People often first encounter Adderall through friends, classmates, or coworkers who share their prescription. But what may start as occasional use for studying or meeting deadlines can easily shift into something more concerning—often before you realize what’s happening.
Adderall is a medication for attention-deficit hyperactivity disorder (ADHD) and narcolepsy. But when it’s taken by people without a medical need for it, whether for practical or recreational use, it acts as a strong stimulant. Adderall misuse affects brain chemistry in ways that can lead to dependence—which can make stopping feel hard, even when you want to.
This can happen to anyone. Smart, responsible people find themselves in this situation all the time. If you’re questioning your relationship with Adderall or wanting to make a change, understanding how dependence develops and what your options are for making a change is a great place to start.
Understanding Adderall Dependence
Adderall contains amphetamine and dextroamphetamine,1 which boost dopamine and norepinephrine in your brain: the chemicals behind focus, motivation, and reward. For people with ADHD, this helps balance brain chemistry. But if you don’t have ADHD, it creates an artificial surge that, for some people, feels very appealing.
If you continue taking Adderall, your brain adapts quickly to these changes and starts making less dopamine on its own. Soon, tasks that used to feel normal—like studying, working, or even hanging out with friends—feel much harder.
This shift can happen faster than you’d think. Some people notice that within just weeks, they need higher doses to get the same effect. Others go from “just for big projects” to taking it daily without intending to.
Adderall abuse is especially common among college students and in competitive work environments, where its reputation as a “study drug” makes it seem relatively harmless. Plus, when it’s easy to get from friends or classmates who have prescriptions, it can feel like a safer choice than other stimulants.
But Adderall is a Schedule II controlled substance2 for a reason: It carries real risks for dependence, no matter how you get it or why you’re using it.
Why People Use Adderall Without a Prescription
People don’t usually wake up one day and decide to start taking someone else’s medication. It often begins with a specific situation that feels urgent—maybe you’re facing final exams and feel overwhelmed, or you’re struggling to keep up at a demanding job while watching colleagues seem effortlessly productive. Some people turn to Adderall hoping it will help them lose weight quickly, while others use it to self-medicate undiagnosed ADHD, depression, or chronic fatigue.
The appeal often comes down to Adderall’s reputation as a “smart pill” that seems relatively safe since it’s prescribed by doctors. But what many people don’t realize is that if you don’t have ADHD, Adderall won’t actually make you smarter.3 It might make you feel more confident and focused, but studies show it doesn’t improve actual performance in people who don’t need it medically.
Why Young People Are Especially Vulnerable
Young adults and college students face a perfect storm of factors that make Adderall misuse particularly tempting. Their brains are still developing the parts responsible for decision-making and risk assessment, making them more likely to try risky solutions without fully considering the consequences.
College culture often normalizes stimulant use4—it’s not uncommon to hear students casually mention taking Adderall to pull all-nighters or cram for exams. Plus, it’s easily available on campus through friends with legitimate prescriptions, making it seem safer and more accessible than other drugs. Add in the intense academic pressure, irregular sleep schedules, poor eating habits, and limited coping skills that come with newfound independence, and Adderall can seem like an easy fix for feeling overwhelmed.
Unfortunately, young people’s more adaptable brains also mean they can develop dependence faster5 than adults.
Recognizing the Warning Signs of Adderall Addiction
Physical signs of Adderall dependence often appear first. You might notice:
- Significant weight loss
- Trouble sleeping or changes in sleep patterns
- Faster heartbeat, even when not taking the medication
- Frequent headaches
- Dry mouth
- Feeling jittery or restless
Behavioral changes can be more subtle but equally important:
- Taking higher doses than you originally planned
- Using it more frequently than intended
- Feeling anxious when your supply runs low
- Thinking about Adderall throughout the day
- Planning your schedule around doses
Mental and emotional symptoms can be especially challenging:
- Mood swings or increased irritability
- Increased anxiety when the medication wears off
- Feelings of depression between doses
- Feeling “flat” or unmotivated without Adderall
- Doubting your ability to perform well without it
These changes can affect your relationships and responsibilities, too. You might withdraw from friends and family, miss important events, or struggle to maintain your usual activities. Professional and academic performance actually decline when people abuse Adderall,6 as it creates a cycle that makes you feel like you need even more to function effectively.
