Welcome to Recovery Reach, the podcast for behavioral health leaders looking for specific marketing and business tactics that can scale their impact.
Supporting Men’s Mental Health: 9+ Insights to Break Stigma and Build Connection
This article is a summary of a heartfelt conversation from the Giving Voice to Depression podcast, hosted by Terry McGuire. Each week on the podcast, Terry shares honest, vulnerable conversations with people who live with depression, as well as experts and professionals who offer insights into mental health challenges and recovery.
In Episode 358: “Rebranding MENtal Health,” Terry and her guest co-host — social worker and educator Carly McCollow — sit down with Ethan Getchell, a mental health counselor whose life took a profound turn after the suicide of his brother. What followed was a journey from grief to purpose, as Ethan dedicated himself to rethinking how we approach men’s mental health.
This episode doesn’t just explore why men struggle to open up; it offers practical, compassionate strategies to meet them where they are. Below, we explore 9+ powerful insights from this conversation that can help us all better support the men in our lives — and remind anyone struggling that they are not alone, and there is always a path forward.
1. Recognize the Cultural Scripts That Shape Men’s Mental Health
Many of us grew up with stories — from movies, TV, even childhood role models — about the tough, independent man who can handle anything on his own. Ethan explains that in the U.S., the idea of the “lone cowboy” or the rugged individualist is deeply ingrained.
Ethan Getchell says:
We haven’t been taught how to build our tribe and community, or how to be vulnerable and emotional.
But the truth is, no one can or should go through life alone. The image of the man who never needs help leaves many men isolated when they inevitably face hardship.
Compassionate reminders:
- Strength is not about facing pain alone — it’s about knowing when to reach out.
- Vulnerability isn’t a flaw; it’s part of being fully human.
- We can all help break the cycle by inviting and normalizing emotional connection.
2. Understand That Isolation Amplifies Depression
The COVID-19 pandemic showed just how fragile many people’s mental health really is — especially for men who were used to distracting themselves with work, hobbies, or sports.
Ethan says:
That’s where covert depression really takes its biggest form … when you’re isolated in your house, you’re forced to sit with your thoughts.
When the distractions fall away, many men realize they’ve been carrying unspoken pain for a long time. But without support systems or emotional tools, they may feel stuck or overwhelmed.
Encouraging takeaways:
- It’s never too late to start building connection and emotional resilience.
- Even small steps toward connection — a check-in with a friend, joining a group, talking to a counselor — can break the spell of isolation.
- You don’t have to wait for crisis to start caring for your emotional health.
3. Therapy Needs a Makeover — and We Can Help
Ethan makes an important point: many men avoid therapy because they don’t like how it’s been “sold” to them.
Ethan says:
Why aren’t we getting men into therapy? It’s because the marketing in what men conceptualize and think of when they hear therapy kind of sucks right now.
He points to campaigns like Man Therapy, which use humor and relatable imagery — like “A mustache is no place to hide your emotions” or “Never ignore your mind’s check engine light” — to make mental health care approachable and less intimidating.
We all have a role in this rebranding. Whether you’re a therapist, a friend, or a loved one, the language you use matters.
Ways to help reshape the narrative:
- Frame therapy as a strength, not a sign of weakness.
- Highlight practical, goal-oriented approaches (more on that below!).
- Celebrate men who share their stories — like Ethan — as role models, not exceptions.
4. Focus on Actionable Behaviors, Not Just Emotions
For some men, the idea of sitting face-to-face in a therapy room talking about feelings is daunting. Ethan adapts his therapeutic approach by starting with behavioral change — something concrete and measurable.
He uses tools like the Habit Share app (which he emphasizes he has no affiliation with) to help clients track daily habits and build momentum.
Ethan says:
You start to acknowledge that your thoughts are influencing you, affecting you — and it’s done through a rebranding and communication style that says, ‘Hey, we’re doing therapy right now, and it’s not hurting you.’
By focusing on behaviors — eating well, exercising, maintaining routines — Ethan helps clients strengthen their mental health in a way that feels tangible and nonthreatening.
Practical tip: Focus first on what you do, and let deeper emotional insights follow naturally over time.
5. Mind the Core Four Elements: Earth, Water, Fire, Air
In moments of darkness or overwhelm, it’s easy to neglect the basics — but those basics are the foundation of well-being. Ethan uses the metaphor of the four elements to help his clients remember what matters most:
- Earth → Eating (nourish your body)
- Water → Hydration (stay hydrated)
- Fire → Movement (get moving, exercise)
- Air → Breathing (practice calm, meditate, pray)
Ethan says:
The first step to making it better is taking care of the things that sustain your life. In Maslow’s hierarchy, take care of your basic needs first. Even when they’re in a heightened state, they can come back to those four.
These simple, grounding checks can make all the difference when someone feels untethered or overwhelmed.
Encouraging reminder: You don’t have to solve everything today. Start with the basics, and build from there.
6. Know There’s a Time for Crisis Management — and a Time for Growth
Ethan explains that therapy often unfolds in two phases:
- Crisis Management — When someone is struggling acutely (suicidal thoughts, intense depression), the focus is on stabilizing and protecting life.
- Exploration and Growth — Once stability returns, deeper work begins: exploring strengths, reflecting on identity, setting goals, and imagining a hopeful future.
Ethan says:
Once you’re not putting out fires, you can start to explore … then you start to learn some of your strengths, weaknesses, passions.
This compassionate framing reassures us that needing crisis help is not failure — it’s the first courageous step on a longer, richer journey.
7. Listening is an Act of Love
One of Ethan’s most profound observations is that many young men come to therapy because they don’t have anyone else who truly listens.
Ethan says:
It’s amazing how with just enough persistent, patient listening, you can get them to come out of their shell.
