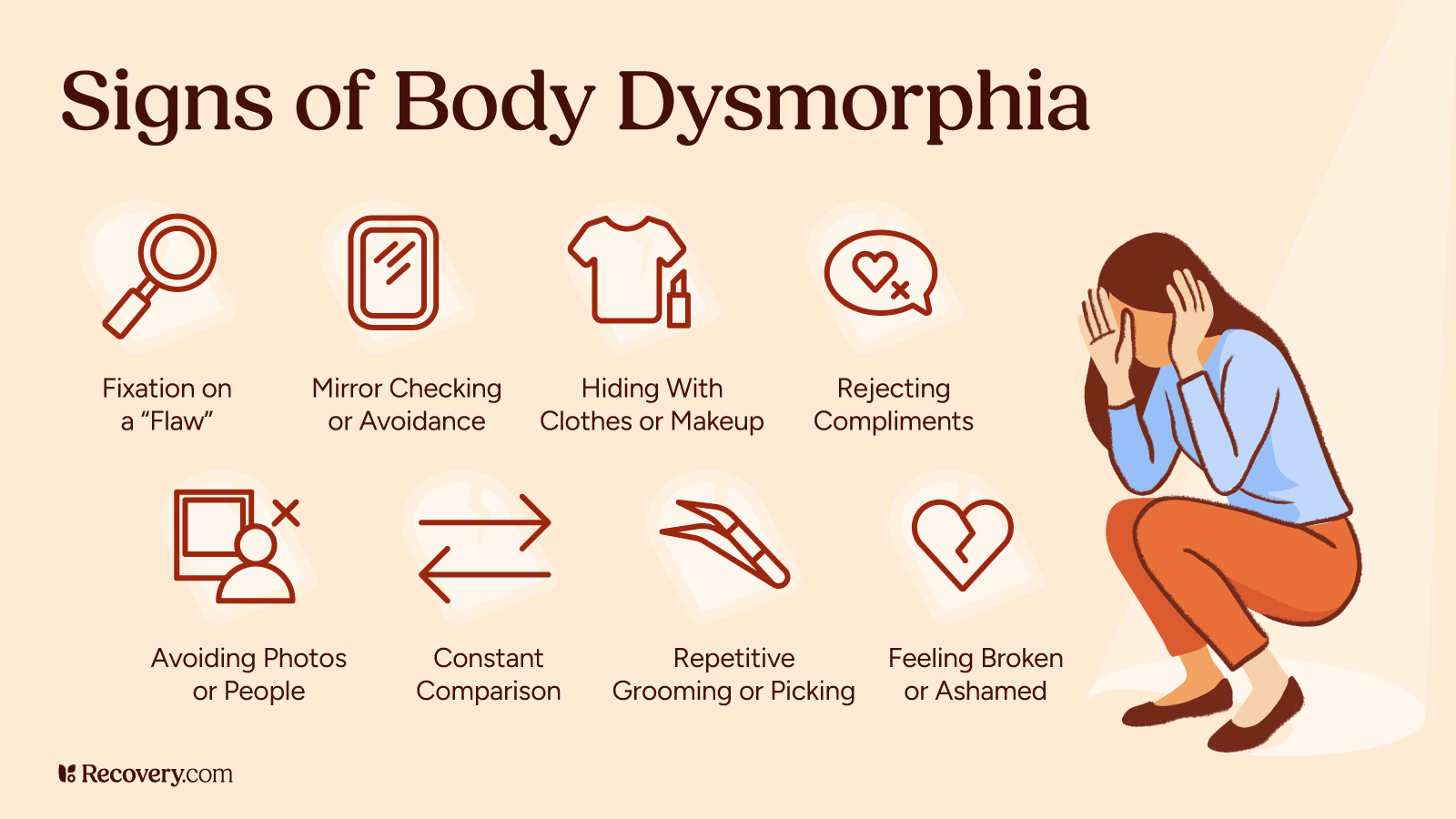
Self-sabotage can be subtle, and it doesn’t look the same for everyone. Here are some common signs that you may be engaging in self-sabotaging behavior:
- Procrastination or chronic avoidance
- Setting unrealistic goals (and then feeling like a failure for not meeting them)
- Negative self-talk and harsh self-criticism
- Starting projects or relationships strong and then abruptly withdrawing
- Sabotaging opportunities with perfectionism or last-minute panic
- Feeling uncomfortable or unworthy when things are going well
- Overcommitting and burning out
- Turning to unhealthy coping strategies like substance use, excessive screen time, or emotional eating
- Fear of asking for help or receiving support
- Procrastinating on assignments1 or projects despite having enough time, then blaming lack of time for poor performance
These patterns often lead to a cycle of regret, shame, and more sabotage. Recognizing the signs is the first step toward interrupting the pattern, increasing self-awareness, and taking steps towards personal growth.
