Recognizing when a loved one is struggling with substance use can be confusing, heartbreaking, and overwhelming. You may feel desperate to help, but unsure of how to do so without enabling their behavior or pushing them away.
Fortunately, with patience, compassion, information, and evidence-based strategies, it’s possible to support someone through the recovery process.
1. Recognize the Signs of Addiction in Others
Addiction isn’t always obvious. While some people display clear warning signs, others—especially people with high-functioning addiction—may mask their struggles with problematic drug use or addiction behind a facade of normalcy.
Common signs of addiction1 include:
- Behavioral red flags: Secrecy, denial, impulsivity, lying, or missing obligations
- Emotional signs: Mood swings, irritability, anxiety, or depression
- Physical indicators: Weight changes, bloodshot eyes, slurred speech, or poor hygiene
In people with high-functioning addiction,2 drug or alcohol use may remain hidden due to career success or social engagement. However, you might still notice subtle patterns related to behavioral health like isolation, frequent “bad days,” or noticeable shifts in demeanor. Many also exhibit a cycle of justification, denial, or defensiveness.
For children or young adults,3 these common signs can also include changes in friend groups, a decrease in participation in school functions or extracurriculars, or changes in grades and academic performance.
2. Understand There Is a Why Behind Substance Use
People don’t usually turn to drugs or alcohol just because they’re bored, they use substances to cope with pain, trauma, or emotional overwhelm. Addiction often starts as a form of control of a seemingly uncontrollable situation.
Substances may offer short-term relief from anxiety, depression, loneliness, or past wounds. In the beginning, the ability to change how you feel with a drink or a pill can seem empowering. But over time, that temporary sense of control, however, can turn into dependency and eventually, loss of control.
Understanding this doesn’t mean you’re excusing the behavior, but it does help you meet your loved one with greater compassion. It shifts the conversation from:
- “Why don’t you just stop?” to “What are you trying to escape or manage?”
- “What’s wrong with you?” to “What happened?”