If you have a man in your life who’s struggling, remember: you don’t need to fix him. You don’t need to lecture or advise. You just need to show up, stay curious, and hold space.
Loving ways to listen:
- Ask open-ended questions.
- Resist the urge to immediately problem-solve.
- Offer reassurance: “You might stumble, but it’s not the end.”
8. Reimagine How We Invite Men Into Support
It’s common to hear people say things like “Dude, you need therapy,” — but that kind of framing can feel shaming or accusatory. Carly highlights how shifting the invitation can make all the difference.
Instead of confronting, try:
- “Hey, you seem overwhelmed. Do you have someone you can talk to?”
- “You’ve been carrying a lot lately — want help finding support?”
As Carly McCollow says:
Even if we change our tone, the voice inside that person’s head might still hear judgment. But if we frame it as concern and care, it’s easier to accept.
The goal isn’t to push people into therapy — it’s to remind them they deserve care, connection, and support.
9. Create Shoulder-to-Shoulder Spaces
Direct, eye-to-eye conversations can feel intimidating — especially when emotions are involved. Ethan and Carly both emphasize the power of shoulder-to-shoulder connection:
Terry McGuire says:
It’s easier to talk when you’re not looking eye to eye … if you’re in the car, or shooting hoops, or walking together.
These parallel spaces lower defenses and make vulnerability feel safer.
Examples:
- Going for a walk together.
- Joining a dads’ “stroller club.”
- Sharing a drive, or doing an activity side by side.
These aren’t just casual hangouts — they’re quiet invitations to share, support, and remind someone they’re not alone.
+1 Bonus: Remember, Everyone Needs Support During Life Transitions
Job loss, relationship changes, illness, parenthood — these life transitions can shake even the most grounded people. Therapy and community support aren’t just for “crisis” moments; they’re tools we can all lean on to navigate life’s ups and downs.
Terry says:
You don’t have to be embarrassed. Therapists have heard it before … they hear regularly from people who have really hard times with all kinds of things.
Let’s break the chain: when we get support for ourselves, we ripple that healing outward to the people we love.
Final Reflections on Men’s Mental Health
This episode of Giving Voice to Depression offers a deeply hopeful and uplifting reminder that meaningful change is not only possible on the individual level, but also across families, communities, and our broader culture. By opening up conversations that challenge outdated ideas about masculinity, strength, and emotional resilience, we begin to create a society where mental health struggles are met with understanding, not judgment.
As Terry so thoughtfully says, these are not merely “difficult” or “uncomfortable” conversations — they are necessary ones. When we rethink how we present therapy, when we invite men into spaces of support with genuine compassion, and when we work intentionally to make vulnerability feel safe rather than shameful, we take important steps toward building a world where no one feels they must suffer silently or carry their burdens alone.
If you or someone you care about is navigating mental health challenges, please remember this: you don’t have to walk this road in isolation. There are caring people ready to listen, to stand beside you, and to remind you — again and again — that healing is not only possible, but that you are deserving of it. You are worth the care, the support, and the hope that recovery can bring.
Xanax Withdrawal Symptoms: What to Expect and When to Get Help
If you take Xanax, it’s important to understand how your body can become dependent on it and what happens when you stop. Xanax (alprazolam) is a medication doctors often prescribe for certain mental health conditions like anxiety and panic disorders.
While it can be helpful for managing severe anxiety in the short term, if you continue taking Xanax, it doesn’t take long for your brain to start relying on it. When you cut back or stop taking Xanax, your body needs time to adjust—and that’s when withdrawal symptoms can show up.
Xanax withdrawal can feel anywhere from uncomfortable (like a bad flu) to very tough to handle but knowing what to expect can help you prepare and get through it safely. Let’s look at what happens during withdrawal, the symptoms you might experience, and how getting the right support can make all the difference.
IMPORTANT NOTE: Never attempt Xanax detox without medical support. Withdrawing from Xanax on your own can be dangerous and potentially life-threatening, with risks including seizures and psychosis in severe cases. When you’re ready to stop taking Xanax, always consult with a healthcare provider first, never stop “cold turkey,” and follow a medically supervised tapering schedule that gradually reduces your dose over time. Even if you’ve been taking Xanax exactly as prescribed, your body may have developed a physical dependence that requires careful management during discontinuation.
Medical supervision ensures you can withdraw safely while managing symptoms effectively, providing tools and medications that make the process much more comfortable and significantly safer than attempting it alone.
What Is Xanax and Why Does Your Body Become Dependent on It?