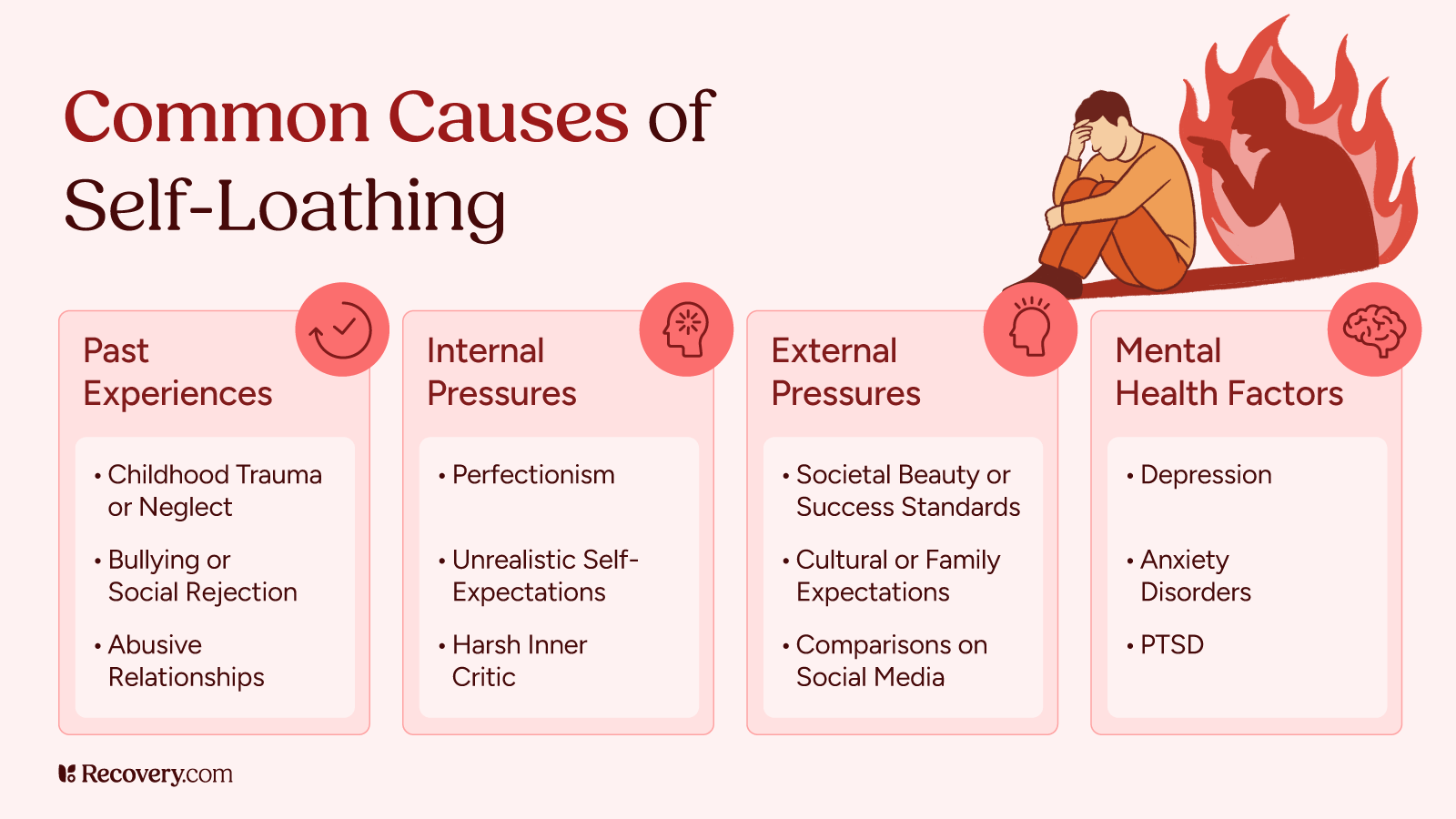
Why Do We Self-Sabotage?
Self-sabotage isn’t about weakness, there’s also no one form of self-sabotage. It’s usually a coping mechanism that may be getting in the way of personal and short-term or long-term goals.
Here are a few reasons self-sabotage might show up:
1. Fear of Failure (or Success)
If failure feels devastating, we might unconsciously create distance from our goals to avoid disappointment or to decrease vulnerability. Paradoxically, some experience fear of success.2 This is because success can be equally scary. It might mean change, pressure, or a shift in identity.
2. Low Self-Worth
If you carry the belief that you’re not good enough or don’t deserve good things, you might act in ways that reinforce that belief. This can include turning down opportunities, pushing people away, or giving up before you even begin.
