Xanax, a prescription medication that’s often used to treat anxiety and panic disorders, can Xanax, a prescription medication that’s often used to treat anxiety and panic disorders, can be a helpful tool when you use it responsibly under medical supervision. But its potential for misuse and addiction raises concerns among healthcare providers and those looking for solutions for acute anxiety.
We explore what Xanax is, how and why people use it incorrectly, and the addiction risks involved—plus treatment options for those seeking help.
What Is Xanax?
Xanax (the brand name for alprazolam)1 is a medication that’s part of the benzodiazepine family. It’s often prescribed to treat anxiety disorders because it helps calm the mind and body.
It’s usually prescribed by medical professionals who are licensed to evaluate and treat conditions like anxiety and panic disorders. These include primary care physicians, psychiatrists, nurse practitioners, addiction medicine specialists, and pain management specialists.
Because Xanax has a high potential for abuse, prescribers are cautious about certain risk factors:
- Any history of substance use disorders
- Monitoring for signs of dependency
- Encouraging therapy or other non-benzodiazepine strategies for long-term management
It’s best to take Xanax as part of a medication management plan under the guidance of a qualified behavioral health professional.
How Xanax Affects the Brain
Xanax works by boosting the effects of GABA,2 a neurotransmitter that slows down nerve signals in the brain. GABA acts like the brain’s natural brake pedal, helping you feel calm and relaxed. By boosting GABA activity, Xanax reduces symptoms of anxiety, helps with sleep, and creates feelings of relaxation.
The medication is fast-acting, which makes it especially effective for acute anxiety episodes. However, this quick action also contributes to its addiction potential—even with short-term use.
Why Do People Misuse Xanax?
Xanax use often begins with a desire for relief from stress, insomnia, or emotional distress. But whether or not they have a prescription, people misuse Xanax for a lot of reasons. Some might take more than prescribed to feel calmer. Others may use it recreationally for the sense of relaxation or euphoria it can provide.
Sometimes, people combine Xanax with other substances, like alcohol, to intensify the effects—which can be extremely dangerous. Misuse often starts because of:
- Stress relief – People often self-medicate to cope with anxiety, stress, or their inability to sleep.
- Tolerance – Over time, the body gets used to Xanax, so people need higher doses to get the same effect.
- Fear of withdrawal – Xanax can cause uncomfortable withdrawal symptoms. This causes many people to keep taking it even when they want to stop.
The National Institutes of Health (NIH) explains:
Alprazolam may be habit forming.3 Do not take a larger dose, take it more often, or for a longer time than your doctor tells you to. Tell your doctor if you have ever drunk large amounts of alcohol, if you use or have ever used street drugs, or have overused prescription medications. Do not drink alcohol or use street drugs during your treatment. Drinking alcohol or using street drugs during your treatment with alprazolam also increases the risk that you will experience these serious, life-threatening side effects. Also tell your doctor if you have or have ever had depression or another mental illness.
How Is Xanax Abused?
People abuse Xanax in a number of ways, including:
- Taking higher doses than prescribed
- Taking it more frequently than prescribed
- Using it without a prescription
- Crushing and snorting pills to feel the desired effects more quickly
- Combining Xanax with other substances like alcohol or opioids to heighten its effects (a dangerous practice that significantly increases the risk of overdose)
Taking Xanax in ways other than prescribed or mixing it with other substances can have unpredictable and potentially life-threatening consequences.
The Scope of the Problem: Xanax Misuse by the Numbers
Xanax misuse isn’t rare. In fact, it’s a growing problem:
- Nearly 12.5% of U.S. adults use benzodiazepines4 like Xanax, and about 17% of them misuse these medications.
- About 30% of opioid overdose deaths also involve benzodiazepines5 like Xanax.
- Benzos are involved in over 200,000 emergency room visits annually.6 Over half of these are from nonmedical use.
These numbers show just how serious Xanax misuse has become—and why it’s so important to understand the risks.