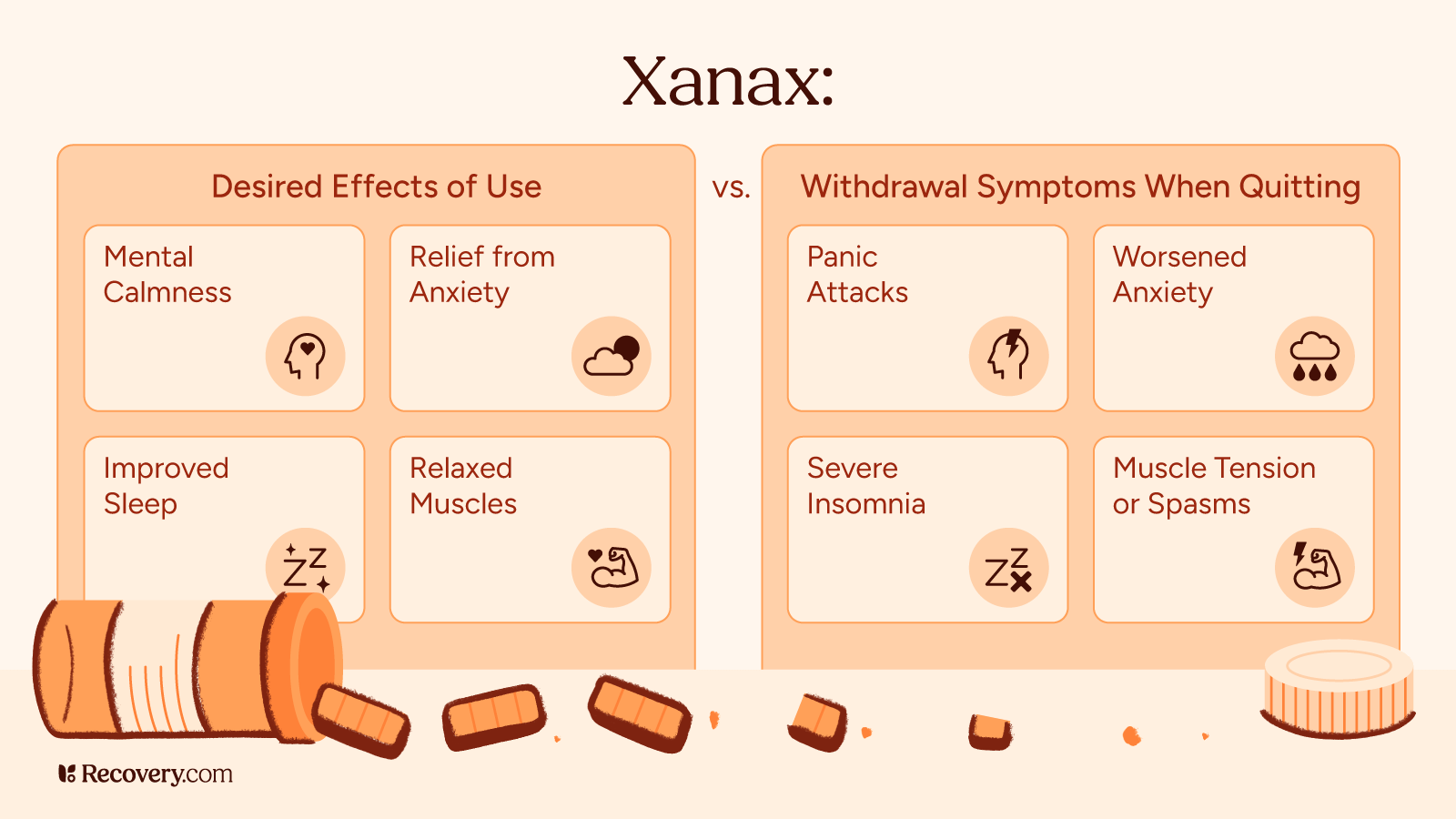
Xanax belongs to a family of medications called benzodiazepines1 (or “benzos” for short). These medications work by boosting a natural calming chemical in your brain called GABA. When you take Xanax, it slows down your overactive brain, which helps reduce anxiety and panic attacks. That’s why it can make you feel relaxed, sleepy, and less bothered by stress.
Physical Dependence: When Your Body Expects Xanax
Because your brain is designed to adapt quickly, it quickly gets used to having Xanax around. After just a few weeks of regular use, your brain starts making less of its own calming chemicals because it’s counting on the medication to do the job instead.
Doctors call this dependence. It means your body has gotten used to functioning with Xanax in your system.
You can become dependent on Xanax even if you’re taking it exactly as prescribed.2 Physiological dependence can happen in as little as 3-4 weeks of regular use, even at normal doses. That’s why doctors usually only recommend Xanax for short periods. The more you take and the longer you use it, the more your body comes to rely on it.
Addiction: When Xanax Takes Control
Addiction is different from dependence. While dependence is about your body physically adapting to the drug, addiction involves behaviors like taking more than prescribed, seeing multiple doctors to get extra prescriptions, or continuing to use Xanax despite the problems it’s causing in your life.
Not everyone who becomes dependent develops a substance use disorder, but the longer you take Xanax, the more your risk of addiction increases.3
What Happens During Xanax Withdrawal?
When you stop taking Xanax, your brain needs to remember how to work on its own again. During this adjustment period, you might feel uncomfortable as your brain tries to restore its natural balance. That’s because your brain is relearning how to calm itself down without chemical help.
Common Xanax Withdrawal Symptoms
When you stop taking Xanax, you can experience several different kinds of symptoms. Here’s what you might feel and why it happens.
Physical Symptoms: How Your Body Reacts
The physical symptoms of Xanax withdrawal4 can feel a lot like having a bad flu or hangover. You might notice:
- Headaches, dizziness, or lightheadedness
- Fever or sweating more than usual
- Muscle spasms, aches, or shakiness
- Blurry vision or sensitivity to bright lights
- Nausea or stomach pain
- Having a hard time falling or staying asleep
- Heart palpitations or increased heart rate
- Higher blood pressure
Your body might feel extra sensitive during withdrawal, so everyday lights and sounds that normally wouldn’t bother you might suddenly feel too bright or too loud. This happens because Xanax is a central nervous system depressant, and without it, your nervous system has to work overtime to calm things down.
Mental and Emotional Symptoms: How Your Mind Reacts
Withdrawal can also affect how you feel emotionally and mentally. You might:
- Feel more anxious or have panic attacks (sometimes worse than before)
- Have mood swings or get irritated easily
- Feel mentally foggy or have trouble concentrating
- Feel down or hopeless
- Have racing thoughts
- Have strong cravings for Xanax
- Feel easily overwhelmed
You might notice that some withdrawal symptoms feel similar to the anxiety disorder you were taking Xanax for in the first place. This “rebound anxiety” is common and doesn’t mean your anxiety is getting worse permanently—it’s just part of the withdrawal process and will improve with time.
