Trying to figure out what kind of treatment you need can feel like stepping into a maze. You might be asking: Do I need to detox first? Is inpatient too much? What even is PHP? If you’re feeling unsure or overwhelmed, you’re not alone—and you’re not doing anything wrong.
This guide is here to help you understand what your options actually look like in practice. From round-the-clock care to flexible weekly therapy, different levels of care are appropriate for different situations. Knowing how they work can make it easier to take the next step, whatever that looks like for you.
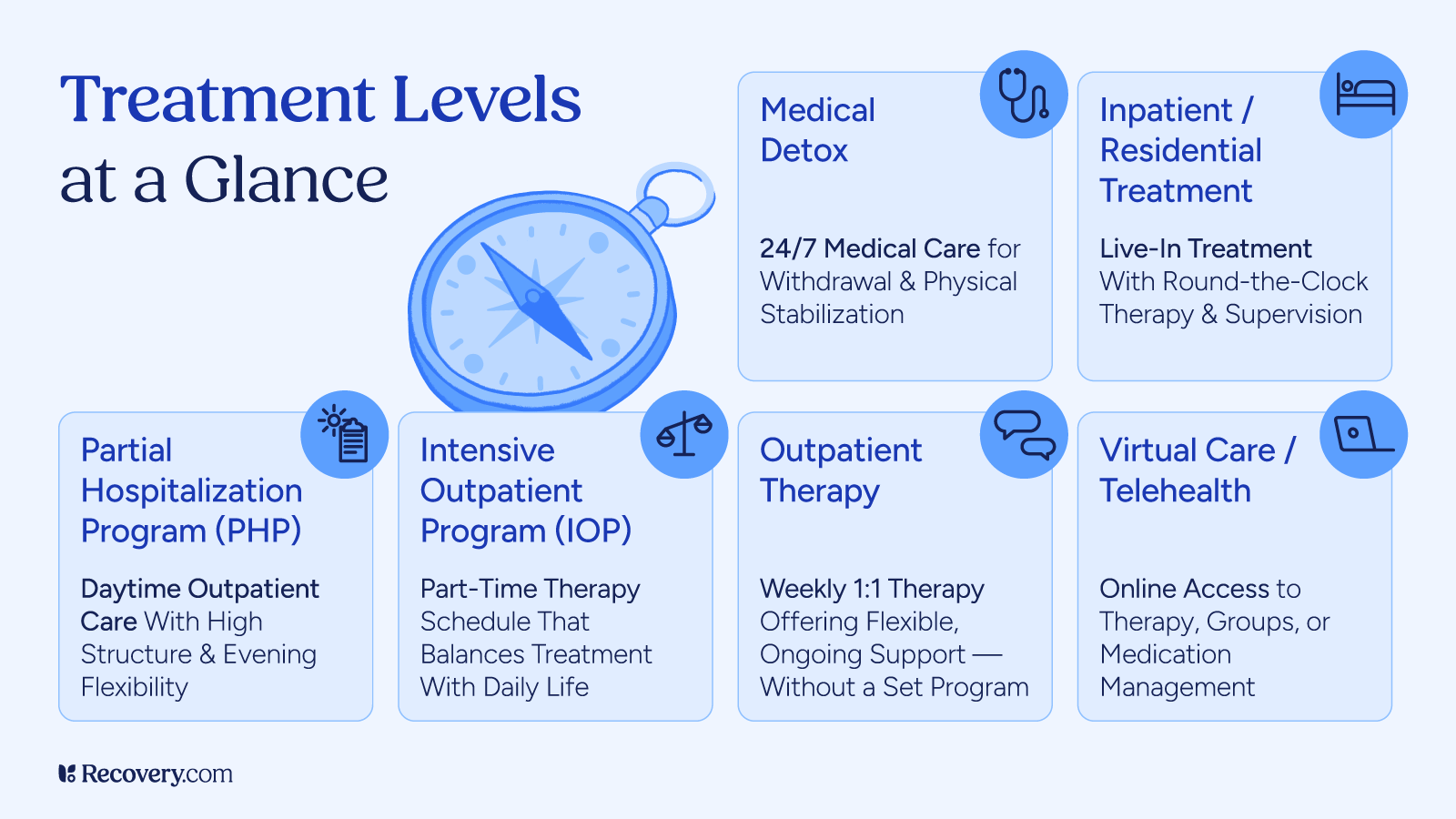
Levels of Care Explained
Addiction treatment takes place on a continuum of care, with various levels of care designed to meet people where they are. Some offer 24/7 medical support. Others give you space to keep working or caring for family members while getting help. Stepped-down treatment options allow you to gradually introduce more and more responsibilities into your life as your mental health and confidence improve.