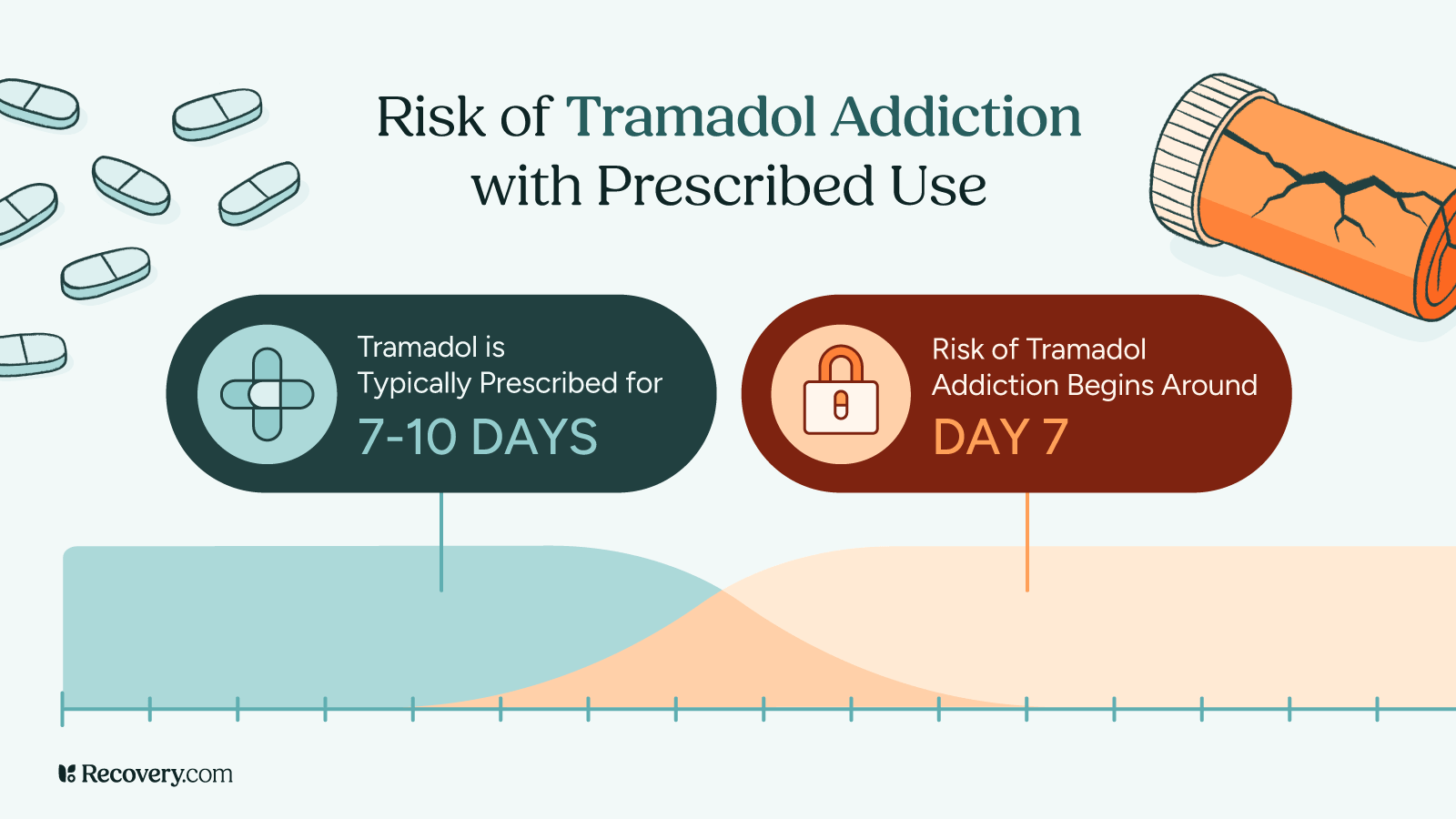
How Addictive Is Xanax?
Xanax is highly addictive,7 especially when compared to other prescription drugs. Its effects are strong and fast, which makes it more likely for people to develop a dependency. This can happen over even a short period of time. Compared to antidepressants like Zoloft, which work gradually over weeks and have lower drug addiction potential, the effects of Xanax are stronger and more immediate, which can lead to psychological dependence much faster.
The NIH explains how Xanax dependence sets in:
Alprazolam may cause a physical dependence (a condition in which unpleasant physical symptoms occur if a medication is suddenly stopped or taken in smaller doses), especially if you take it for several days to several weeks.
What makes Xanax so addictive?
- Short-lasting effects: Xanax works quickly but wears off fast, which can make you want more.
- Feel-good effects: The sense of calm it provides can be hard to give up, especially if the cause of your anxiety persists.
- Tolerance: As your body adjusts, you might want to take larger doses, which increases your risk of addiction.
