If this is a question that you have asked yourself, then you may have an unhealthy relationship with alcohol.
Alcohol dependence can appear differently in everyone. The stereotype of an alcoholic as unemployed and disheveled is just that: a stereotype. Someone struggling with alcohol consumption can have healthy relationships, a successful career, and look great.
However, these positive aspects can quickly deteriorate if an addiction is left untreated. Spotting warning signs early and making changes can help you create a healthier lifestyle.
Understanding Alcohol Consumption
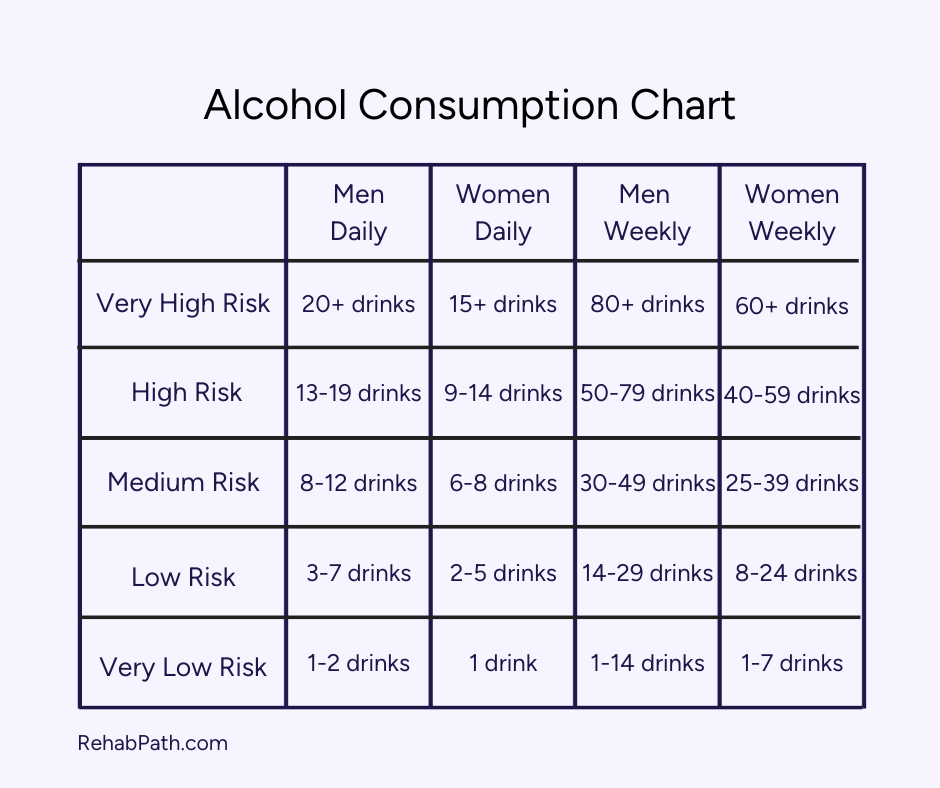
The recommended alcohol consumption and amount that turns excessive varies based on factors such as gender, age, and overall health. To understand your drinking habits, consumption can be split into these categories1:
- Moderate drinking typically refers to up to one drink per day for women and up to two drinks per day for men; however, it is not recommended to drink daily.
- Binge drinking is characterized by consuming a large amount of alcohol in a short period, leading to a blood alcohol concentration (BAC) level of 0.08% or higher. For men, binge drinking usually occurs after consuming five or more drinks within two hours, while for women, it is after four or more drinks in the same timeframe.
- Heavy drinking means consuming more than the moderate drinking guidelines, such as more than one drink a day.
Remember, the healthiest amount of alcohol is no alcohol. If you’re interested in decreasing your regular consumption or giving up alcohol completely, learn more about the sober curious movement.
Alcohol Use Disorder (AUD) is a medical condition characterized by an impaired ability to stop or control alcohol use1 despite adverse social, occupational, or health consequences. AUD can vary in severity, and heavy alcohol use causes lasting changes in the brain that perpetuate AUD and make individuals vulnerable to relapse.
If you currently drink every night and feel it would be hard to stop, it may be time to assess your relationship with alcohol.
