Self-medication is the use of drugs or alcohol as a coping strategy. In many cultures, this behavior is normalized. Phrases like “take the edge off” or “drown your sorrows” downplay the seriousness of self-medicating. It can quickly escalate to substance abuse. Recognizing the signs of self-medicating and getting treatment early on are key to avoiding addiction and keeping your life on track.
Self-Medication Explained
Self-medication is the use of substances, like drugs and alcohol, to cope with mental or emotional distress. It also includes taking prescription drugs without medical supervision.
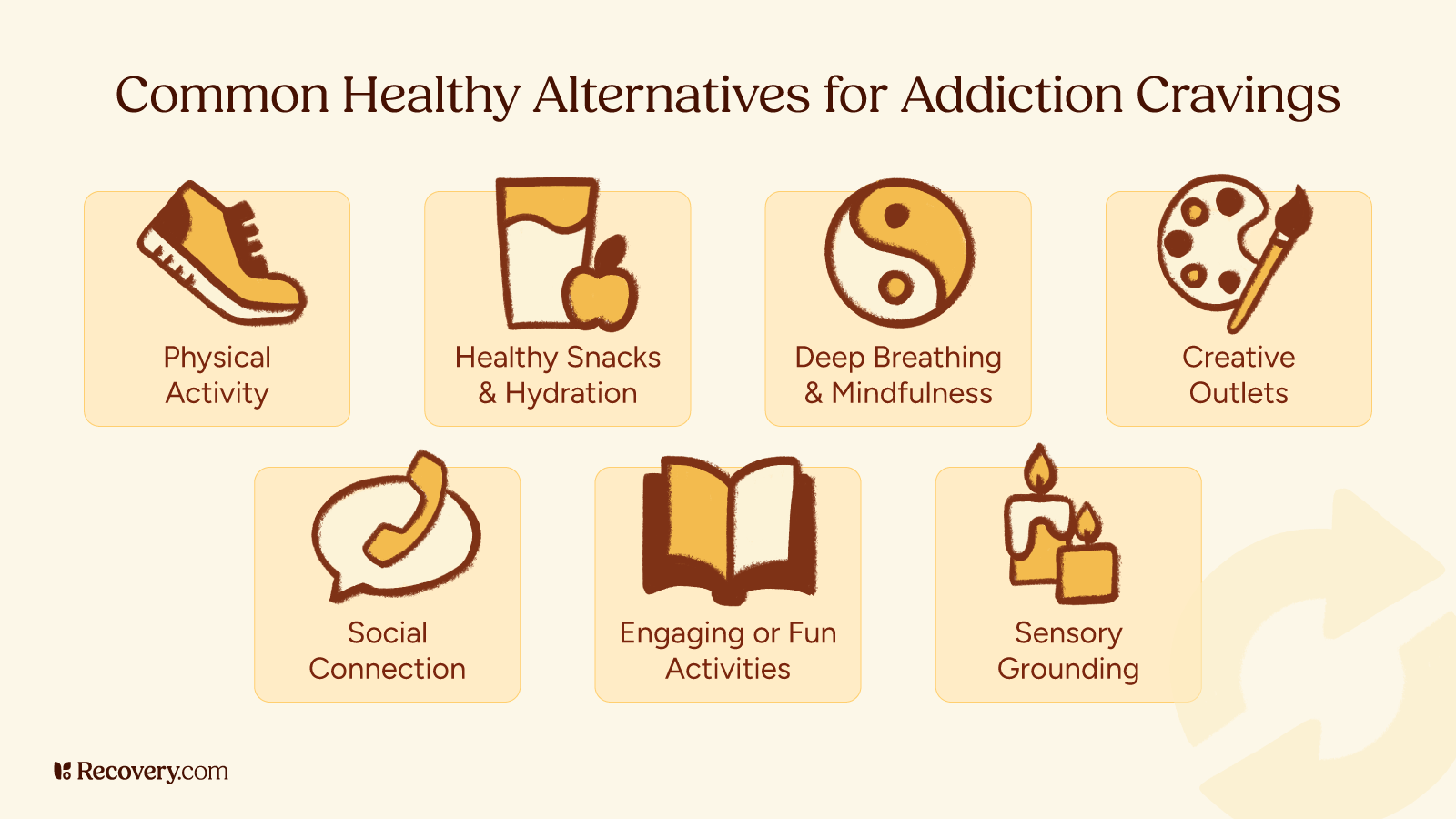
Everyone experiences stress, difficult emotions, or challenging situations, but it’s important to learn how to manage them in ways that don’t cause further harm. Unhealthy coping strategies include anything that negatively impacts your mental or physical health. That includes substance use.
Using substances to feel better may offer temporary relief, but it carries harmful risks. Self-medication often develops into a substance use disorder.1 It’s also very common. One study showed that up to 24.1% of people with mood disorders used drugs or alcohol to cope.
To prevent this from happening to you, watch for these warning signs:
1. Using Substances to Cope With Your Emotions
Using substances to deal with stress, anxiety may not seem harmful at first, especially when it’s so normalized. In many countries, using alcohol to manage burnout and stress is common. However, alcohol is a drug, just like any other substance. And suppressing emotions with substances only prolongs the issue and prevents you from growing your emotional resilience.
Unresolved stress is linked to increasing substance use2 over time. Increasing your substance intake causes you to build tolerance. And when that happens, your body requires more of a substance to feel the same effects as before. Tolerance is a sign that you’re heading toward addiction.3 While substances offer temporary relief, ultimately, they only make problems worse.