Understanding Withdrawal and “Crashes”
A “crash” happens when the effects of Adderall wear off, which can leave you feeling exhausted, depressed, and mentally foggy. This isn’t just being tired—it’s your brain struggling to function without the chemical boost it’s gotten used to.
Withdrawal symptoms7 typically include:
- Extreme fatigue
- Difficulty concentrating
- Intense cravings for the medication
- Depression that can feel overwhelming
- Irritability or mood swings
- Anxiety
- Disrupted sleep patterns (sleeping too much or insomnia)
These symptoms usually peak within the first few days of stopping and can last several weeks. The timeline varies based on how long you’ve been using Adderall, how much you usually take, and your brain chemistry.
This is why stopping cold-turkey can be not only uncomfortable but potentially unsafe. Your brain needs time to readjust and start producing its own dopamine again. Medical supervision during this process helps ensure your safety and makes the experience more manageable.
Safe Ways to Stop Using Adderall
The safest approach to stopping Adderall is to work with a healthcare provider who understands prescription stimulant dependence. They can help you create a plan that minimizes withdrawal symptoms and reduces health risks.
Medical supervision is particularly important because Adderall affects your cardiovascular system. Stopping suddenly can cause blood pressure and heart rate changes that need monitoring. Your care provider can also prescribe medications to help manage withdrawal symptoms that affect your mental health, like depression or severe fatigue.
Many people benefit from a gradual reduction8 rather than stopping all at once. This gives your brain time to adjust, which can make the process a lot more comfortable. Your treatment provider might also recommend nutritional support. This strong central nervous system stimulant has a side effect of suppressing appetite,9 which can lead to deficiencies.
Practical preparations matter too. Plan to stop during a less stressful period if possible, stock up on nutritious foods, and consider how you’ll manage work or school responsibilities while your energy and focus return to normal levels. Don’t be afraid to lean into your support system during this time—social support can make a huge difference in your recovery experience.
Practical Steps for Quitting Adderall
1. Talk to Your Healthcare Provider
Some people worry that they’ll be judged for discussing their Adderall use with their doctor. Remember that healthcare providers are bound by confidentiality,10 and their job is to help. You can start by saying: “I’ve been using Adderall without a prescription and I’m concerned about my use. I’d like help stopping safely.” Be honest about how much and how often you use it—this helps them create the safest plan for you.
2. Find an Adderall Addiction Treatment Program
When researching treatment options, ask about their experience with stimulant medication dependence, what therapies they offer, and what kind of support they provide during withdrawal. Also inquire about insurance coverage, payment options, and whether they offer flexible scheduling if you need to maintain work or school commitments.
Learn the right questions to ask potential providers in our guide to what to ask a rehab center to make sure you find the right program for your needs.
3. Take Time Off if You Need To
You don’t necessarily need to share specific details with employers or schools. You can simply say you’re addressing a medical issue that requires treatment and ask about your leave options.
If you’re concerned about protecting your job while seeking treatment, learn exactly what to say to your employer and understand your legal rights in our guide to how to request time off work for rehab.
Treatment Options and Support
Several treatment approaches can help you overcome Adderall addiction. The best option for you depends on your specific situation and needs.
Behavioral Therapy
Professional treatment often includes behavioral therapy, which can help you understand why you’re using Adderall as a coping strategy and teach you healthier strategies for handling those situations. Contingency management,11 for example, is one evidence-based therapy that’s proven effective for stimulant dependence. If you attend a comprehensive addiction treatment program, your team will design a treatment plan that combines the therapies that work best for you and adjust that plan as needed to match your progress.