Here’s what each one involves, so you can get a better sense of what best fits your life right now.
Medical Detox
- Typical duration: 5–10 days
- Hours per week: 24/7 care
- Time of day: Day and night
If you’ve been using substances (especially alcohol, opioids, or benzodiazepines) regularly, stopping suddenly can result in severe, or even fatal, symptoms. Medical detox gives you a safe place to withdraw with trained staff on hand. A qualified treatment team will monitor your symptoms, help you manage pain or discomfort, and step in if any complications arise.
This is often a preliminary step, prior to starting a comprehensive addiction treatment program, for people who are physically dependent on substances.
Learn more about what to expect in the detox process: See our detox FAQs.
Residential or Inpatient Treatment
- Typical Duration: 30–90 days
- Hours per Week: 24/7 care
- Time of Day: Day and night
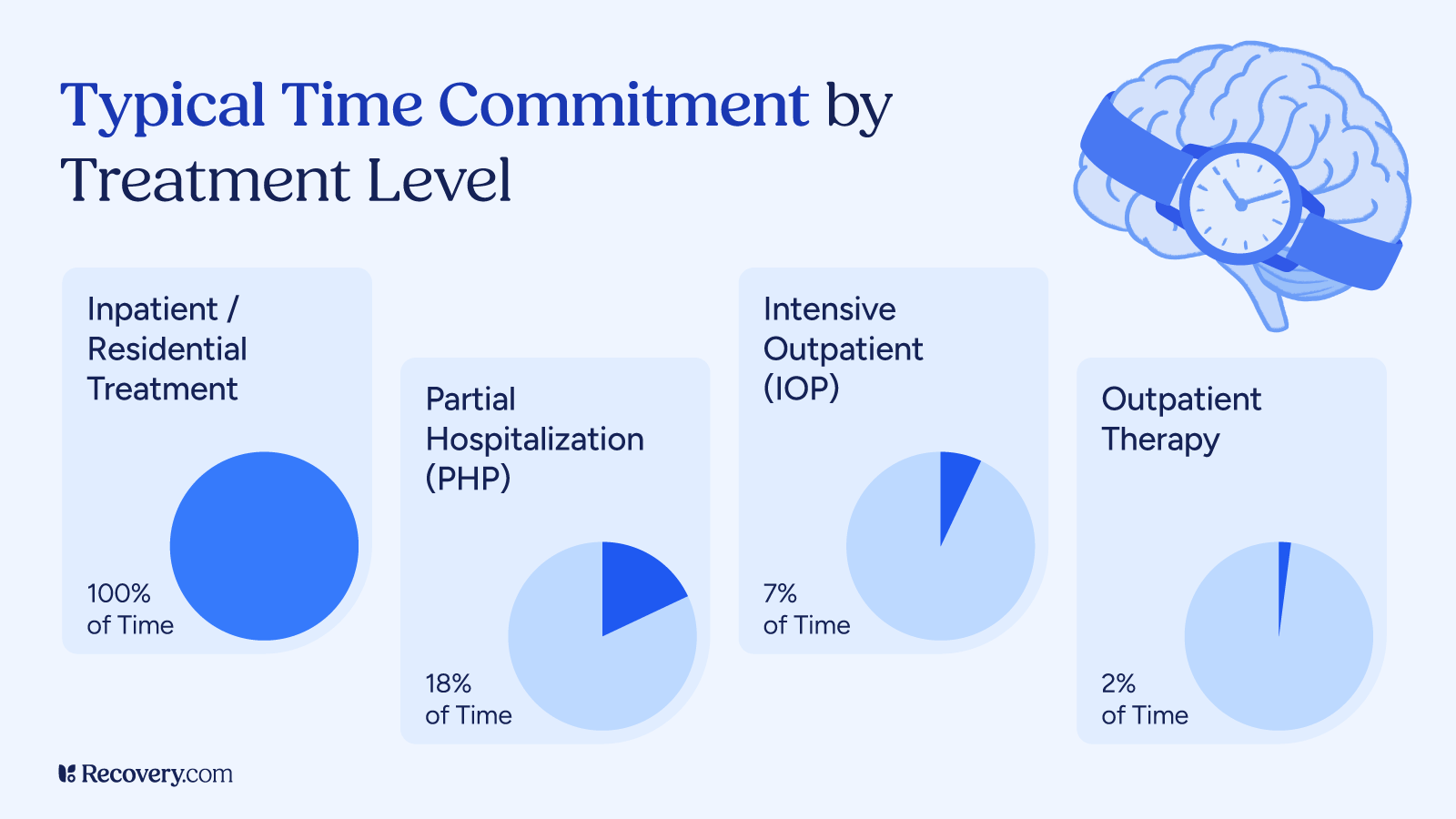
In residential rehab, you live at a treatment facility while focusing entirely on recovery. It offers a structured environment and full daily schedule of therapy, group support, mental health care, and activities that help you build new coping tools. Many residential programs also incorporate family therapy.
Because your meals, housing, and daily routine are all taken care of, you can put all your energy into getting better without juggling the pressures of work, school, or family obligations. It’s a space where your only job is to focus on your healing.
This level is a good fit if you need more acute care such as dual diagnosis or eating disorder treatment, or need space away from issues at home that may complicate your recovery.
Partial Hospitalization Program (PHP)
- Typical Duration: 15–30 days
- Hours per Week: 25–30 hours
- Time of Day: Primarily during the day
A PHP (also known as day treatment) is one of the most intensive available outpatient services. You’ll spend most of your day at a treatment center for therapy, psychiatric care, and medical check-ins, then go home (or to sober housing) in the evening. For most people, the time spent at a PHP feels like the equivalent of a full-time job.
PHPs are a step down from inpatient care but still offer a high level of structure and support, especially if stabilization is still a concern.