Evaluating Your Drinking Habits
Reviewing your alcohol consumption through self-reflection and with the guidance of a medical professional can reshape your lifestyle choices and help you moderate or abstain from drinking.
Frequency of Alcohol Consumption
The National Institute on Alcohol Abuse and Alcoholism (NIAA) does not recommend daily alcohol consumption. Alcohol consumption is entirely advised against special groups, such as pregnant women, those on medication, and those with certain medical conditions.
Drinking every day can deteriorate multiple areas in the body2, including the heart, liver, stomach, and brain. Moreover, it can create a biological need for alcohol3 as the brain and body adjust to daily consumption. The more regularly you drink, the harder it will be to decrease consumption or stop altogether.
Consistent drinking can also interfere with daily responsibilities, relationships, and overall well-being. If you find alcohol is becoming a priority over other activities or obligations, that could indicate a problem.
Quantity and Type of Alcohol
For most people, moderate drinking is inconsistent and includes only a couple drinks at a time. Someone with a healthy relationship with alcohol can have 2 drinks at dinner and then not drink for a number of days.
Excessively drinking any type of alcohol is unhealthy, even though some say that wine is healthier than beer, for example. The best way to maintain well-being is to limit your amount of any type of alcohol. Beer, wine, and spirits are classified as a Group 1 carcinogen4, or a cancer-causing agent—and the more alcohol is consumed, the higher the risk of developing cancer.
Context and Patterns of Drinking
Drinking can become psychologically unhealthy when it’s used to escape uncomfortable feelings. Sometimes, people drink to relieve stress from work, relationships, or other areas of life. Others use it as a social lubricant to feel less inhibited and more outgoing. This can evolve to a solitary activity, frequenting the same bar every week and drinking until drunk every time.
The truth is: Alcohol may help for the moment of unease, but consistent consumption can degenerate physical, mental, psychological, and spiritual aspects of your life. As patterns become habits that soon become unshakable routines, drinking turns into dependence.
Signs of Alcohol Dependence
Your brain and body can indicate if you’re forming an alcohol dependence. The Priory Group, owner of Life Works Rehab in the United Kingdom, breaks down the signs5:
- Secretive or dishonest behaviors related to alcohol
- Drinking heavily in solitude
- Heavy drinking or binge drinking
- Drinking at inappropriate times such as first thing in the morning
- Avoiding contact with loved ones
- Withdrawing from responsibilities at home or work
- Continuing to drink despite the negative effects that this has had on home, work, or social life
- Losing interest in activities that were once important to you
Alcohol dependence can take a toll on the body, including serious, long-term health complications.
The Impact of Regular Drinking
The body can become far too acquainted with alcohol, so much so that it alters the ways organs and systems function. These changes can sometimes evolve to permanency; however, early intervention decreases that risk.
Physical Health Risks
Alcohol consumption impacts vital organs in the body, including
- The Brain: Chronic drinking disrupts neurotransmitters6, the chemical messengers in the brain, impacting the dopaminergic, serotoninergic, glutamatergic, and GABAergic neural circuits. These changes can restructure the brain7, impairing cognitive function, memory, learning, and concentration. Over time, alcohol consumption can even damage gray and white matter8, also known as shrinking brain tissue, thus impacting judgment, decision-making, and coordination.
- The Cardiovascular System: Alcohol use has complex effects on cardiovascular health. Chronic drinking is linked to hypertension, coronary heart disease, stroke, peripheral arterial disease, and cardiomyopathy9. Alcohol raises blood pressure, weakens the heart muscle, and disrupts heart rhythm, all contributing to these diseases that can be life-threatening if not treated.
- The Liver: During normal functioning, the liver breaks down alcohol and other items we ingest into harmless byproducts. If the liver is constantly overwhelmed by excessive alcohol consumption, it can’t metabolize toxins effectively, causing liver cells to accumulate fat10. This process can progress to fatty liver disease, alcoholic hepatitis, and, the most dangerous and permanent, cirrhosis11.