Most people with substance use disorder are carrying deep emotional burdens. Recognizing the underlying why behind their substance use can guide more effective, empathetic support and help you focus not just on the behavior or coping mechanism,4 but the pain beneath it.
3. Educate Yourself About the Science of Addiction
Addiction may not have a one-size-fits-all cure, but with the right knowledge and support, you can be better prepared to support a loved one. One of the most empowering steps you can take is to understand what addiction really is.
Addiction is a chronic brain disease,5 not a moral failing or a lack of willpower. Long-term substance use changes how the brain communicates, especially in areas related to reward, decision-making, and impulse control. This disruption often stems from changes in neurotransmitters like dopamine, which plays a major role in pleasure and motivation.
At first, for your loved one, using substances may feel like a choice, but over time, the brain rewires itself, increasing tolerance and craving while decreasing natural dopamine production. That’s when people often feel “trapped”—not weak, but physically and mentally hooked.
Understanding these biological realities6 helps reduce blame and increases compassion. It also reminds us that support, grace, and education are crucial parts of the healing process.
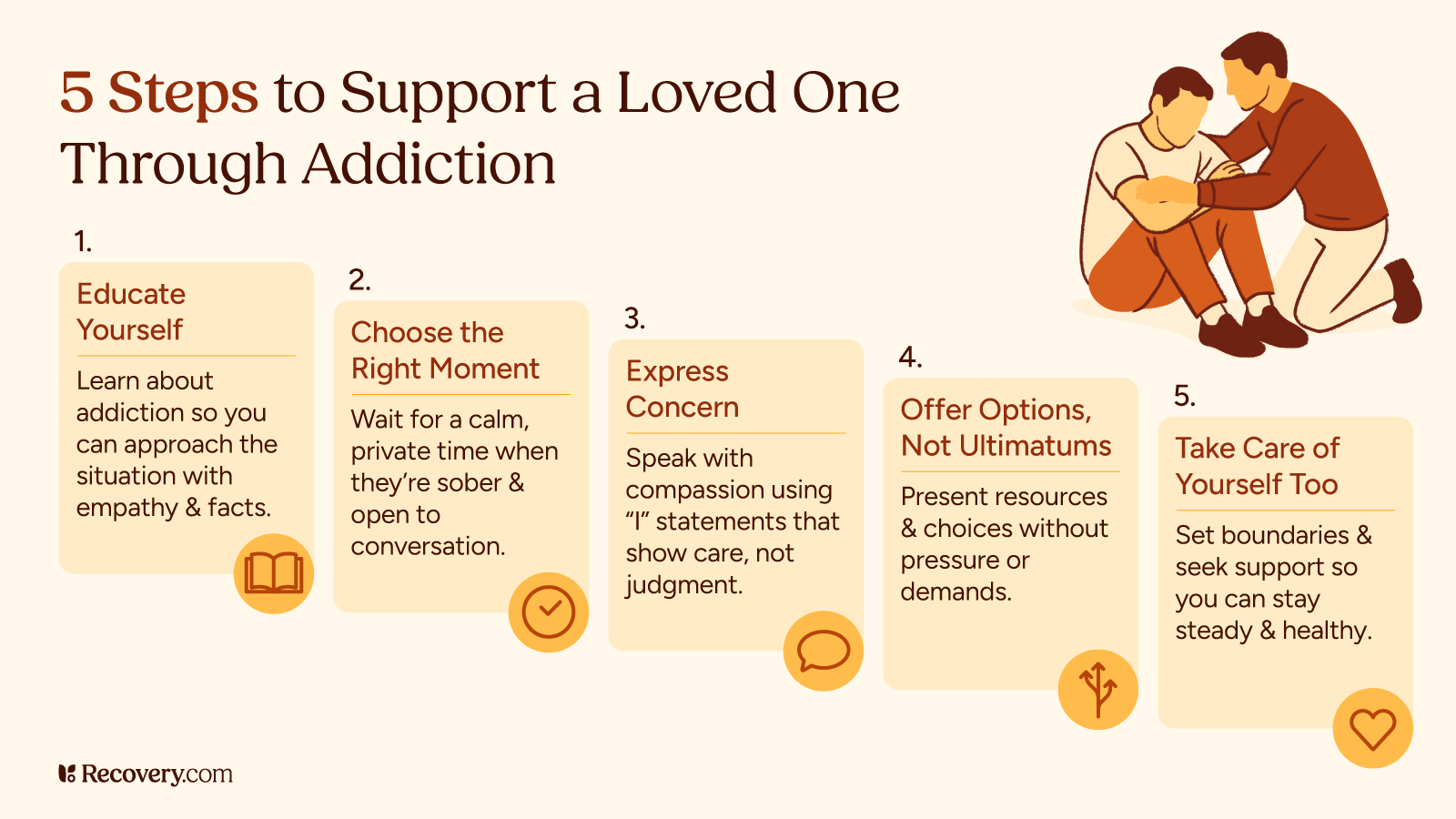
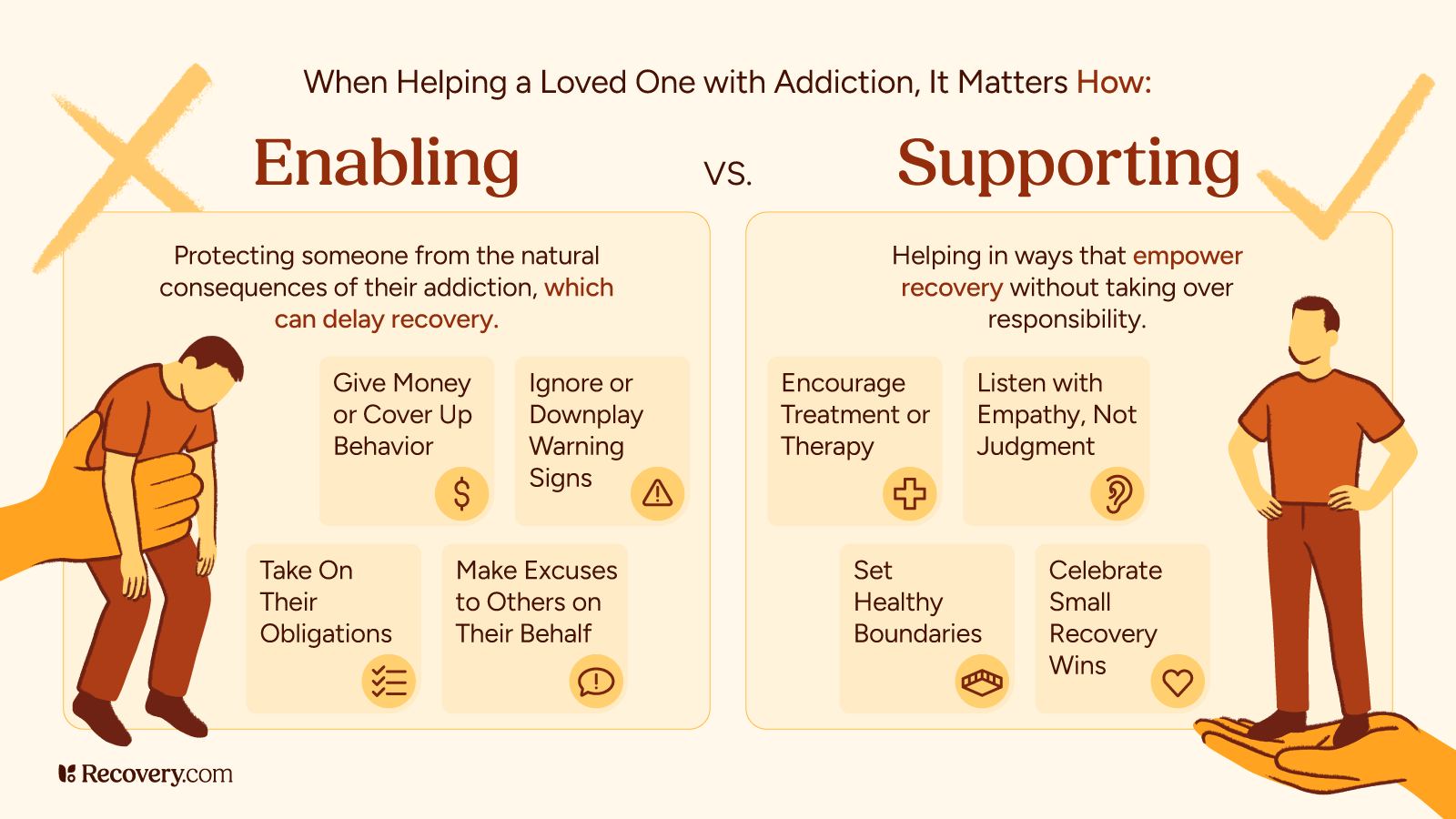
4. Learn the Dos and Don’ts of Supporting Someone in Addiction
Loving someone with an addiction requires empathy, education, and strong boundaries. You might be feeling helpless, but there are things you can do. Here are some practical ways to offer support:
Do:
- Listen with compassion. Let them talk openly and acknowledge what they’re feeling without judgment.
- Set healthy boundaries. Set clear limits around what you’re able to offer and follow through.
- Learn about addiction and recovery. Understanding substance use, withdrawal, and treatment options can help you support them better.
- Celebrate progress. Encourage small steps forward and remind them that change takes time.
Don’t
- Don’t enable or protect them from consequences. Covering up, making excuses, or giving money can unintentionally prolong the problem.
- Don’t give ultimatums before they’re ready. Lasting change usually starts with internal motivation, not outside pressure.
- Don’t blame yourself. Their choices are not your fault, even when it’s hard to watch.