Serious Withdrawal Symptoms: When to Get Immediate Help
In some cases—especially after heavy or long-term use—Xanax withdrawal can cause more serious symptoms. If you experience any of these, you should seek medical attention right away:
- Seizures
- Seeing or hearing things that aren’t really there
- Severe confusion about where you are or what’s happening
- Losing touch with reality
These severe symptoms are more likely to happen if you stop Xanax suddenly5 (“cold turkey”) instead of gradually reducing your dose under a doctor’s guidance. This is why getting help from a medical professional during withdrawal is so important, especially if you’ve been taking higher doses or using Xanax for a long time.
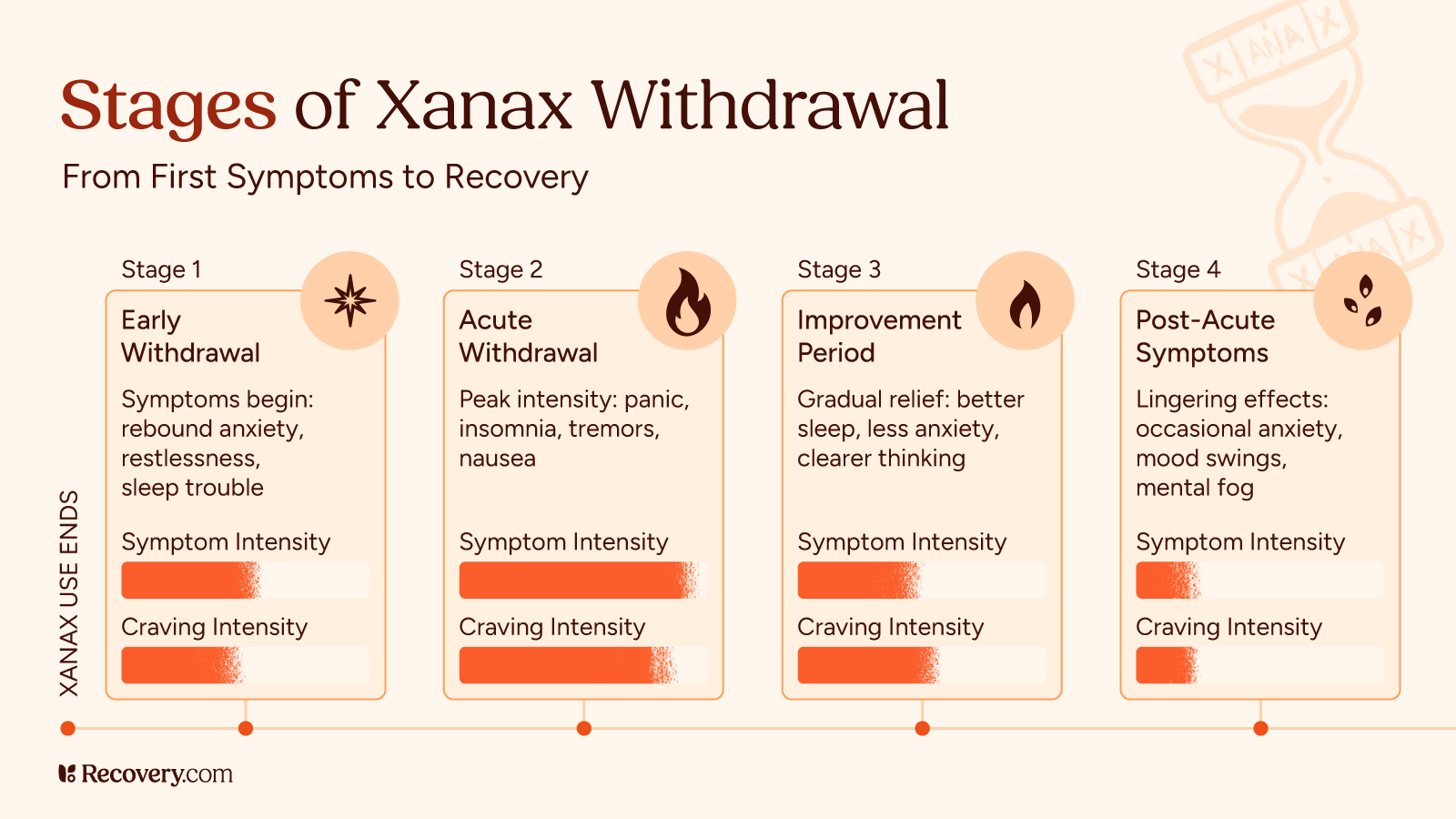
When Will I Feel Better? The Xanax Withdrawal Timeline
No two people experience Xanax withdrawal exactly the same way, but there is a general pattern most people follow. Knowing what to expect and when can help you prepare and get the right support for your situation.
Early Withdrawal (1-4 Days After Your Last Dose)
Xanax withdrawal symptoms6 often kick in within 1-4 days after your last dose. Since Xanax is a short-acting benzodiazepine, it has a shorter half-life than many other benzos. This means you’ll likely notice symptoms starting sooner rather than later. During these first few days, you might experience:
- “Rebound” anxiety that might feel stronger than your original anxiety
- Trouble falling or staying asleep
- Feeling restless or on edge
- Irritability or mood changes
These early symptoms happen as your body first notices the absence of Xanax in your system.