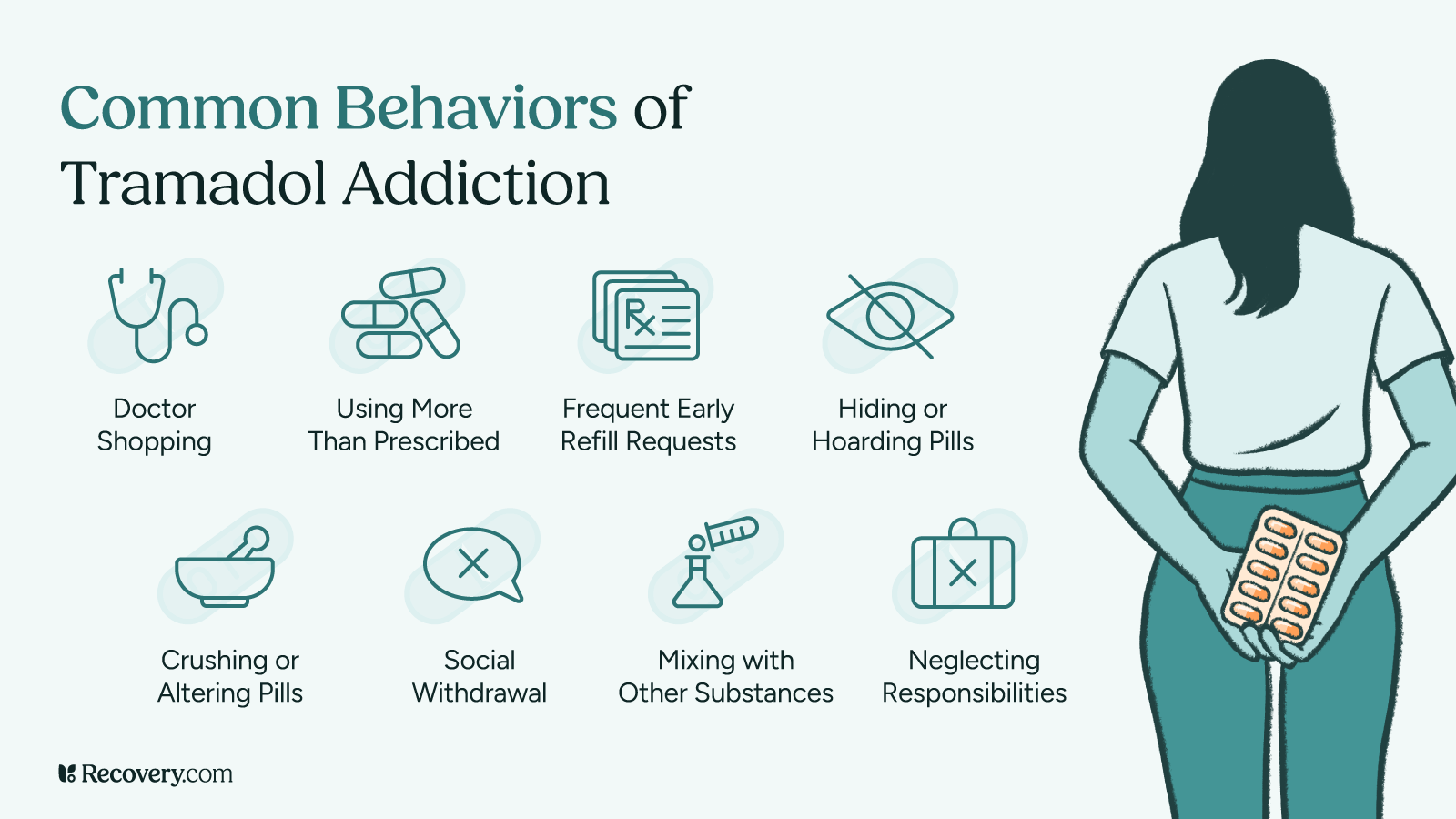
Signs of Xanax Addiction
If you’re worried about your relationship with Xanax, look for these warning signs:
Behavioral Indicators
- Taking more Xanax than you were prescribed or using it without a prescription
- Seeing multiple doctors to get extra prescriptions (a practice called “doctor shopping”)
- Avoiding your responsibilities at work, school, or home
- Acting secretive or withdrawing from your social circle
Physical Symptoms
- Constant drowsiness or feeling sedated
- Slurred speech or trouble staying balanced
- Constantly feeling tired or weak
- Muscle aches and tremors
Psychological Effects
- Feeling anxious, irritable, or panicked when you don’t have Xanax
- Trouble concentrating or memory lapses
- Depression or mood swings
- Craving Xanax even when you know it’s causing problems in your life
Risks of Xanax Misuse and Addiction
The use of Xanax doesn’t just put you at risk for addiction—it can also seriously affect your physical and mental health.