Intensive Outpatient Program (IOP)
- Typical Duration: 8–12 weeks
- Hours per Week: 9–15 hours
- Time of Day: Day or evening options
IOPs give you solid support without requiring you to put your life on hold. You’ll attend several individual and group therapy sessions each week, and may have access to medication management. The time commitment here is similar to a part-time job.
An IOP works well if you’re stepping down from a higher level of care, or if you’re juggling recovery with work, school, or family responsibilities.
Outpatient Therapy
- Typical Duration: Ongoing or as needed
- Hours per Week: 1–5 hours
- Time of Day: Flexible
Outpatient therapy can be as simple as seeing a therapist once a week. Some people start here if their symptoms are mild; others continue therapy after completing a more structured program. It’s a space to keep working through triggers, rebuild relationships, and stay grounded in your recovery over time. You can choose a schedule that fits your daily life.
Sober Living or Transitional Living
- Typical Duration: 1–12 months
- Hours per Week: Independent, with optional meetings
- Time of Day: Mostly daytime routines
Sober living homes are group environments where people in early recovery live together under shared rules. There’s no formal therapy, but you’ll usually have curfews, house meetings, and drug testing, as well as attending meetings and recovery-friendly activities outside the home. It’s a helpful bridge between structured treatment and living completely on your own—especially if your home environment poses challenges to your recovery.
Learn more about length of stay in different types of treatment in our article on how long rehab lasts.
Virtual Care (Telehealth)
- Typical Duration: Varies by program
- Hours per Week: 1–15 hours
- Time of Day: Day or evening availability
Virtual care lets you access therapy, support groups, and even medication management from home. It’s especially useful if you live in a rural area, have mobility issues, or just need more flexibility. Some people use it to start treatment; others use it to stay connected to a sober support network after in-person care. As long as you have a phone or internet connection, you can access high-quality behavioral health care.