Acute Withdrawal (Days 5-14)
The full-blown withdrawal syndrome typically lasts about 10-14 days. During this period, you might deal with:
- Increased anxiety and possible panic attacks
- Sleep disturbances and nightmares
- Physical symptoms like tremors, sweating, and nausea
- Difficulty concentrating or thinking clearly
- Muscle pain and stiffness
- Headaches and sensitivity to light
- In more severe cases, possible seizures7 (which is why medical supervision is crucial)
This acute phase is when symptoms are typically most intense and when medical support is most important, especially if you’ve been on higher doses or taking Xanax long-term.
Improvement Period (After Week 2)
After the acute withdrawal phase, most people start to see gradual improvement. During this time, you might notice:
- Symptoms becoming less intense and more manageable
- Better sleep quality
- Decreasing anxiety levels
- More good days than hard ones
For some people, symptoms resolve completely within a few weeks. For others, some symptoms may persist longer.
The Long Haul: Months Later
Some people deal with lingering symptoms for months after stopping Xanax.8 Doctors call this post-acute withdrawal syndrome (PAWS). If this happens to you, you might experience:
- Occasional anxiety or panic attacks that come out of nowhere
- Nights where you just can’t sleep well
- Mood swings that seem to have no trigger
- Feeling mentally foggy or having trouble thinking clearly
The good news is these protracted withdrawal symptoms usually get milder and show up less often as time passes. For most people, they eventually go away completely, though it might take several months.
To learn more about long-term side effects, see our complete guide to post-acute withdrawal syndrome (PAWS) and how to manage these lingering symptoms.
Factors That Affect Your Withdrawal Experience
How long your withdrawal lasts and how severe it is depends on several factors:
- How much you were taking: Higher doses usually mean more severe withdrawal symptoms.
- How long you were taking it: Months or years of use means a longer recovery.
- How you stop: Gradually reducing your dose (tapering) under medical supervision causes fewer problems.
- Your personal health factors: Your age, overall health, and body chemistry matter.
- Past experiences: If you’ve gone through benzo withdrawal before, your body might be more sensitive.
This timeline is just a general roadmap. Your personal journey might look different, and that’s okay.
Xanax Detox and Recovery: Find Help for the Journey Ahead
Withdrawing from Xanax can be challenging, but with the right support and care, it’s a journey you can take on successfully. Keep in mind that the discomfort of withdrawal is temporary, and plenty of people have gone through this process and emerged stronger on the other side.
If you or your loved one is considering quitting Xanax, the first step is to speak with a healthcare professional. A qualified addiction medicine specialist can assess your situation and create a personalized treatment plan that may include inpatient or outpatient rehab and support groups. Don’t try to go through this alone—professional support is hugely important for your safety and comfort during withdrawal.
For help finding treatment options, search for specialized Xanax addiction treatment programs in your area. Recovery is possible, and support is available whenever you’re ready.
FAQs
Q: When might I experience withdrawal symptoms from benzodiazepines?
A: Withdrawal symptoms can begin within 6-12 hours after your last dose of Xanax, which has a shorter half-life than many other benzodiazepines. Symptoms often peak within 2-4 days.
Q: How long do Xanax withdrawal symptoms last?
A: Acute withdrawal symptoms typically last 1-2 weeks, but some people experience milder, lingering symptoms for several weeks or months. The timeline varies based on dosage, duration of use, and individual factors.
Q: Is it safe to detox from Xanax at home?
A: Home detox can be dangerous, especially after long-term or high-dose use. Always consult with a healthcare provider before attempting to stop taking Xanax. Medically supervised detoxification is strongly recommended for most people quitting Xanax.
Q: Where can I find a Xanax detox clinic?
A: You can find medical detox facilities by using our treatment finder at Recovery.com.
Q: What is the best way to manage Xanax withdrawal symptoms?
A: The safest approach is a medically supervised gradual taper, combined with supportive medications for specific symptoms, therapy, and self-care practices. Suddenly stopping Xanax use is never recommended.
Maureen’s Journey in Eating Disorder Recovery and Self-Love
The Giving Voice to Mental Health Podcast recently shared a deeply personal story of resilience with Maureen, who recounted her journey through an eating disorder that began during her time as a ballet dancer in the 1980s. Her powerful narrative offers crucial understanding and hope for individuals facing similar challenges and those who support them. Hosts Terry McGuire and Caroline Beidler guided a conversation that illuminated the isolation of struggling with an eating disorder when awareness was limited, contrasting it with the growing resources available today.
More Than Just Food: Understanding the Core of Recovery
Maureen thoughtfully described her experience not as a “battle,” but as “working through” an eating disorder. This highlights the ongoing and internal nature of recovery, extending beyond just physical health to encompass self-image, self-esteem, and, most importantly, self-love.
“I feel that I am recovering from a combination of… not understanding how to take care of myself. It’s beyond the amount of food that you put in your body, for example, it’s really about self-image and self-esteem and self-love…”
Her words emphasize that true recovery involves a fundamental shift in how one perceives and values themselves.
The Weight of External Expectations: Body Image and Triggers
As a ballet dancer in the 1980s, Maureen faced immense pressure regarding her body image. This environment became a significant trigger, highlighting how external expectations can contribute to the development of eating disorders.
“As a young person in college, I was a dancer, a ballet dancer in the 1980s and at that time, body image was a huge thing and you had to look a certain way and be a certain way in order to perform…”
This experience underscores the importance of recognizing and addressing societal and environmental factors that can fuel disordered eating.
A Long and Winding Road: The Reality of Ongoing Recovery
Maureen’s journey to self-acceptance has spanned decades, illustrating that recovery is rarely a straight path. It involves continuous effort, with challenges and negative thoughts potentially resurfacing.
“It’s taken me this much of my life to arrive at being okay with myself, you know? And even that gets challenged all the time… I’m always in recovery. I’m always working on recovery.”
Her strength lies in her ability to identify unhealthy patterns and consciously choose a healthier direction, affirming, “You’re okay. You’re good just the way you are.”
