Luxury weight loss spas offer a unique and holistic approach to managing weight while prioritizing overall wellness. These retreats combine personalized fitness programs, expert nutritional guidance, and cutting-edge therapies in luxurious settings, helping guests achieve sustainable weight loss.
Beyond the physical benefits, luxury weight loss spas support mental and emotional well-being by incorporating mindfulness practices like yoga, meditation, and stress relief techniques. The serene, high-end environments can provide a peaceful escape from daily life, allowing guests to focus entirely on their health and transformation in comfort and luxury.
Here are some of the best weight loss spas around the world.
Euphoria Retreat
Greece

Euphoria Retreat, located in the heart of the Peloponnese in Greece, offers a unique wellness experience that blends ancient Greek and Chinese healing philosophies within a luxurious and tranquil setting. Nestled in Mystras, a UNESCO-listed town, the retreat is renowned for its state-of-the-art spa facilities, which include a 4-story wellness center featuring saunas, a cold plunge pool, and hydrotherapy options. Guests can indulge in an array of treatments that prioritize holistic well-being, such as Kneipp water therapy, aromatherapy, and hot stone massages.
Euphoria Retreats’ approach integrates physical fitness and mindfulness with activities like yoga, pilates, hiking, and meditation. These are complemented by tailored wellness programs, including detox services, weight management, and emotional balance retreats. The on-site restaurant serves nutritious Mediterranean cuisine that detoxes and boosts energy.
Chiva-Som
Thailand

Set on the beautiful beaches of Hua Hin, Thailand, Chiva-Som is a luxury wellness retreat that offers a holistic and integrative approach to health and well-being. The program combines Eastern and Western therapies with customized wellness programs designed to meet individual health goals, including detox, weight management, fitness, and stress relief. The retreat offers over 200 treatment options, including traditional Thai therapies, advanced physiotherapy, acupuncture, and spa treatments. Chiva-Som focuses on mind-body balance through various activities, such as yoga, meditation, Tai Chi, and fitness training.
Chiva-Som crafts personalized wellness journeys, where guests undergo consultations with health professionals to develop tailored plans based on their specific needs. The serene surroundings, luxurious accommodations, and wellness offerings all create a transformative experience for guests.
Golden Door
USA

Golden Door is a luxury wellness retreat in San Marcos, California that offers a truly personalized and immersive experience aimed at rejuvenating the body, mind, and spirit. Set on over 600 acres of private land, it includes 30 miles of exclusive hiking trails, biodynamic gardens, and serene natural surroundings. Each guest enjoys a custom wellness plan tailored to their goals, including daily spa treatments, fitness classes, and nutritious farm-to-table meals sourced from their own organic farms. The intimate setting, accommodating only 40 guests at a time, provides a highly personalized experience with a 4:1 staff-to-guest ratio.
The wellness journey at Golden Door is deeply holistic, focusing on physical fitness, mental clarity, and spiritual healing. Offerings range from yoga, pilates, and meditation to more adventurous activities like archery. The retreat also integrates mindfulness practices and personal empowerment workshops, making it a transformative experience for those seeking a fresh start, relaxation, or recovery from life’s challenges.
SHA Wellness Clinic
Spain

Tucked away in serene Alicante, Spain with stunning ocean views, SHA Wellness Clinic is a unique wellness retreat that combines modern medicine with natural therapies, drawing from both Eastern and Western practices. The SHA Method is a holistic approach focused on improving long-term well-being through personalized health programs that are tailored to address a wide array of needs, such as weight management, fitness, stress relief, and anti-aging.
The clinic utilizes cutting-edge medical treatments alongside holistic therapies like genetic testing, hydrotherapy, and acupuncture. Its Integrative Health Programs are designed to help guests achieve optimal health by blending medical expertise, nutrition, physical activity, and relaxation techniques.
Clinique La Prairie
Switzerland

Clinique La Prairie, located on the shores of Lake Geneva in Montreux, Switzerland, is a world-renowned luxury retreat known for its innovative approach to health and longevity. Established in 1931, it combines cutting-edge medical science with holistic therapies, offering a unique and personalized approach to wellness.
The retreat’s Revitalization Program is based on a unique cell therapy that is integrated into a broader philosophy that blends preventive medicine, longevity research, and natural wellness practices. The clinic emphasizes personalized care, offering tailor-made health programs that address various needs such as detox, stress management, weight loss, and anti-aging. Guests benefit from access to leading specialists, advanced diagnostic technologies, and a luxurious spa experience.
In addition to its health programs, Clinique La Prairie is renowned for its tranquil location with views of the Alps and Lake Geneva, luxurious accommodations, and Michelin-starred dining focused on balanced, nutritious meals.
VIVAMAYR
Austria