How to Know What’s Right for You
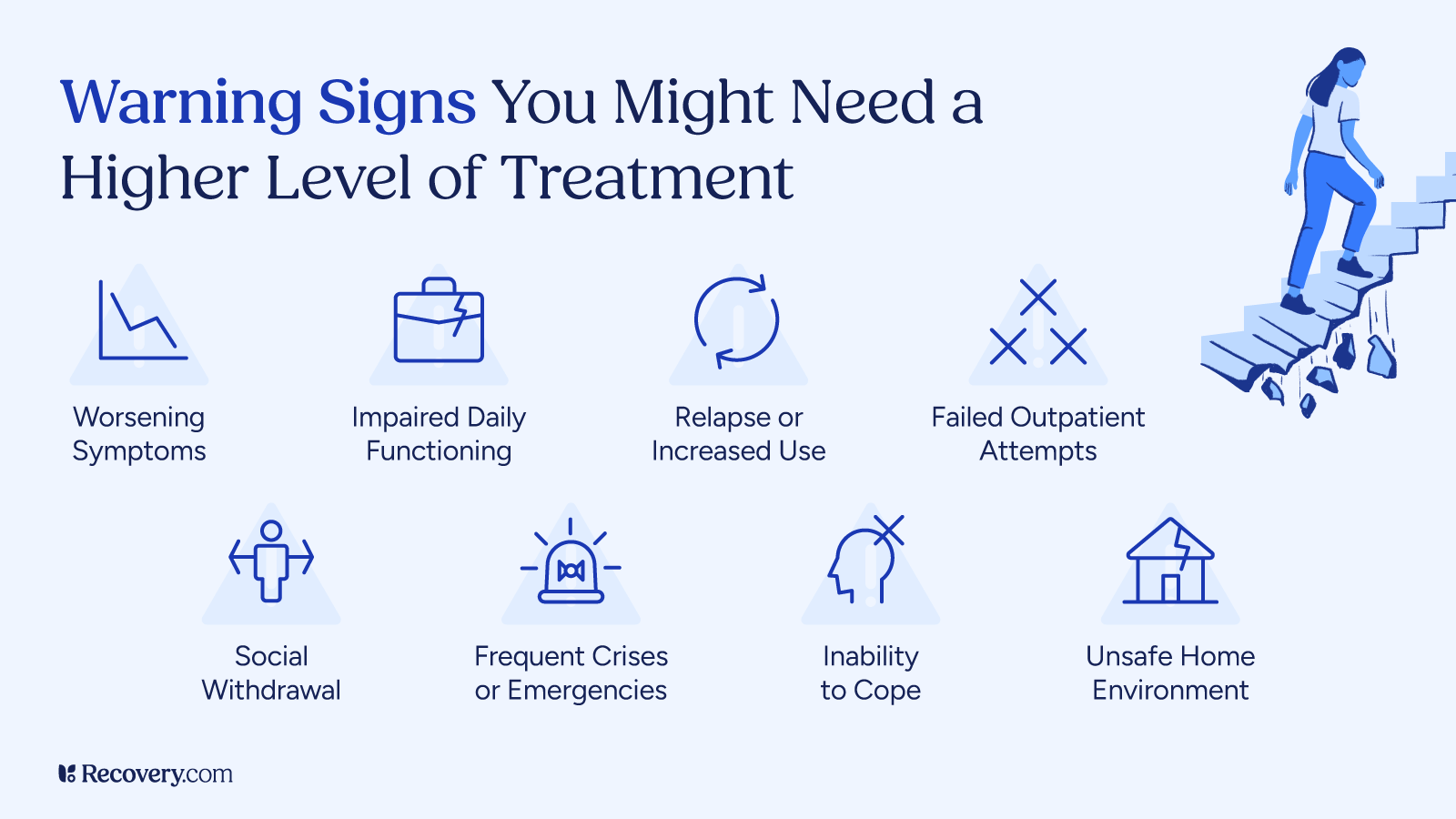
Choosing a treatment program is about finding what fits your circumstances and resonates with your approach to healing. Start by thinking about how withdrawal affects you, whether you’re also dealing with anxiety, depression, trauma, or other mental health disorders, and if you’ll have any specific needs while in treatment.