- The Digestive System: Alcohol irritates the stomach’s lining, causing gastritis ulcers12, and small intestines’ lining, leading to an inability to absorb nutrients and a decrease in vital vitamins and minerals. Chronic drinking also triggers the enzymes in the pancreas to activate prematurely13, leading to alcoholic pancreatitis and possibly permanent damage. Importantly, heavy alcohol consumption wreaks havoc on the bacteria responsible for gut health and digestion, creating harmful imbalances. This induces digestive issues as well as negatively affects mental health—the gut microbiome is directly linked to mood disorders14.
As mentioned earlier, alcohol is a cancer-causing agent directly associated with multiple forms of cancer15, including liver, breast, colon, mouth, throat, and more. Researchers hypothesize that multiple factors contribute to the increased risk of cancer, such as
- The metabolization process turns alcohol to acetaldehyde (a dangerous chemical compound).
- The creation of molecules that damage proteins, lipids, and DNA through oxidation.
- The impairment to the body’s ability to break down and absorb various nutrients.
- The increase of estrogen, a sex hormone, is linked to the risk of breast cancer.
Mental Health and Emotional Well-Being
Consistent and excessive alcohol consumption is strongly linked to co-occurring mental health disorders16. The bidirectional relationship between alcohol and mental health can cause complex thoughts and behaviors to untangle—meaning, alcohol use can contribute to the development of mental health disorders, and pre-existing mental health issues can lead to the use of alcohol as a form of self-medication.
While alcohol causes an initial feeling of euphoria or relaxation17, it is a central nervous system depressant18, ultimately leading to adverse changes in mood. The depressing effects lead to chemical imbalances in the brain, contributing to anxiety, depression, and mood swings. Additionally, cortisol, the stress hormone, is released each time you drink19, causing daily anxiety if you are drinking every day.
Someone in the throes of addiction will continue to drink despite the negative effects. The compounding physical and psychological symptoms can be managed through professional treatment and the commitment to stop excessive drinking.
When to Seek Help
Knowing when to get help for drinking can be simple: Once you realize that you have an unhealthy relationship with alcohol, seek out help. The earlier you get professional care, the less likely you’ll need intensive treatment, have lifelong health complications, and have lasting social, emotional, and spiritual consequences.
Recognizing Problematic Drinking
You can ask yourself questions like
- Would you be able to quit drinking right now?
- Has your drinking caused tension or conflict with friends, family, or colleagues?
- Do you miss important events or obligations because you are drinking or hungover?
- Do you use alcohol to cope with stress, sadness, loneliness, or boredom?
- Have friends, family, or co-workers expressed concern about your drinking?
- Have you given up hobbies or activities you used to enjoy because you prefer to drink?
- Are you concerned about where your health and happiness might lead to if you keep drinking at your current rate?
The answers will likely be straightforward and telling if you need medical treatment.
Resources for Assessment
Self-assessment tools, such as online quizzes, can help you gauge whether your alcohol use may be problematic and if you might benefit from professional help. These tools are not diagnostic but can give you a clearer picture of your relationship with alcohol.
Your primary care physician can provide an initial evaluation and refer you to a specialist for a more comprehensive assessment, such as a mental health professional or addiction specialist. During this session, you can ask questions such as
- How is my current level of drinking affecting my overall health?
- What are the signs and symptoms of alcohol dependence I am exhibiting?
- Based on my evaluation, do you believe I have a mild, moderate, or severe alcohol use disorder?
- What kind of treatment do you think I need?
- How can I safely reduce or quit drinking, and what steps should I take to do so?
- Can you refer me to any support groups or resources that might help me?
Treatment Options for Alcohol Use Disorder
As you embark on your recovery journey, you and your care team can explore treatment options to determine the best fit for your individual needs.
Detox
Many people begin their journey by going through the detox process, so you can safely rid your body of alcohol. Medical professionals will be there to ensure you’re as comfortable as possible. This can help you feel more focused and prepared to take on therapy.
It is crucial to detox under medical supervision, as withdrawal symptoms can be life threatening. In some cases, FDA-approved medications can be prescribed, such as Naltrexone and Disulfiram20, to assist the tapering process. Your clinical team can help you decide what treatments and procedures suit you.