Inpatient vs. Outpatient Treatment
Some people do well with outpatient programs that let them keep up with work or school while going to regular therapy sessions. Others can benefit from more intensive inpatient treatment, especially if they’ve tried to quit before or are dealing with other mental health issues, too.
Whichever option you choose, make sure your program helps you plan for aftercare to sustain the work you’ve done for long-term recovery.
ADHD Evaluation and Alternatives
If you were using Adderall to manage undiagnosed ADHD symptoms, a proper evaluation can determine whether you actually have ADHD and would benefit from legitimate treatment. If you’re not comfortable taking ADHD prescription medication, you can talk to your therapist about non-stimulant ADHD medications, behavioral interventions, and lifestyle changes, all of which can be effective alternatives.
Mental Health Support
A lot of people who misuse Adderall are also dealing with mental health conditions like anxiety, depression, or perfectionism. Getting help for these underlying issues makes it much easier to stay off Adderall long-term.
Support Groups
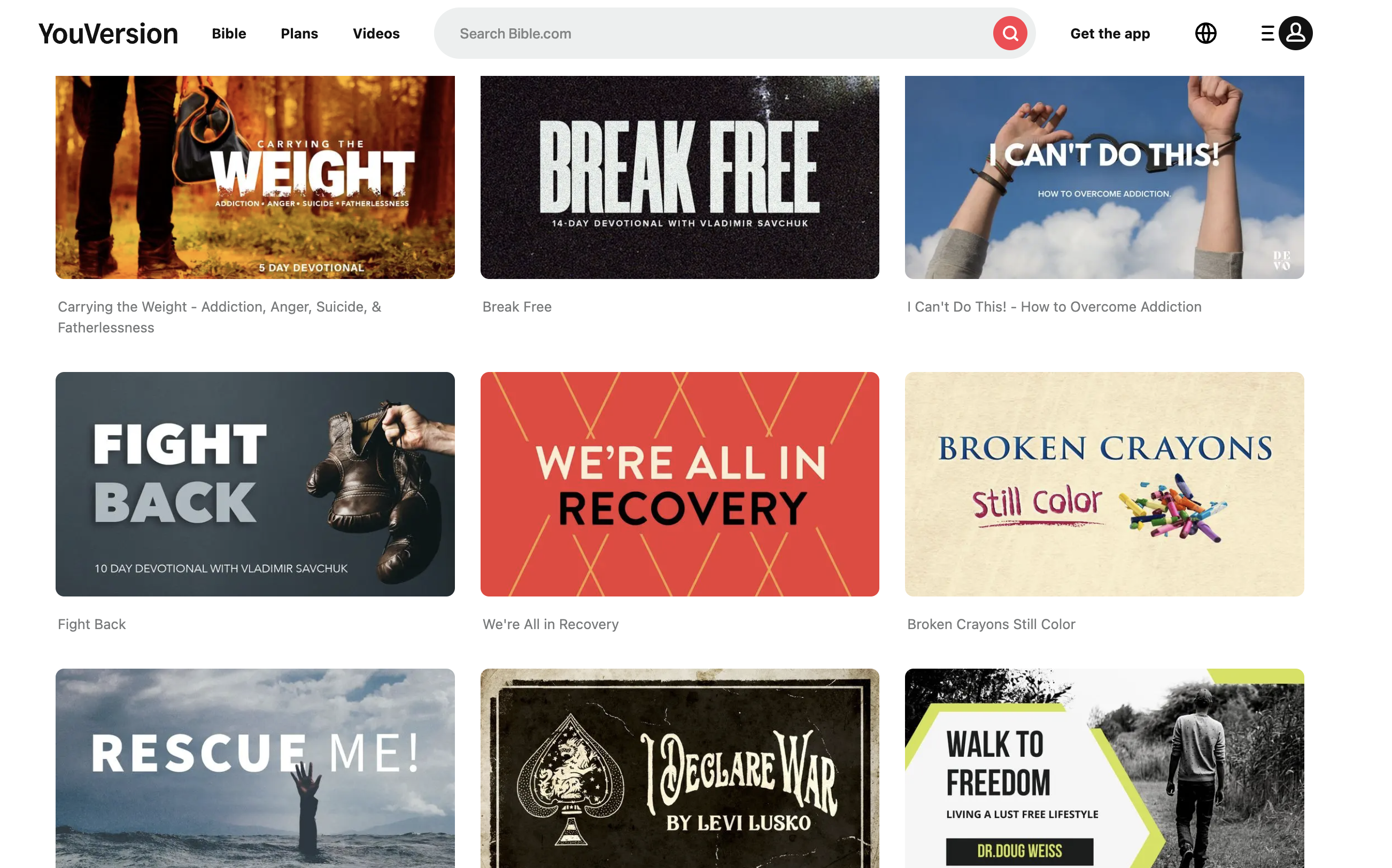
Support groups, whether in-person or online, connect you with others who understand what you’re going through. Hearing the experiences of people on similar journeys and learning what worked for them can be incredibly valuable.