Explore eating disorder treatment options.
The Harmful Words: What Not to Say to Someone Struggling
Well-intentioned but misguided advice, such as “just eat more,” can be detrimental to someone with an eating disorder. Maureen emphasized the importance of avoiding comments about food altogether.
“Teachers didn’t really know what to do with me. They didn’t know what to say. They just kept saying, well, you have to eat more. You have to eat more. It’s not what, it’s not the right thing to say… Don’t say anything about food. Leave it alone and let me figure it out.”
Instead, she suggests expressing non-judgmental support and focusing on aspects of their life unrelated to food or body image. Suggesting alternative activities, like “Let’s go for a walk,” can be far more helpful.
Finding Support: The Power of Connection
While formal therapy wasn’t consistently available to Maureen in the early stages, she found crucial support in friends, particularly within the modern dance community, which offered a more accepting environment. This highlights the significance of supportive relationships in recovery.
“I found support in friends and interestingly in among dancer friends… I found a really wonderful, supportive community there.”
The lack of readily available professional help in the 1980s underscores the progress made in providing resources today.
A World of Options: Hope for Today and Tomorrow
Maureen reflected on the lack of treatment options available when she was struggling, a stark contrast to the resources that exist now. Today, individuals have access to information, various therapies, peer support groups, and treatment facilities.
“If it happened to me now, I wouldn’t hesitate to look around for a place to go, you know, somebody to talk to or a situation to take care of myself…”
Caroline emphasized the wealth of information available on https://recovery.com/resources/ and the importance of educating ourselves and others about eating disorders and available support.
Embracing Life: Finding Joy in Self-Acceptance
Maureen’s journey ultimately led her to a powerful realization: life is truly good when you treat yourself with kindness and embrace self-acceptance.
“Oh. ’cause life is so good when you’re, when you’re able to treat yourself well. When you’re able to love yourself and accept yourself, life is really, really great.”
This message of hope and the possibility of a more positive and vibrant life serves as an encouragement for anyone currently struggling to believe in their own potential for recovery and self-love.
Anorexia vs. Bulimia: Knowing These 4 Key Differences Can Improve Your Recovery
You might think anorexia and bulimia are pretty much the same thing, but actually, they work in very different ways. Learning about these differences isn’t just about knowing medical facts—it can help you spot warning signs in yourself or someone you care about.
Let’s look at how anorexia and bulimia compare and what physical signs, behaviors, thinking patterns, and health risks are unique to each condition. We’ll also explain treatment options and where to find help, whether you’re trying to understand your own experiences or are concerned about a loved one.
Before getting into the specific differences between anorexia and bulimia, what exactly is an eating disorder, and what makes them so serious?
What Are Eating Disorders?
Eating disorders are serious mental health conditions that involve harmful eating habits and troubling thoughts about food and eating, as well as distorted body image. About 9% of people in the U.S. will have an eating disorder in their lifetime.1 Women and girls are diagnosed more often, but anyone can develop these conditions.
Anorexia nervosa and bulimia nervosa are 2 of the most well-known eating disorders. They share some features but work differently in terms of eating behaviors, symptoms, and health effects. Other types include binge eating disorder and avoidant/restrictive food intake disorder (ARFID).
Eating disorders aren’t choices or phases—they’re complex conditions influenced by genes, biology, psychology, and social factors. They can seriously harm people’s physical health, emotional well-being, and everyday life. But with quality treatment and support, people can and do recover—though that journey looks different for each person.
Anorexia Nervosa: Key Characteristics
Anorexia involves severely limiting food and having an intense fear of gaining weight, even when you’re already underweight. People with anorexia usually see their bodies differently than others do. For example, they may think they look fat even when they’re actually very thin.
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR), to be diagnosed with anorexia,2 someone must eat so little that they’re at an unusually low weight, be terrified of gaining weight, and have a distorted view of their body. There are 2 main types: The restricting type (mostly limiting food) and the binge-eating/purging type (restricting but sometimes also bingeing and purging).
Physical signs of anorexia3 include:
- Extreme weight loss
- Always feeling tired or dizzy
- Complaining about being cold all the time
- Development of fine hair all over your body
- Constipation
- Brittle nails
- Dry skin
- Stopped menstruation
Many people who struggle with anorexia create strict food rules, like cutting food into tiny pieces, only eating at certain times, or avoiding meals with others.
The mental side often includes:
- Constantly thinking about food, calories, and weight
- Feeling a sense of control or achievement when restricting food
- Difficulty recognizing how serious your condition is
- Reluctance to ask for help
How can clinicians better identify bulimia given its “hidden” nature compared to the more visible signs of anorexia?
Being direct and sensitive when asking about binging or purging is important. It can be easy to dance around the topic, but it’s important to bring light to it in sessions so clients can be challenged. There is a delicate line to balance here, and it can be managed with tone, building trust, and appropriate timing. Clinicians can also ask about their recent diet history and exercise patterns. This may not directly or completely uncover behaviors, but it can be a leading indicator of areas where there may be some concerns.
Silvi Saxena, MBA, MSW, LSW, CCTP, OSW-C
Bulimia Nervosa: Key Characteristics
Bulimia involves cycles of eating huge amounts of food (binging) and then trying to prevent weight gain through behaviors like throwing up. During binges, someone eats an excessive amount of food in a short window and feels like they can’t stop or control their eating.
After binging, people with bulimia try to “undo” the calories they ate by making themselves throw up, taking laxatives or diuretics, fasting, or exercising too much. Unlike people with anorexia, those with bulimia usually stay at a normal weight or slightly above, which makes the condition a lot harder for others to notice.