Residential Programs
Residential rehab provides an intensive, distraction-free environment to focus on psychotherapies and learning healthy coping skills. Individuals in this stage of care live in the center and have 24/7 support. Ideally, the clinical team creates a personalized treatment plan to address the unique needs of each individual in recovery.
You might participate in evidence-based therapies like cognitive behavioral therapy (CBT) and holistic and alternative healing methods like yoga and massage therapy. The center may provide a blend of individual and group therapy sessions. Your loved ones can engage in family therapy so you can find common ground, improve communication skills, and work towards healthier relationships.
Outpatient Programs
Your care team may recommend an outpatient program if your recovery does not require 24/7 support. Outpatient treatment has varying levels of care, with partial hospitalization (PHP) providing a more intensive level of care and outpatient (OP) providing the least intensive. You’ll participate in the program for a few hours a day on certain days of the week, allowing you to go to work or attend school simultaneously. You’ll likely participate in therapies similar to a residential program and build your support network as you heal with others in therapy.
Support Groups
Joining support groups like Alcoholics Anonymous and SMART Recovery provide a sense of community, understanding, and accountability in your recovery. They offer a safe space to share experiences, learn from others, and receive ongoing support.
Building a Support Network
Creating a support network with strong relationships is a foundational aspect of long-lasting recovery. Social support in recovery can reduce stress, increase self-efficacy, and motivate lasting sobriety21. Your relapse prevention plan can detail how you will connect with loved ones who supported you through the treatment process. You may make new friends through sober activities and groups. Try your best to plan regular get-togethers with friends and family, as avoiding isolation and bolstering these relationships can make recovery easier.
Setting and communicating boundaries in recovery is a practice of self-love and can enhance your relationships. Without boundaries, you may say “yes” to things you don’t want to, avoid necessary conversations, and be consumed by others’ negative feelings. Prioritizing your boundaries ensures you’re aligned with what’s best for your well-being.
Preventing Relapse
Not everyone in recovery will relapse, but it can be a part of the recovery process22—and that’s okay. Relapse prevention can help you address these obstacles and keep you on the right track.
Relapse prevention planning aims to recognize and address these warning signals before they escalate to the physical stage—drinking after a period of sobriety. It takes a cognitive behavioral approach to prevent relapse and provides appropriate skills on what to do if a relapse does occur. Relapse prevention blends education, coping strategy development, trigger identification, building support networks, and lifestyle changes.
You and your care team can begin to build your relapse prevention plan by reflecting on 3 key recovery components:
- Reflect on your recovery history. In treatment, what worked and what didn’t work? If you’ve relapsed before, what led to it? What were your triggers before you got treatment? Learn from mistakes of the past to make a realistic relapse prevention plan.
- Write down personal, relationship, and employment goals to highlight situations you want to be in and people you want to be around.
- Identify your triggers—all the people, places, and things that could cause stress. Developing coping strategies for each trigger can empower you to live life without fear.
One of the most essential parts of a relapse prevention plan is building skills to navigate uncomfortable feelings and situations. You may practice coping techniques such as breathing exercises, regulating emotions through journaling, and saying “no” to situations that do not serve your recovery. This can help you walk into any situation with confidence.
Attending outpatient care or talk therapy sessions can help you navigate foreign situations and continue skill-building. During individual therapy sessions, you’ll likely engage in various therapeutic methods like dialectical behavior therapy (DBT) and acceptance and commitment therapy (ACT).
Creating a daily routine that promotes physical and mental health, including regular exercise, balanced nutrition, and sufficient sleep, can bolster sustainable recovery23. A scheduling system, such as time blocking in a calendar, can help you avoid idle time that might lead to thoughts or behaviors associated with relapse.
A day of sobriety is a day worth being celebrated! The effort to choose your health and well-being every day is a great feat, so continue to reflect and pride yourself on your hard work.
A Step in the Right Direction
If you feel like you can’t drink at a healthy pace and use alcohol to cope with uncomfortable feelings, it might be time to seek treatment. You can discover and sustain a healthy and balanced lifestyle that prioritizes your well-being. Embrace a life without alcohol. Begin your search by browsing our list of alcohol addiction treatment centers.