2. Escaping Reality: Isolating and Avoiding Problems
Someone who is self-medicating uses substances to detach from everyday life. This can look like neglecting responsibilities, isolating, and emotionally numbing.
Ignoring responsibilities is a sign that substances are taking priority over other areas of life. Teens with addiction tend to miss school4 and other important milestones. Adults might miss deadlines, or not show up for work. In the long run, these decisions impact career prospects and increase financial stress.
Substance abuse fuels isolation.5 You might withdraw from social events or distance yourself from your support network. And social withdrawal makes mental health issues worse. Too much social isolation leads to anxiety6 and depression, and increases the risk of heart disease and dementia.
When emotional pain becomes too much to bear, it’s natural to want to escape it—and substances present an easy way to feel better. If you slip into this behavior, it doesn’t mean you’re broken; it means you’re human.
Being able to recognize when this is happening is a great first step towards healing. Fortunately, you have several avenues for recovery, from individual therapy to residential rehab.
3. Mood Swings and Emotional Instability
Emotional instability and self-medication feed into each other. Some people self-medicate to avoid difficult emotions, making it hard to process them healthily. Substances also alter your brain chemistry and affect areas that play a role in mood regulation. For example, drugs and alcohol decrease levels of GABA,7 a brain chemical that helps you stay calm.
Mood swings are sudden mood changes that vary in intensity and duration:
- Increased irritability
- Hyperactivity
- Angry outbursts
- Paranoia or anxiety with no apparent cause
- Unusual giddiness
- Strong reactions to minor stressors
A long-term effect of self-medicating includes substance-induced mood disorder,8 in which someone develops depressive, anxious, psychotic, or manic symptoms as a result of substance use. Another long-term symptom is emotional dependence, or relying on substances to feel “normal.”
4. Changes in Routine and Priorities
Changes in routine and priorities are worrying signs of self-medication. These can look different for different people:
- A teen might prioritize substances over school.
- An employee might be far less productive than usual, or miss work.
- A spouse might lose interest in spending time with their loved one.
Several factors cause these changes. Substances interfere with the brain’s dopamine-based reward system, reducing your ability to feel pleasure. That’s why when you’re depressed, things you normally enjoy may no longer interest you at all.
These changes to the brain’s reward system can cause cravings.9 And cravings have a powerful impact on priorities, making it hard to focus on anything else. When this happens, important responsibilities—even relationships—take a back seat. You might start changing your daily routine to accommodate substance use.
5. Decline in Health and Physical Well-Being
A dip in your physical health indicates that self-medicating has become a problem. Substance abuse takes a toll on the body.10 Because these issues aren’t always noticeable at the surface level, they’re often overlooked. For example, self-medicating with alcohol over a few years impairs your liver’s ability to regenerate. While it might not be apparent for some time, long-term drinking causes permanent liver damage.11 This is generally irreversible and reduces life expectancy.
There are other, more immediate health concerns related to substance use:
- Unexplained health problems, such as fatigue or pain
- Weight fluctuations
- Engaging in risky sexual behavior or other decisions that jeopardize your health
- Missing doctor visits due to substance use
Physical and mental health depend on each other. It’s hard to treat one without addressing the other. That’s why many mental health treatment programs also focus on physical wellness, with options like nutrition therapy, personal training, yoga, and more.
6. Relationship Strain and Isolation
When self-medicating becomes a go-to coping mechanism, it shakes the foundation of our relationships. You might notice rifts between you and the people in your life. Conflicts with loved ones due to substance use12 are a common experience. They arise for a number of reasons:
- Drugs and alcohol impair your judgment, making it hard to maintain healthy dynamics.
- Long-term substance abuse can lead to mood and personality changes.
- You may prioritize drugs or alcohol over relationships and spend less time with others.
- You might act in ways that erode trust.
- Addiction leads to financial and legal issues, putting further strain on relationships.
Self-medicating can be isolating—loneliness is typical among people with who regularly use substances. In one study, up to 71% of people with substance use problems reported feeling lonely.13 If you’re struggling with isolation, remember that you have options for support. You can confide in a therapist, find community in support groups, or seek solace in group therapy.
7. Decline in Work or School Performance
A decline in work or school performance is an indicator of self-medication. Some people show a sharp drop in performance, while others decline more gradually (such as with high-functioning alcoholism). While it may seem like you can keep up appearances, this lifestyle isn’t sustainable. It’s a sign of shifting priorities. In the U.S. alone, alcohol use disorder is linked to 232 million missed workdays14 per year.
Poor work performance can lead to job loss, heightening stress and anxiety.
A Path to Healing: Find Professional Help for Self-Medication
If self-medicating is how you cope with life’s challenges, you’re likely doing yourself more harm than good.
Thankfully, there are plenty of healthier ways to cope, and various avenues for learning them. If you’re ready for support, you can explore treatment options and compare providers based on what they treat, price, insurance accepted, and more.
Frequently Asked Questions About Self-Medicating With Substances
What are the signs of self-medicating with drugs or alcohol?
– Using substances to cope with stress, anxiety, or other emotions
– Escaping reality, isolating, and avoiding problems
– Mood swings and emotional instability
– Changes in routine and priorities
– Decline in health and physical well-being
– Relationship strain and isolation
– Decline in work or school performance
What are the risks of self-medicating with drugs or alcohol?
– Addiction
– Mood disorders
– Social problems, such as relationship strains, job loss, and financial issues
– Difficulty managing emotions in a healthy way
– Building tolerance to drugs or alcohol