Coping Strategies
While professional treatment provides the foundation for recovery, there are also practical strategies you can use day-to-day to manage challenges and support your healing process.
Managing Cravings
When cravings hit, try the “urge surfing” technique: acknowledge the craving without acting on it, and remind yourself it will pass. Distract yourself with physical activity, call a supportive friend, or engage in a hands-on task. Keep a list of reasons why you want to stop using Adderall where you can easily see it.
Natural Comfort During Withdrawal
For mild withdrawal symptoms, prioritize sleep, gentle exercise, and nutritious meals to help your brain heal. Stay hydrated and consider supplements like B vitamins (with your doctor’s approval). However, if you’re experiencing severe depression, intense cravings, or significant physical symptoms, seek medically supervised detox for your safety.
Handling Social Situations
Try preparing responses ahead of time:
- “I’m not doing that anymore.”
- “I’m taking a break from stimulants.”
You don’t owe anyone a detailed explanation. Consider avoiding situations where you’ll be offered Adderall until you feel more confident in your recovery.
Study and Work Strategies
Break large tasks into smaller chunks, use timers for focused work periods, eliminate distractions, and create organized environments. Consider accommodations like extended deadlines while you adjust. Your natural focus will return—it just takes time.
Get Effective, Professional Help
If you or your loved one is unable to stop using Adderall on your own, experiencing severe withdrawal symptoms, or if your use is affecting your relationships, or responsibilities, or well-being, it’s best to reach out for professional help.
Many treatment centers offer specialized programs specifically for prescription drug abuse. Search for a treatment program that matches your needs and start your recovery journey today.
FAQs
Q: Is it bad to take Adderall every day without a prescription?
A: Yes. Daily use without medical supervision significantly increases your risk of dependence, heart problems, mental health issues, and other health problems.
Q: What causes Adderall addiction?
A: Adderall changes brain chemistry by increasing dopamine levels. Over time, your brain produces less natural dopamine, creating dependence. Psychological factors like stress, perfectionism, or pressure to perform also contribute.
Q: How long does Adderall withdrawal last?
A: Acute withdrawal symptoms typically peak within 2–4 days and can last 1–3 weeks. However, some people experience mood and energy issues for several months as their brain chemistry rebalances.
Q: Why is Adderall misuse so common among young adults and adolescents?
A: Young adults and teens face intense academic and career pressures that make Adderall seem like a performance enhancer. Their developing brains also have less impulse control and risk assessment ability. Easy access through friends with prescriptions makes it feel safer than other stimulants. These factors create high risk for misuse and dependence.
Q: Can you overdose on Adderall?
A: Yes, Adderall overdose is serious and potentially life-threatening. Warning signs include rapid heartbeat, high blood pressure, chest pain, trouble breathing, high fever, severe agitation, confusion, or panic attacks. Serious cases can cause seizures, stroke, or heart problems. Call 911 immediately if you suspect an overdose—don’t wait to see if symptoms improve.