3. Control and Predictability
Failing on our own terms can feel safer than risking the unknown. Self-sabotage can be a way of staying in control of outcomes, even painful ones.
4. Trauma and Protective Mechanisms
People who’ve experienced trauma3—especially relational trauma—may sabotage connection or progress as a way to stay emotionally safe. If thriving feels unfamiliar, the nervous system may respond with resistance.
When Should You Seek Help?
If self-sabotage is consistently interfering with your relationships, career, health, or mental wellbeing, it may be time to seek professional support.
You don’t have to hit “rock bottom” to benefit from therapy, but if it’s leading you to struggle with things like low self-esteem, negative thoughts, self-doubt, low self-confidence, limiting beliefs, or with your mental health in general, it may be time to reach out.
Here are some signs that outside help could be beneficial:
- You feel stuck in repetitive patterns you can’t break
- You frequently regret your actions but don’t know how to change
- Your inner critic feels overwhelming or cruel
- Perfectionist behaviors are getting in the way of self-improvement or success
- You avoid opportunities you deeply want out of fear
- You feel anxious, depressed, or emotionally numb much of the time
- You’re struggling to connect with loved ones or in your romantic relationships4
- You feel unable to stop self-destructive or self-defeating behaviors
- Negative beliefs and emotions lead you to experience overthinking, limit your own success, or disengage in self-care
You don’t have to figure it all out alone. Healing is possible—and you deserve support along the way.
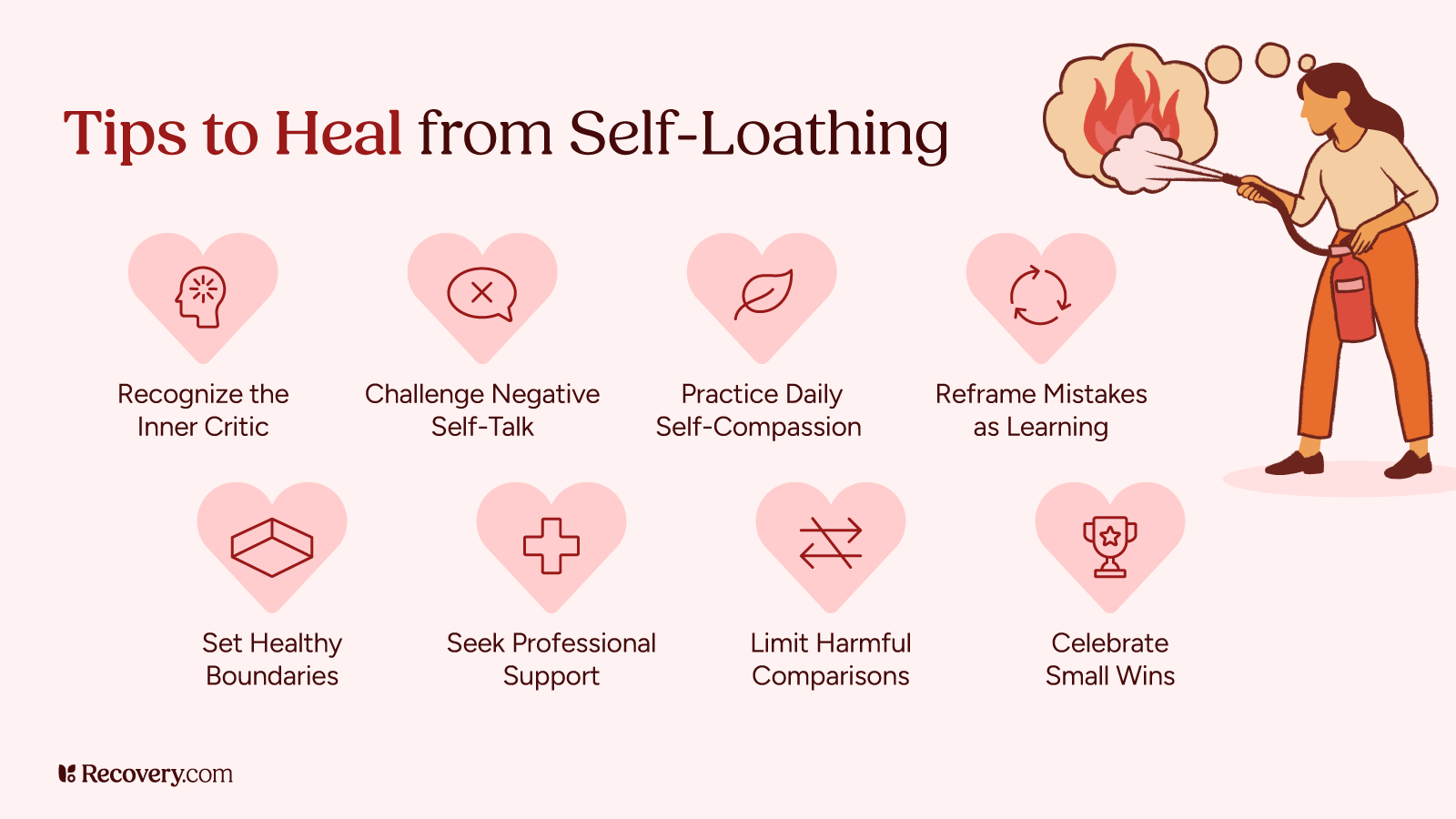
How to Break the Cycle
Self-sabotage is sticky because it’s often unconscious, but the good news is you can overcome self-sabotage. The key is learning to recognize it, approach it with compassion, and slowly replace it with more aligned behaviors.