Xanax Overdose
Xanax slows down your central nervous system,8 which controls vital functions like breathing and heart rate. Taking too much—or mixing it with other substances like alcohol—can cause your breathing to slow to dangerous levels. This respiratory depression is the main cause of fatal overdose.
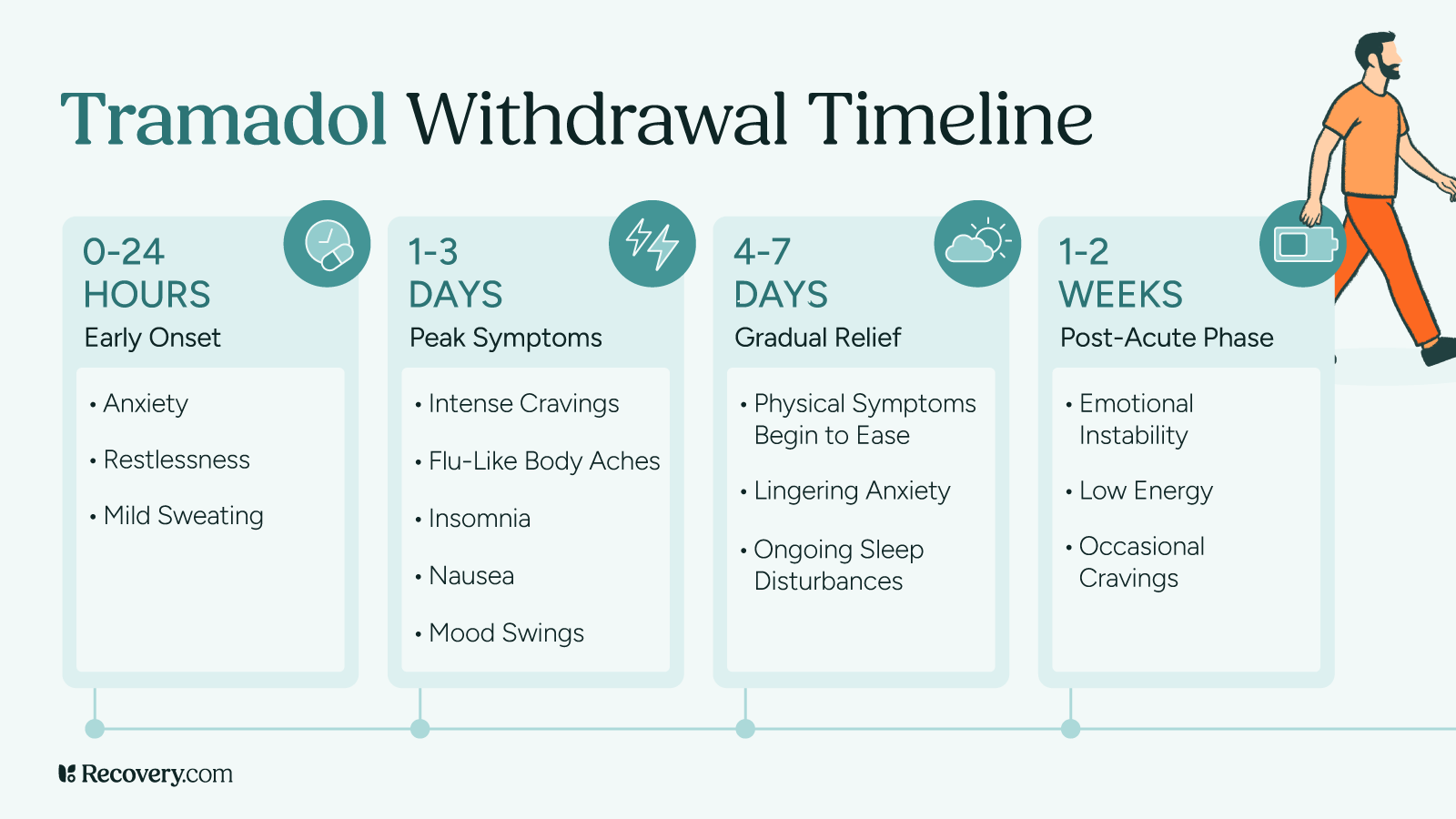
Withdrawals
If you’re dependent on Xanax, stopping suddenly is dangerous. It can cause severe withdrawal symptoms that include seizures, panic attacks, and insomnia. Quitting “cold turkey” without medical help is risky—it’s hugely important to taper off under a doctor’s supervision.