If you’re in crisis, can’t stop using on your own, or feel unsafe at home, inpatient care might be the most supportive place to begin. If you’re more stable or have responsibilities you can’t step away from, outpatient care may give you the balance you need.
There’s no wrong place to start. The most important thing is to start somewhere.
Do I Need Medical Supervision?
If you’ve ever had severe withdrawal symptoms (or you’re worried you might), it’s important to talk to an addiction specialist before you try to stop using on your own. Symptoms like seizures, hallucinations, or heart issues can be dangerous without medical support.
You might also need supervised care if you have certain medical needs such as a health condition that affects your recovery, or if you’re taking medications that could interact with withdrawal. Medical detox or inpatient treatment can give you safety and stability while your body adjusts.
Dual Diagnosis or Co-Occurring Disorders
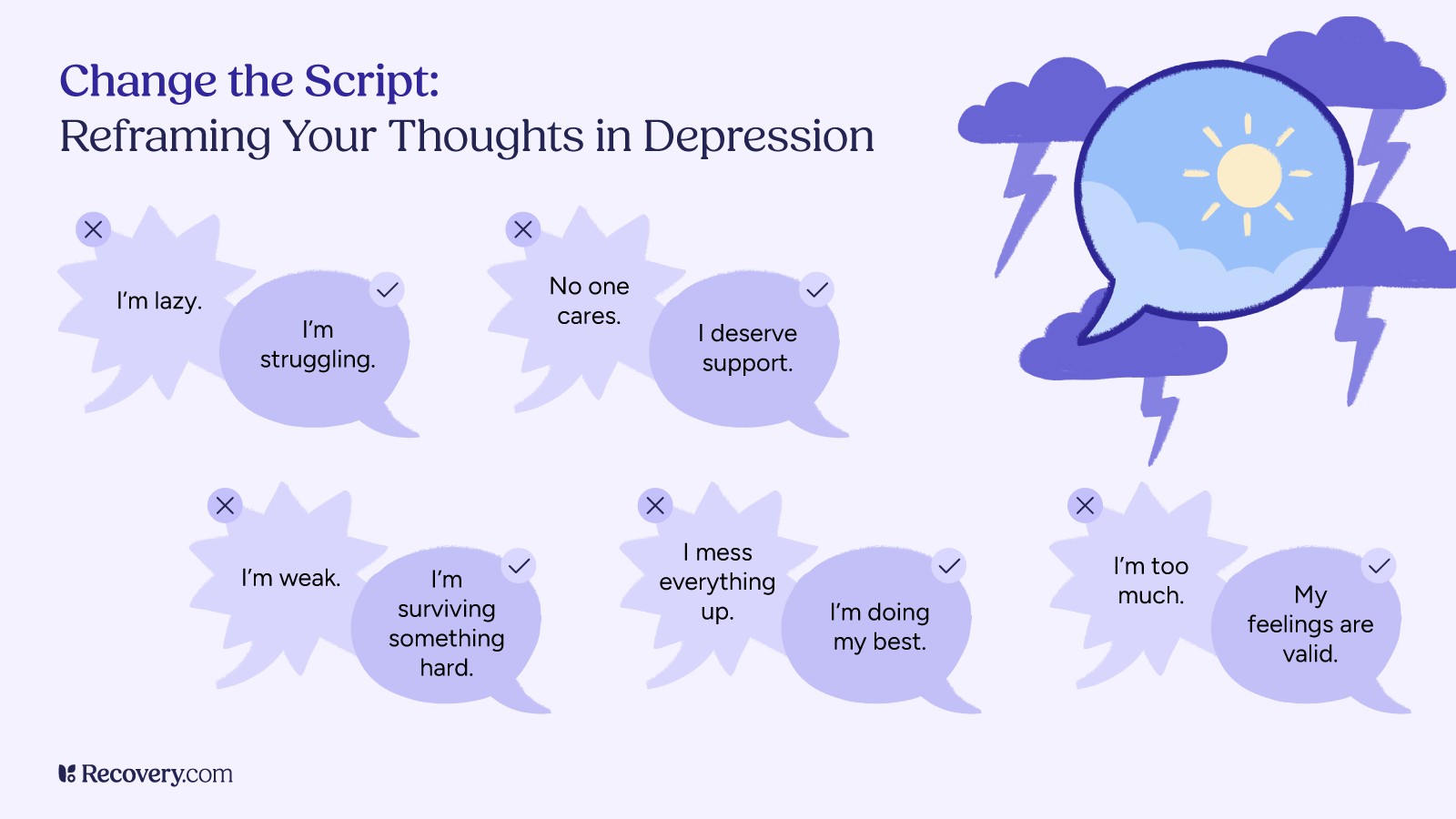
If you’re struggling with both mental health and substance use, you’re not alone—and you’re not a problem to solve. A lot of people use substances to cope with depression, anxiety, trauma, or other emotional pain. But over time, that coping can create its own set of challenges.