Strategies To Help You Stop Self-Sabotaging:
- Build Awareness: Start by noticing your self-sabotaging patterns and doing some self-research. Take note: When do they tend to show up? What thoughts or feelings come with them? Journaling or working with a therapist can help make these patterns visible. Don’t be afraid to look up some books5 and resources on self-sabotage too!
- Identify the Underlying Belief: What fear or belief is underneath the behavior? (e.g., “If I try and fail, I’ll prove I’m not good enough.”) Naming this belief is a powerful step toward challenging it.
- Practice Self-Compassion: You’re not doing this to hurt yourself—you’re trying to protect yourself. Speak to yourself gently and have self-compassion.6 Ask: What do I need right now? Or What part of me is trying to help right now, even if it’s doing so in a harmful way?
- Set Small, Sustainable Goals: When fear or overwhelm kicks in, large goals can feel paralyzing. It can help to break things down and tackle them in your own way through creating SMART goals.7 Celebrate progress, not perfection.
- Work With a Professional: Psychotherapy can help uncover the roots of self-sabotage and create space for healing, especially if trauma or deep-seated self-worth issues are involved. Cognitive Behavioral Therapy can also be helpful to aid you with reframing your self-sabotage thinking patterns.
Self-sabotage can feel like an invisible barrier between you and the life you want—but it isn’t permanent. These behaviors often start as coping tools and can be unlearned with patience, support, and self-awareness. When you start to notice what’s driving your actions and gently challenge the beliefs that no longer serve you, change becomes possible. You don’t need to have it all figured out. Growth happens when you take steady, honest steps toward the life you want—without punishing yourself along the way.
If you’re ready to stop getting in your own way, consider working with a trauma-informed therapist or treatment program that can help you understand the roots of self-sabotage—and build a healthier, more supportive path forward.
FAQs
Q: What mental disorder is self-sabotage?
A: Self-sabotage is not a mental disorder in itself, but it can be a symptom or behavior pattern associated with several mental health conditions. These include depression, anxiety disorders, borderline personality disorder (BPD), post-traumatic stress disorder (PTSD), and attention-deficit/hyperactivity disorder (ADHD). It can also occur in individuals without a diagnosable condition, often as a learned coping strategy or result of unresolved emotional wounds.
Q: What is the meaning of self-sabotaging behavior?
A: Self-sabotaging behavior refers to actions (or inactions) that undermine your own success, well-being, or goals. These behaviors often emerge from unconscious fears, low self-esteem, or internalized beliefs that you’re unworthy of happiness or success. Even when the intention is to protect yourself from disappointment or failure, the result is usually increased frustration, regret, and emotional pain.
Q: How can therapy help with self-sabotaging behaviors?
A: Therapy helps by identifying the roots of self-sabotage—such as fear, trauma, or limiting beliefs—and providing tools to change those patterns. A therapist can help you increase self-awareness, challenge negative self-talk, and develop healthier coping strategies. In trauma-informed or cognitive-behavioral approaches, therapy also offers a safe space to build self-compassion and practice new ways of relating to yourself and your goals.
Q: Why do people engage in self-sabotaging behaviors?
A: People self-sabotage for a variety of reasons, most of which are rooted in fear, shame, or self-protection. Common motivations include:
- Fear of failure or success
- Low self-worth or imposter syndrome
- Desire to stay in control of outcomes
- Learned patterns from childhood or past trauma
- Difficulty tolerating positive emotions or vulnerability
Q: Can self-sabotage affect my relationships?
A: Yes, self-sabotaging behaviors can significantly impact relationships. This might look like pushing people away when things feel too close, codependency, testing boundaries, being overly critical, or avoiding conflict until it explodes. People may unconsciously sabotage healthy connections due to fears of rejection, abandonment, or being “too much.” Over time, these patterns can create instability, miscommunication, or emotional distance. There is help available for you and your loved ones. Family therapy may be a beneficial treatment option to explore.