The NIH warns:
Do not stop taking this medication or take fewer doses without talking to your doctor. Stopping alprazolam suddenly can worsen your condition and cause withdrawal symptoms that may last for several weeks to more than 12 months. Your doctor probably will decrease your alprazolam dose gradually. Call your doctor or get emergency medical treatment if you experience any of the following symptoms: unusual movements; ringing in your ears; anxiety; memory problems; difficulty concentrating; sleep problems; seizures; shaking; muscle twitching; changes in mental health; depression; burning or prickling feeling in hands, arms, legs or feet; seeing or hearing things that others do not see or hear; thoughts of harming or killing yourself or others; overexcitement; or losing touch with reality.
Not all doctors are trained in addiction-related care. It’s important to get professional help from a prescriber who has experience helping patients taper off benzodiazepines.
Long-Term Health Consequences
Prolonged Xanax abuse can lead to:
- Memory and focus problems: Over time, Xanax leads to cognitive impairment in areas like concentration and recall.
- Physical dependence: Your body can become so reliant on Xanax that it’s hard to function without it.
- Emotional instability: Xanax misuse can worsen anxiety,9 depression, or other mental health conditions over time.
How Can I Help Someone Struggling With Xanax Addiction?
If someone you care about is struggling with Xanax addiction, your support can make a major difference in their recovery journey.
Start by approaching them with compassion rather than judgment or blame. Express your concerns calmly and offer your support. When you’re ready to have a conversation, encourage them to speak with a therapist or addiction specialist. You can offer to help them look into treatment options or even go with them to appointments.
Take time to learn about addiction yourself. Understanding how Xanax addiction works can help you provide better support and set realistic expectations for recovery. It’s also hugely important to take care of your own wellness— supporting someone with addiction is emotionally draining. You can also join a support group for loved ones of people with substance use disorders.
While you can’t force someone to get help, you can create an environment that supports their recovery.
If you’re ready to have this important conversation, learn effective strategies and find the right words in our guide to talking to a loved one about going to rehab.
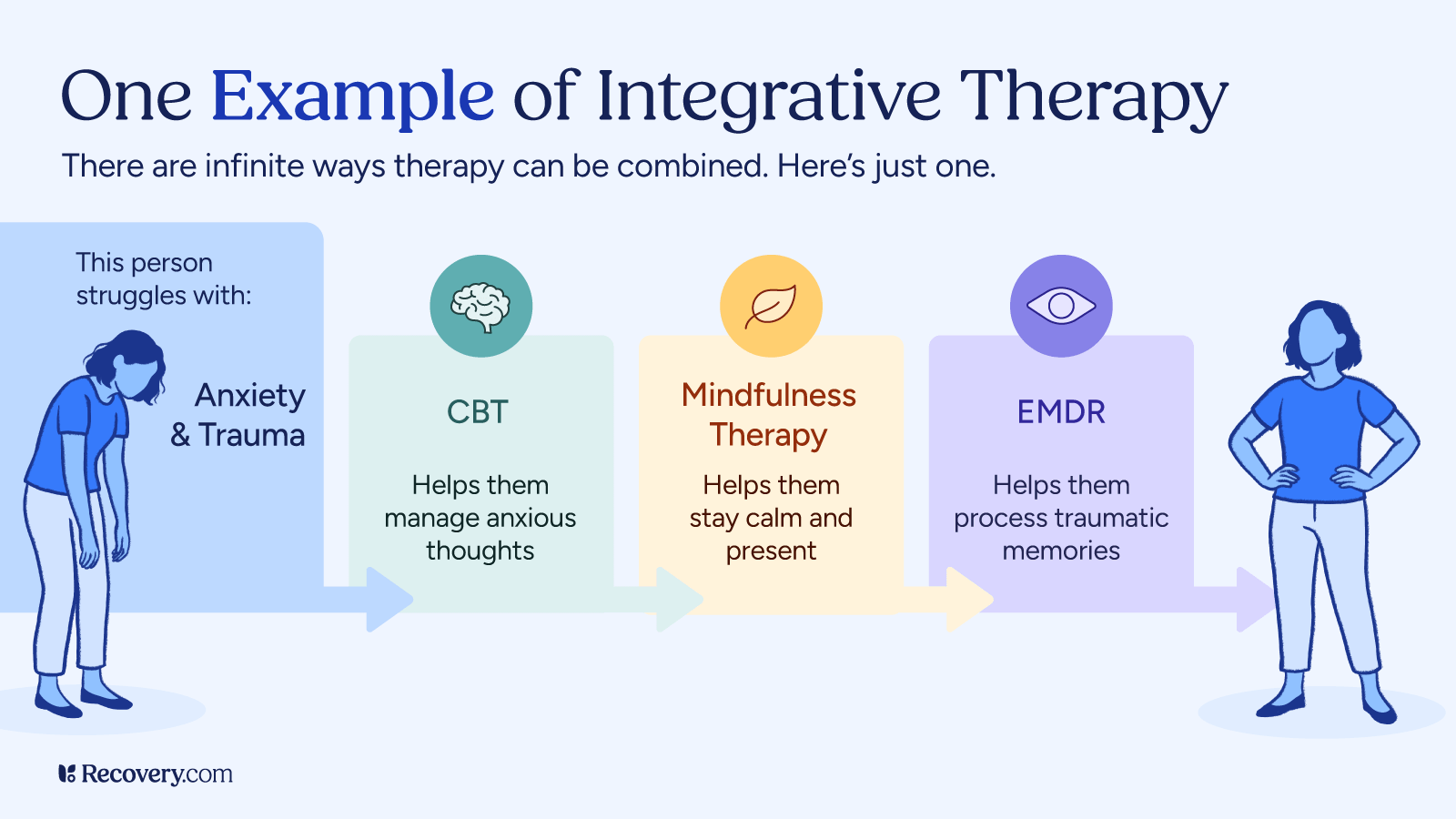
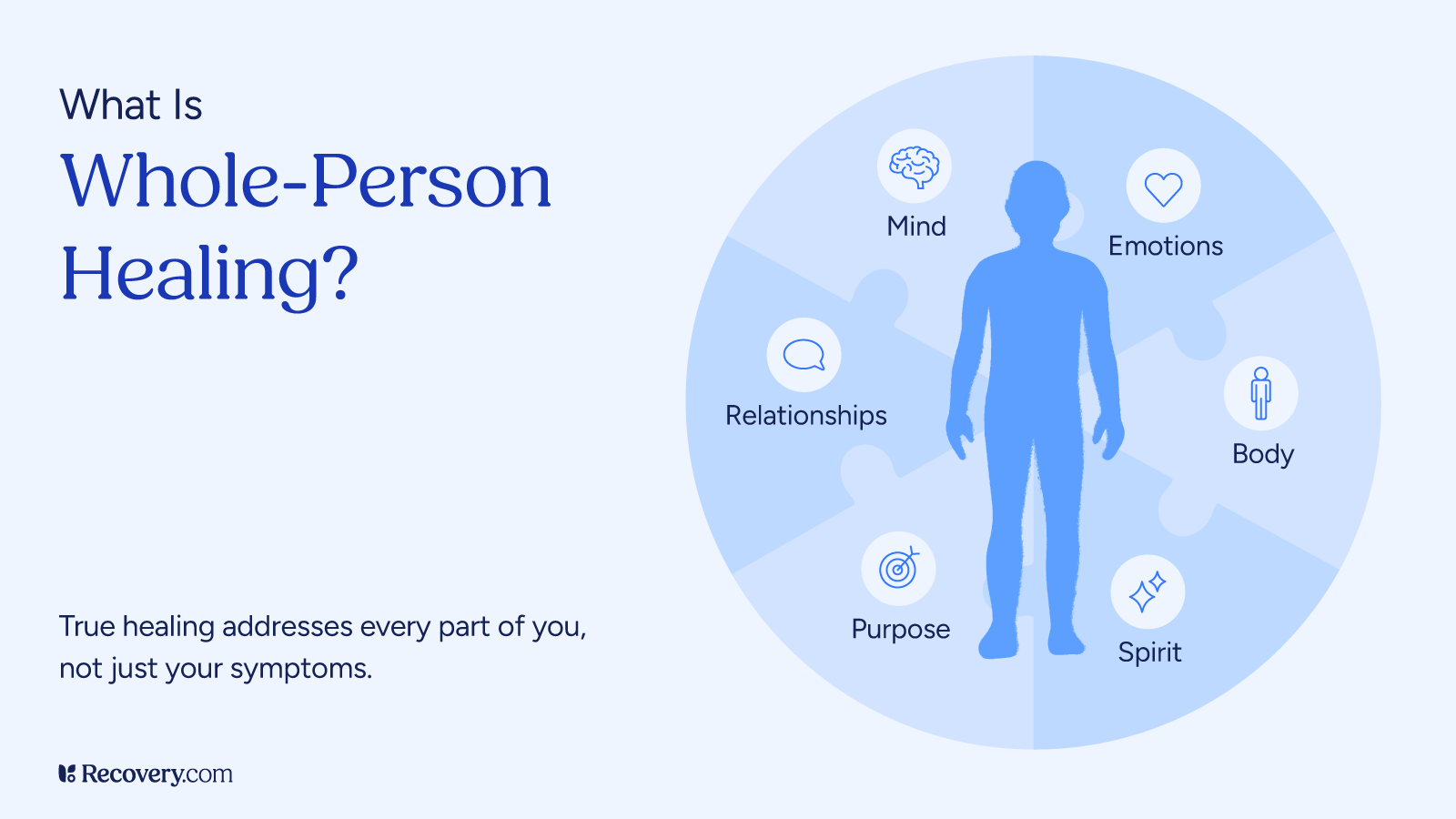
Treatment for Xanax Addiction
The good news is that Xanax addiction is treatable, and there are plenty of resources to help you recover. Effective treatment for Xanax addiction usually involves a combination of medical intervention, evidence-based and complementary therapies, and ongoing support.