When both are happening at once, it’s called a co-occurring disorder. These situations often need integrated care: treatment that addresses mental health and substance use at the same time, not in separate silos.
Dual diagnosis treatment is available at most higher levels of care and some outpatient programs. If this applies to you, look for programs that offer addiction treatment, psychiatry, and trauma-informed support under one roof.
What an Intake Assessment Looks Like
Most treatment centers begin with an intake or admissions assessment to better understand your needs. This process typically includes two parts:
- A brief phone screening with an admissions advisor. This initial conversation covers basic information about your substance use, mental health, and immediate needs to determine whether the program is a good fit. It’s also your chance to get your questions answered.
- A more in-depth assessment once you arrive at the treatment center. This is usually conducted by medical and clinical staff and dives deeper into your medical history, substance use patterns, mental health conditions, living situation, and any safety concerns.
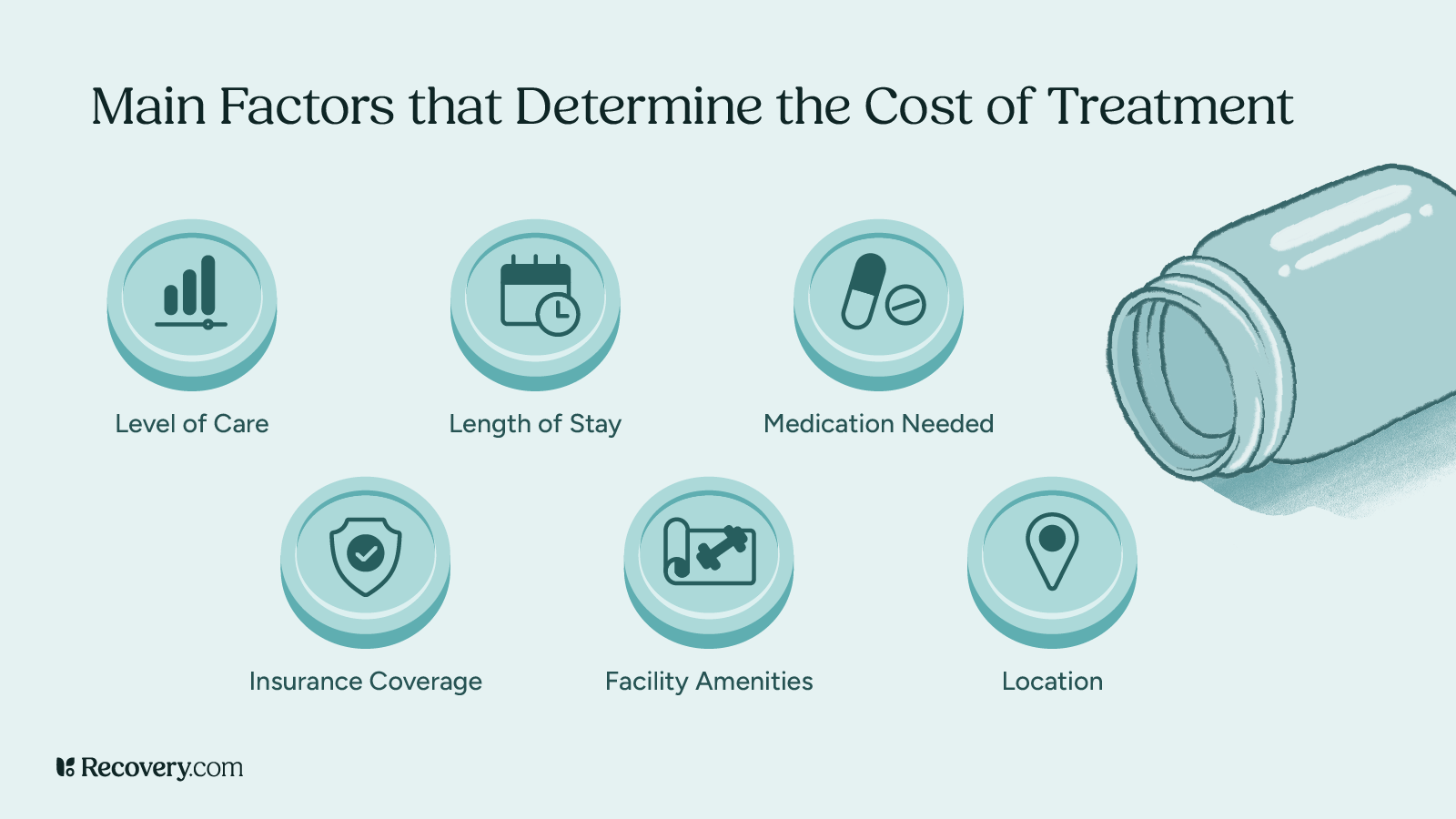
The goal is to get a full picture of your situation so the team can recommend the most appropriate level of care and build a personalized treatment plan. Clinicians often use tools like the ASAM Criteria1 (developed by the American Society of Addiction Medicine) and a biopsychosocial assessment to guide your treatment plan.