Physical signs of bulimia4 might include:
- Puffy cheeks
- Dental problems from stomach acid
- Calluses on knuckles from self-induced vomiting
- Weight that fluctuates up and down
- Stomach problems
- Imbalanced electrolytes
- Acid reflux
- Chronic sore throats
- Heartburn
The binge-purge cycle often happens in secret and makes people feel disgusted, guilty, or ashamed. Despite these negative feelings, the cycle is hard to break because both binging and purging can temporarily make emotional pain feel better. Like anorexia, bulimia involves intense worry about body shape and weight, but the approach to food is very different.
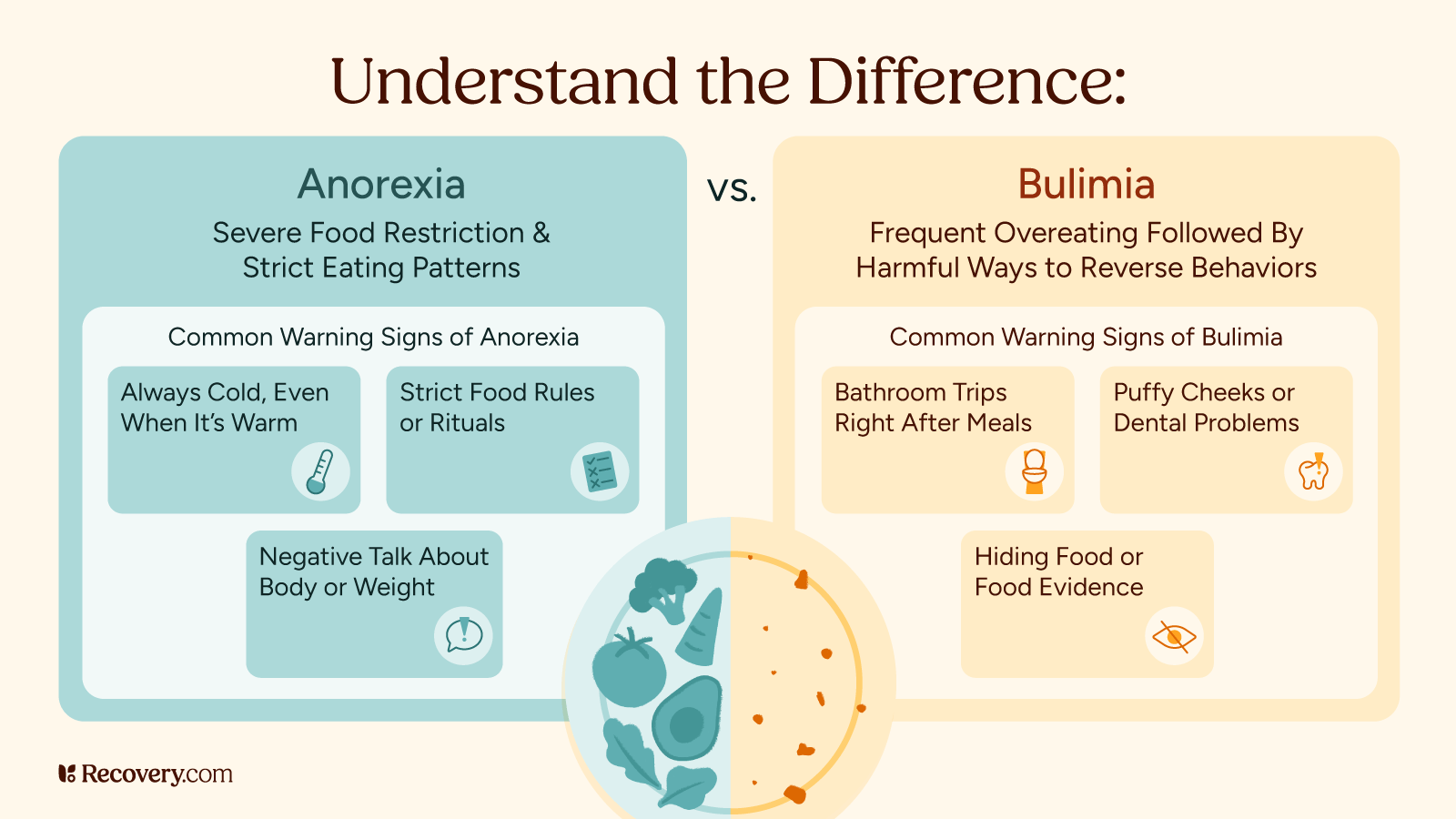
Major Differences Between Anorexia and Bulimia
Physical Appearance
The most obvious difference is how people with these disorders typically look. Those with anorexia are usually very underweight, while people with bulimia may maintain their normal weight or be slightly overweight. This means you can often see anorexia, while bulimia can stay hidden for years.
Eating Patterns
The eating patterns are also quite different. People with anorexia mainly restrict their food intake,5 eating very little or avoiding certain foods completely. People with bulimia swing between episodes of binge eating (eating large amounts of food at a time) and compensatory behaviors to try to get rid of those calories.
Relationship to Food
These conditions cause different feelings about food, too. People with anorexia tend to create strict rules about food and may feel anxious about eating. Those with bulimia typically feel out of control during binges, often eating foods they normally avoid, then desperately trying to counteract what they’ve eaten.
Emotional Experience
The emotional experience is different as well. Anorexia often brings a sense of accomplishment from restricting food and losing weight, while bulimia usually involves intense shame around binging and purging.
Binge eating disorder (BED) and orthorexia survivor Elisa Aas describes how shame fueled the cycles of her disordered eating:6
You feel you abused food and your body so much you don’t deserve to enjoy food again.
Both of these conditions make people feel unhappy with their bodies, but how that shows up in behaviors is quite different.