- Don’t expect them to quit cold turkey. Sudden withdrawal from substances like alcohol or benzodiazepines can cause death without medical support.
Supporting someone who’s struggling with addiction7 can be emotionally draining. It’s important to keep in mind that you matter, too. It’s important to care for your own heart and well-being as you walk alongside your loved one.
You won’t be able to fix everything and that’s okay. Healing is a long road, and it’s not your job to carry it all.
Set boundaries that protect your peace. If a conversation becomes too intense, give yourself permission to step away. A simple pause can make space for clarity, calm, and compassion. Come back when you’re ready with a clearer mind and a softer heart.
And remember: you don’t have to be involved in every part of their journey. Showing up consistently in small, healthy ways often speaks louder than trying to do it all.
5. Understand How to Talk to Someone About Their Addiction
Confronting someone about their substance use is difficult, but it can also be a turning point. To have the best outcome, choose a calm, private setting and use non-threatening language.
Pam Lanhart, Founder and Director of Thrive Family Recovery Services shares:
First, we need to listen to our loved ones well and listen for language that might indicate that they are getting tired of the way things are. Then we validate that and ask them what it might look like to do something different. ‘What step do you think you might be able to take to move forward?’
We need to be patient and let them feel like they have agency in these decisions. Walking with them while they figure things out is critical. And of course, we can’t do that if we don’t have boundaries. I love language such as ‘say more about that,’ or ‘Can you tell me more?’ or ‘I’m trying to understand. Can you explain?’ Just listen and be curious because they know what they need and will often come to the conclusion themselves.
Here are a few brief conversation tips that can help you as you communicate with your loved one who may be struggling with an addiction.
Conversation Tips
- Start with an “I” statement: “I’ve noticed you seem stressed lately, and I’m worried about you.”
- Express concern, not control: “I care about your well-being and want to help.”
- Avoid labels like “addict” or “junkie,” which can cause shame or defensiveness.
Timing matters. Choose a moment when they’re sober and not in a state of crisis or withdrawal.