You don’t need to have all the answers going in, just be as honest as you can.
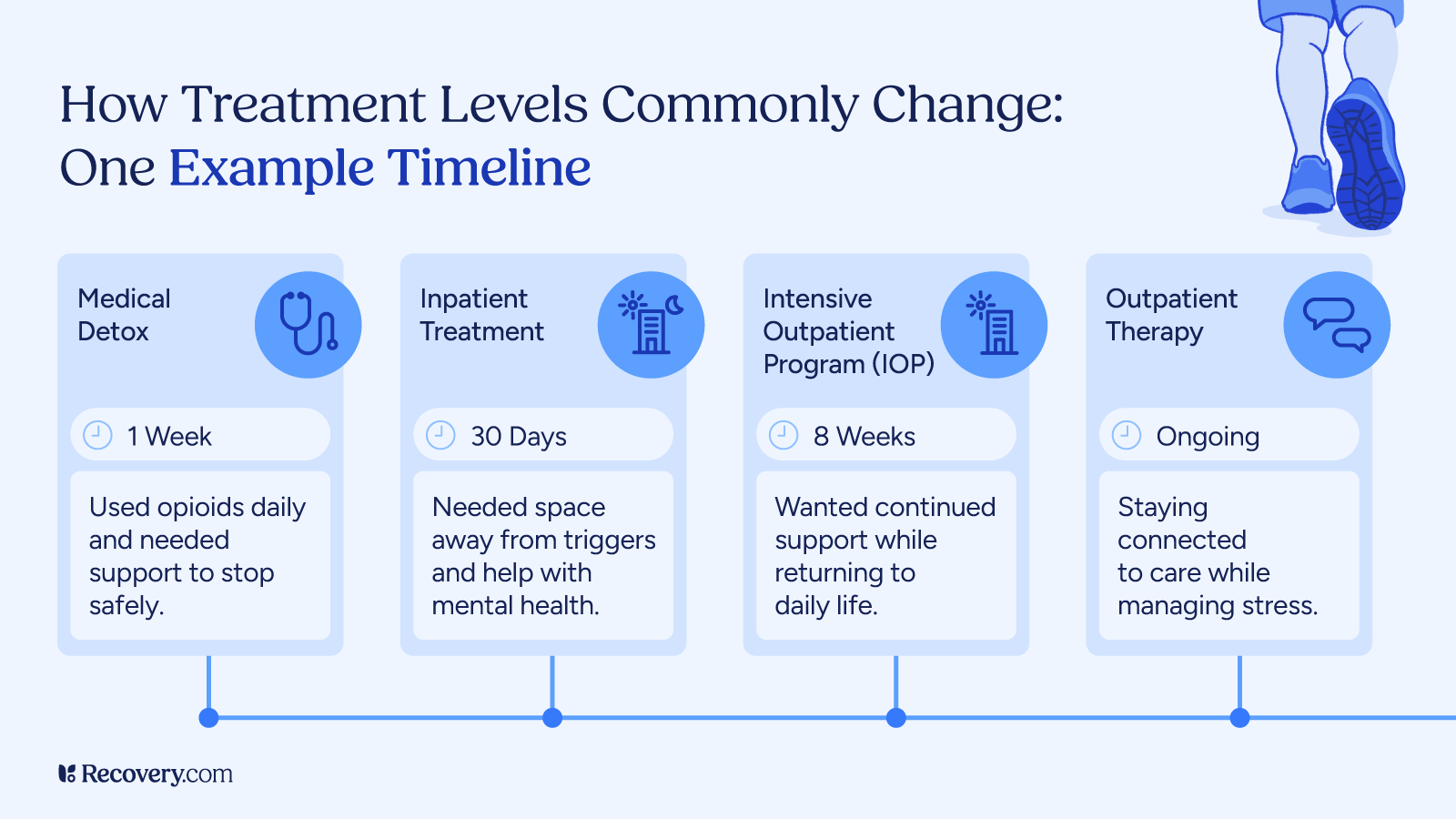
Adjusting Treatment Over Time
You don’t have to commit to one level of care forever; you’ll likely move through several stages of treatment as your needs change. For example, you might start with inpatient rehab as your primary care, then step down to a lower level of care like an IOP, then continue with weekly therapy while living in sober housing.
Recovery isn’t linear. You might go forward, take a step back, or ramp up your meetings or therapy sessions when you’re going through a hard time. That’s normal. What matters most is staying engaged and open to support, even when your path looks different than someone else’s.
Ready to Take the Next Step?
If you or your loved one are thinking about treatment, you don’t have to figure it all out alone. Rehab admissions advisors are usually happy to walk you through your options and help you find a level of care that fits your individual needs.
Use Recovery.com to explore treatment centers near you. You can compare programs, read about their services, and reach out directly.
The right kind of support is out there—you just have to ask for it.
FAQs
Q: What are the levels of care in addiction treatment?
A: Levels of care in addiction treatment include medical detox, inpatient or residential rehab, partial hospitalization programs (PHP), intensive outpatient programs (IOP), sober living, individual therapy, and virtual or telehealth services.
Q: When do you need inpatient treatment?
A: Inpatient addiction treatment is best when you need 24/7 support, can’t stay sober on your own, or are dealing with complex mental health or medical issues.
Q: How does outpatient substance use treatment work?
A: Intensive outpatient programs (IOPs) offer therapy and support on a set schedule—often a few times a week—so you can keep living at home while receiving a high level of therapy and support.
Q: Who needs residential treatment?
A: Residential care is ideal for people who need structure, distance from triggers, or support for a co-occurring substance use disorder and mental health condition.
Q: How long do you need to be in outpatient treatment?
A: It varies. Some people stay for a few weeks while others find long-term support helpful. Your treatment team can help you determine your timeline based on your needs and healing progress.
Q: How do I choose the right level of care for my treatment needs?
A: Your treatment provider can help you determine what level of care you need via an intake assessment. How much support you need will likely depend on your daily functioning, withdrawal risk, mental health, and living environment. When it comes to addiction and mental health treatment, your safety and well-being come first.