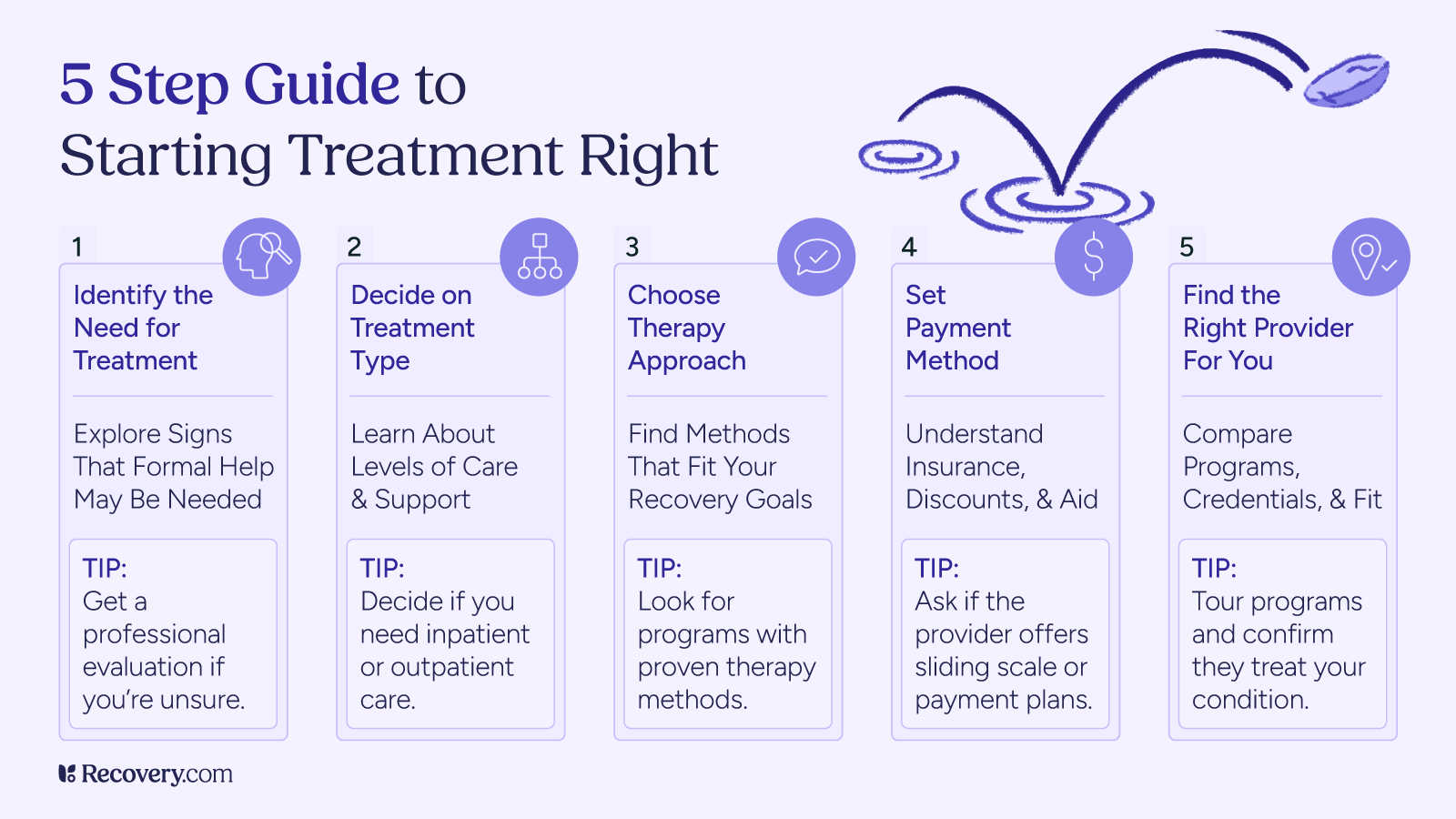
Detox
The first step is detoxification, where the body gets rid of Xanax. Because withdrawal can be intense, it’s important to do this under medical supervision. Usually, your doctor will taper the dose slowly to make the process safer and more manageable.