VIVAMAYR is known for its unique fusion of modern medicine and traditional healing practices based on the Mayr Cure, a detoxification method developed by Dr. Franz Xaver Mayr. Located in Austria, VIVAMAYR’s programs focus on improving gut health and overall well-being through personalized medical diagnostics, nutrition plans, and holistic therapies.
The retreat offers various health programs tailored to individual needs, such as weight and stress management. They believe that gut health is key to overall health, so VIVAMAYR integrates cutting-edge medical treatments with lifestyle coaching, therapeutic fasting, and mindful eating practices. The retreat combines advanced diagnostic tools with therapies like hydrotherapy, massage, and tailored fitness programs, all set in a tranquil environment, offering a holistic path to lifelong wellness.
Preidlhof
Italy
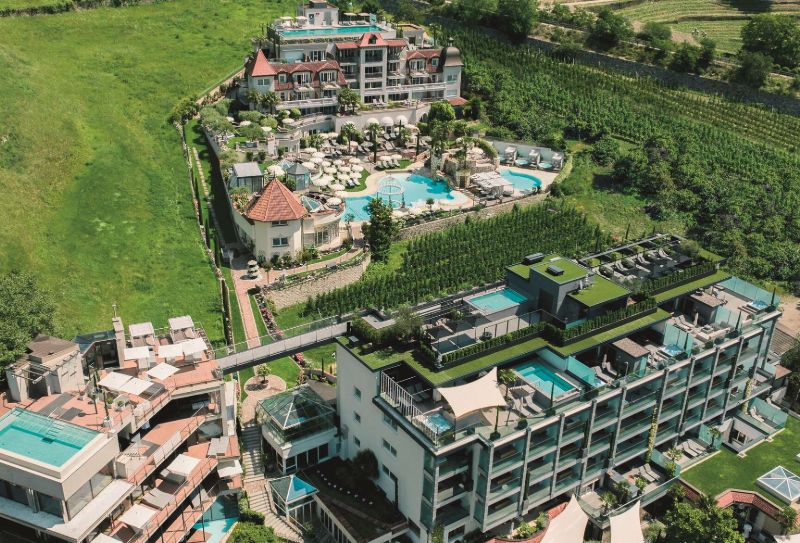
Preidlhof, located in South Tyrol, Italy, is a luxurious retreat renowned for its comprehensive approach to well-being, combining relaxation, medical spa treatments, and holistic healing. With the serene backdrop of the Italian Alps, Preidlhof’s attention to personalized care, innovative treatments, and unique location combine to create a wellness retreat that offers both luxury and rejuvenation .
Preidlhof’s 6-floor spa includes saunas, steam rooms, pools, and panoramic relaxation areas, providing a unique experience. Guests can indulge in treatments ranging from massages to advanced medical therapies like anti-aging and detox treatments. Preidlhof also offers various holistic wellness programs that integrate mindfulness, nutrition, and fitness, making it a destination for those seeking a transformative health experience.
Absolute Sanctuary
Thailand

Absolute Sanctuary is a standout wellness retreat located on the island of Koh Samui in Thailand that specializes in fitness, detox, and overall well-being. The facility combines holistic health programs with a luxury resort experience, and it’s particularly renowned for its comprehensive detox programs, yoga retreats, and fitness boot camps, all designed to help guests rejuvenate their body and mind.
The retreat offers an extensive range of wellness facilities, including a top-notch fitness center, yoga studio, detox center, and spa with treatments ranging from massages to specialized therapies like colon hydrotherapy. Its programs are customizable to address specific health goals. Absolute Sanctuary strives to provide healthy cuisine with nutritious, plant-based meals that complement guests’ wellness journeys.
Rancho La Puerta
Mexico

Rancho La Puerta is a pioneering wellness retreat known for its holistic approach to well-being, blending fitness, mindfulness, and nature. Established in 1940 in Baja California, Mexico, it has a rich legacy of promoting health through connection with nature and personal empowerment. The retreat offers an all-inclusive wellness program that provides 80+ fitness classes, therapeutic spa treatments, and workshops aimed at enhancing physical, mental, and spiritual well-being.
Rancho La Puerta’s mission and legacy focus on creating personal transformation and community through an environment where guests can unplug from daily life and focus on lasting well-being. The retreat features an organic farm-to-table dining experience, where meals are sourced from the center’s own gardens to incorporate nutrition as a key part of the wellness journey. Mindfulness is a core value and is utilized through activities such as meditation, yoga, and nature hikes across the 4,000-acre property.
Canyon Ranch
USA

Canyon Ranch in Tucson, Arizona, has an integrative approach to health and well-being, focusing on whole-person wellness and offering customized programs that address physical, mental, emotional, and spiritual health. The resort provides an extensive range of services and experiences, including fitness classes, spa treatments, nutritional guidance, and specialized wellness consultations with medical experts, life coaches, and spiritual advisers.
Set in the Sonoran Desert, Canyon Ranch integrates nature into its wellness offerings with outdoor activities like hiking and biking to take advantage of the desert landscape. The retreat also provides mind-body practices such as yoga, meditation, and mindfulness to complement cutting-edge treatments in their spa and health centers. Canyon Ranch’s holistic wellness approach, personalized care, and immersive desert environment makes it a standout destination for those seeking transformation and renewal.