6. Decide When and How to Encourage Treatment
Suggesting treatment should be a compassionate invitation, not a demand. If the person is open to help, present options like:
- Speaking with a mental health professional or healthcare provider
- Considering inpatient or outpatient addiction treatment programs
- Exploring evidence-based options such as behavioral therapy, medication-assisted treatment, detox, or other types of medical treatment
- Encouraging holistic wellness and recovery support services
It’s normal for people to resist the idea at first. Ambivalence doesn’t mean they’re not willing—it often means they’re afraid or unsure of what recovery entails.
How do people change? Over time. With stops and starts, along a crooked line. With practice. With ambivalence. More often than not, without formal help. When the trade-offs seem worth it. With a little help—sometimes a lot of help—from friends and family. With anguish. With effort. With joy.
― Jeffrey Foote, PhD., Beyond Addiction: How Science and Kindness Help People Change8
7. Know What to Do if They Refuse Help
Refusal doesn’t mean you should give up. Harm reduction strategies9 can keep your loved one safer, sometimes easing cravings, while leaving the door open for change:
- Encourage safer practices (like not mixing substances and using clean supplies)
- Stay emotionally available without enabling
- Know your limits and take care of yourself
You might need to seek your own mental health support or attend family therapy to cope with feelings of guilt, anger, or helplessness. That’s okay. Recognizing that addiction impacts the entire family and not just the person struggling is key to a healthy recovery journey for everyone.
8. Get Familiar With Resources for Families and Friends
Support services exist for those affected by a loved one’s addiction.10 You are not alone.
- Al-Anon and Nar-Anon: Peer-led groups for family and friends
- SMART Recovery Family & Friends: Offers tools based on cognitive behavioral therapy
- SAMHSA resources that define and discuss recovery principles and supports
- Books and podcasts that explore addiction and family dynamics
- Helplines that provide 24/7 support
- Therapy with a mental health professional familiar with substance use disorders
Helping someone with drug use, drug addiction, or alcohol use isn’t about fixing them—it’s about walking beside them, with compassion and hope. Whether they’re seeking professional help or resisting treatment options, your role matters. Take steps to protect your own well-being, stay informed, and know that recovery is possible for your family member—even when the road is long.
Connect With Professional Support
Ready to connect your loved one with professional help? Find qualified addiction treatment programs in your area that offer personalized care and proven recovery methods.
FAQs
Q: What should you not say to someone who has an addiction?
A: Avoid blaming, shaming, or using stigmatizing terms like “junkie” or “addict” when talking to or about your family member. Phrases like “just stop” or “you’re ruining everything” often shut down communication. Focus instead on expressing care and concern while encouraging effective treatment options.
Q: How can I help without enabling?
A: Helping without enabling means supporting their recovery, not their addiction. Avoid giving money, covering up consequences, or making excuses. Instead, offer emotional support, resources, and healthy boundaries.
Q: What are some ways to help people who are suffering from addiction?
A: You can help by listening without judgment, offering treatment options, and encouraging small steps toward change. Support groups, harm reduction strategies, and family therapy can also make a difference.
Q: What is substance use disorder (SUD)?
A: A substance use disorder is a medical condition characterized by an uncontrollable urge to use drugs or alcohol despite negative consequences. It affects brain function and behavior and often requires comprehensive treatment.
Q: How do I get a loved one to admit they have a problem?
A: Use “I” statements to express concern, avoid confrontational language, and choose a calm moment to talk. Understand that denial is common and change takes time.
Q: How do I know if someone needs help for their drug or alcohol use?
A: Warning signs of alcohol addiction or other drug abuse include neglecting responsibilities, changes in mood or behavior, secrecy, physical deterioration, and an inability to stop despite consequences. A professional assessment can clarify their needs.
Q: Is there a good way to convey addiction concerns to a family member or friend?
A: Yes. Speak from a place of compassion using statements like, “I’ve noticed some changes and I’m worried.” Choose a quiet time, avoid judgment, and be prepared for resistance.
Q: Are you covered for addiction treatment?
A: Many insurance plans cover addiction treatment, including inpatient, outpatient, and therapy options. Check with your insurance provider or rehab admission team for guidance on available coverage.
Q: What are effective ways to support someone in recovery from addiction?
A: Offer encouragement, celebrate milestones, be patient during setbacks, and avoid substances around them. Attending support groups together and staying informed can strengthen your role in their recovery. Encouraging effective treatment plans that address not only substance use, but also co-occurring mental health conditions, is important.
Q: What steps can I take to support someone seeking addiction recovery?
A: Help research treatment options, provide transportation or childcare if needed, and support attendance in therapy or peer groups. Remind them that recovery is a journey, not a destination.