Medication-Assisted Treatment (MAT)
In some cases, your doctor might prescribe other medications to manage withdrawal symptoms or address co-occurring mental health issues.
Comprehensive Xanax Addiction Treatment Programs
Inpatient rehab programs provide 24/7 medical supervision and intensive therapy in a controlled environment. These programs typically last 30–90 days and are ideal for people with more severe addiction or those who feel they can benefit from a more immersive treatment experience. You’ll participate in individual counseling, group therapy, and behavioral therapies that help you identify and change the patterns that lead to misuse.
Outpatient rehab programs allow you to continue living at home while attending scheduled treatment sessions. These programs offer flexibility for people who have work or family responsibilities but still need structured support. Outpatient treatment includes individual counseling to work through personal struggles related to addiction, group therapy for peer support, and educational sessions about addiction and recovery strategies.
When you start rehab, your care team will do a thorough assessment and create a treatment plan according to your needs.
Aftercare and Ongoing Support
Continuing care is important to maintain your recovery progress after you complete initial treatment. This ongoing support includes regular therapy sessions to reinforce coping strategies and address any emerging challenges. Many people find support groups like Narcotics Anonymous (NA) or SMART Recovery helpful for connecting with others in recovery. Lifestyle changes such as developing healthy stress management techniques, establishing regular sleep patterns, and building a strong support network are also important aspects of preventing relapse and maintaining sobriety.
Long-term recovery often involves a combination of continuing care approaches, such as:
- Regular check-ins with your healthcare provider
- Outpatient addiction treatment
- Ongoing individual therapy
- Support groups like Narcotics Anonymous (NA)
Find a Treatment Center
If you want to stop using Xanax but are having a hard time doing so on your own, finding the right treatment facility is a great step toward recovering safely and effectively.
Rehabs offer personalized addiction treatment programs that are tailored to your needs. They provide a combination of therapies to address underlying issues, and resources for long-term recovery. Many also have medical detox facilities on-site, or can help you arrange detox prior to starting treatment.
Explore benzodiazepine addiction treatment options to find a facility near you.
FAQs
Q: What makes Xanax so addictive?
A: Xanax is highly addictive due to its fast-acting, short-lasting effects, which can create a cycle of dependency. Over time, as tolerance builds, people often feel they need higher doses for the same relief. This increases the risk of benzodiazepine addiction, especially if you’re taking Xanax without medical supervision.
Q: How can Xanax withdrawal be managed safely?
A: Xanax withdrawal should always be managed under medical supervision. Gradual tapering, as directed by a healthcare provider, reduces the risk of severe symptoms like seizures, panic attacks, or insomnia. Detox programs also offer safe and effective support.
Q: What are the risks of mixing Xanax with alcohol?
A: Mixing Xanax with alcohol can severely depress the central nervous system, leading to slowed breathing, impaired coordination, and increased risk of overdose. This combination is extremely dangerous and should always be avoided.
Q: What are the withdrawal symptoms of alprazolam?
A: Xanax withdrawal symptoms can range from mild to severe and may include:
- Anxiety and panic attacks
- Insomnia and sleep disturbances
- Tremors and muscle twitching
- Sweating and hot flashes
- Nausea and vomiting
- Headaches
- Difficulty concentrating
- Memory problems
- Seizures (in severe cases)
- Depression and mood changes
- Sensitivity to light and sound
Withdrawal symptoms can last from a few weeks to more than 12 months, depending on factors like dosage and length of use.
Q: Is Xanax more addictive than Zoloft?
A: Yes, Xanax is significantly more addictive than Zoloft.10 Xanax belongs to the benzodiazepine class and produces immediate calming effects, making it highly habit-forming. Zoloft is an antidepressant (SSRI) that works gradually over several weeks and has a much lower addiction potential. While some people may experience withdrawal symptoms when stopping Zoloft, it doesn’t create the same physical dependence and craving patterns as Xanax.