Stress and addiction can feed into and cause each other. “Stress” could be anything that taxes or exceeds your ability to healthily adapt1. For example, stress could prompt you to drink to cope with negative emotions. Similarly, having a heavy drinking habit could cause stress when it affects your life and well-being.
The bi-directional, sometimes cyclical relationship between stress and addiction can seem tricky to separate and treat. But with therapy and the right approach to treatment, you can heal from each and find an improved quality of life.
What Is The Relationship Between Stress And Addiction?
The relationship between stress and addiction is complex and multifaceted. Numerous studies have investigated their relationship and have provided insights into how stress can increase the risk of addiction.
Crucially, stress can cause someone to take and crave substances2. Chronic stress can further increase the risk of drug use and addiction. Stress can induce changes in neural pathways and cravings, which can contribute to substance-related disorders. The stress response system, including the hypothalamus-pituitary-adrenal (HPA) axis, plays a critical role3 in the development and maintenance of addiction.
Stress can also impact your ability to control impulses or other inappropriate behaviors, along with craving instant gratification.
Ultimately, the effects of stress can all lead to substance use. The American Psychological Association (APA) reveals that “stress is one of the most commonly reported precipitants of drug use4” and relapse.
More stress, or chronic stress, is also associated with a higher risk of substance use2 and addiction.
The Neurological Relationship
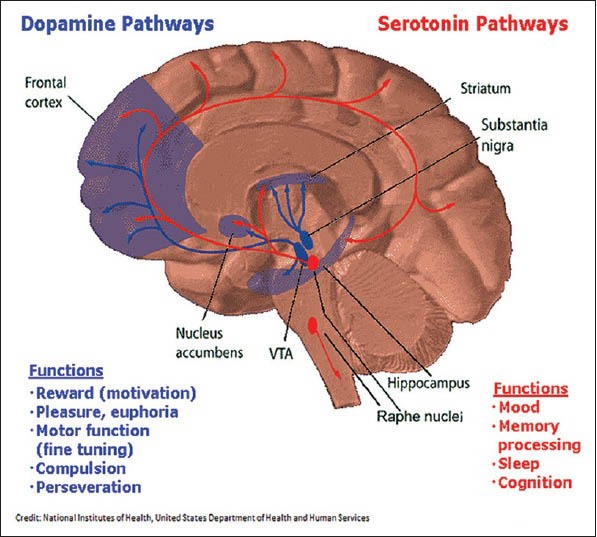
Stress can raise your levels of dopamine5, which is a neurotransmitter responsible for feeling good and reinforcing the activity that feels good. Alcohol and drugs increase your levels of dopamine6, too. Stress-induced alterations in dopamine transmission can increase the risk of addictive behavior.
Because it releases dopamine, you can even become addicted to stress7. And with stress and substance use affecting the system, it can be more difficult to disconnect one from the other and cope without the dopamine they produce.
The dopamine-intertwined relationship between stress and addiction can have negative but treatable effects on mental health and overall wellness.
Individual Factors
The relationship between stress and addiction is also influenced by individual factors, such as coping strategies and resilience. Effective coping strategies8 can protect individuals from the maladaptive effects of stress that can contribute to addiction.
On the other hand, maladaptive coping strategies, such as procrastination9, can increase the risk of addiction. Using substances as a maladaptive coping skill certainly increases the risk, too.
Additionally, those with lower levels of psychological resilience may be more susceptible to the effects of stress10 and more prone to developing addiction.
Effects of Stress And Addiction on Mental Health
Stress makes addiction and mental health conditions more likely to develop2. The untreated effects of stress increase your risk of anxiety, depression, and other mood-related disorders. In some cases, stress can cause trauma11 and conditions like post-traumatic stress disorder (PTSD).
Multiple stressors or chronic stress can also be the catalyst2 between using a substance and becoming addicted to one. The more stressors you have in your life, the more likely you are to develop an addiction.
How to Treat Stress and Addiction
Treatment that addresses your stress and addiction simultaneously can help you heal from both conditions. Therapy, wellness activities, and at-home coping strategies can help you manage stress and recover from addiction.
Therapies for Stress and Addiction
- Stress management skill training1: This therapy can reduce emotional reactions to stress, helping you avoid relapses. You’ll usually attend 12 sessions in group therapy, learning a specific skill each time.
- Cognitive behavioral therapy (CBT)1: CBT can help you regulate your emotions and how to respond to stress without using substances. You’ll learn and practice coping skills in and out of therapy.
- Mindfulness meditation12: This therapeutic intervention helps you enter a state of meditation where you’re mindful of what you’re feeling and accepting how the emotions feel in your mind and body. Meditation practices can then lower your breathing and slow your heart, helping you calm your mind and body simultaneously.
- Dialectical behavioral therapy (DBT)13: A mindfulness-based behavioral therapy focusing on emotional regulation. Similar to mindfulness meditation, you’ll work on becoming more aware of what you’re feeling and accepting the emotions. Then, you’ll learn how to regulate your emotions and your stress, which can help lower stress and prevent relapse.
Stress-Reducing Activities
- Yoga: the guided movements and stretches of yoga can help you manage stress.
- Mindfulness: everyday mindfulness can help you hone in on big and small experiences, like feeling the wind or noticing the birds in the sky as you walk into work. Mindfulness can calm your body as your focus drifts to what’s happening around you. Mindfulness can effectively reduce stress without alcohol or drugs.
- Exercise: movement can reduce stress and burn off nervous energy it may cause. You could go on a daily walk, spend time in the gym, or move in any way that feels good to you.
- Baths: a warm bath, especially one with epsom salts and essential oils, can calm the mind and body. Baths can also reduce soreness and pain.
- Progressive muscle relaxation14: a mindfulness technique where you gradually tense and relax your muscles. You can start at your toes and end at your head, but the pattern is up to you.
- Create something: art, music, or writing can take you out of a stressful mindset and help you process what’s stressing you out.
- Self-compassion15: Dr. Kristin Neff suggests self-compassion as a tool for stress reduction–one you can do at any time. Her research has found self-critical approaches to failure or struggle only results in further stress. Practicing self-compassion can cause greater emotional calm and keep your stress from escalating.
Find Relief for Stress
Treatment can effectively stop the cycle of stress and addiction, help you avoid relapse, and feel better as a whole. You can find rehabs treating stress by browsing our list of rehabs for stress with photos, reviews, and insurance information to help you make an informed decision.