Finding and diagnosing these disorders also follows different paths. Anorexia tends to be diagnosed earlier on7 because of visible weight loss, while bulimia’s secretive nature and normal-looking weight make it harder to notice from the outside. This difference can affect how quickly someone gets help, and what kind of help they need.
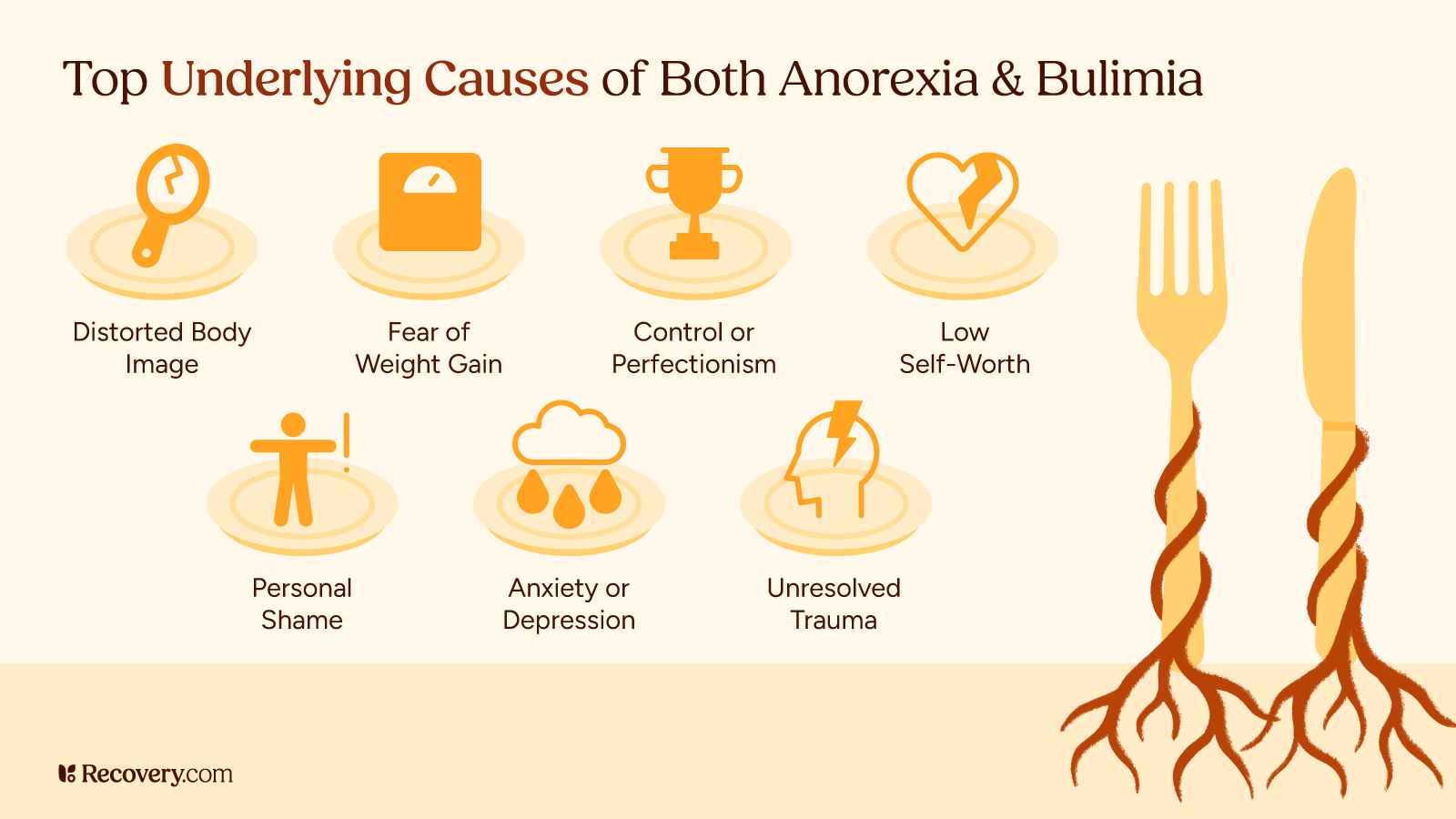
Key Similarities Between Anorexia and Bulimia
Though they may look different, anorexia and bulimia have important similarities. Both involve judging your self-worth largely based on your weight and body type. People with either condition often measure their value as a person by how they look8 or how well they can control their eating.
Risk Factors
Both anorexia and bulimia can come from similar risk factors,9 including genetics, personality traits like perfectionism, history of dieting, and cultural pressures around thinness. Traumatic experiences, family dynamics, and other mental health issues like anxiety or depression can contribute to both disorders.
What are the most promising developments in eating disorder treatment that address both the physical and psychological aspects of these conditions?
The most promising development I have seen in eating disorder treatment for Anorexia and Bulimia is the increase in adoption of the Health at Every Size Approach. So often, patients living in larger bodies have fallen by the wayside due to the stereotypes of what an eating disorder ‘should look like,’ when eating disorders are, first and foremost, mental illnesses that have a physical impact.
By treating the physical impacts of the disorder but not using them to determine the severity of one patient’s condition over another, and incorporating a variety of therapies (such as DBT, ACT, CBT, and family therapy), eating disorders are being treated at all angles. As a person in recovery who has lived in a larger body for most of my life, paired with my professional experience, I have witnessed how the Health at Every Size Approach leads to creating more inclusive treatment plans and lasting positive outcomes.
Sage Nestler, MSW | Releasing the Phoenix
Coping Mechanisms
There’s significant overlap between eating disorders,10 especially among people with anorexia. One study found that of the participants with anorexia, over half switched between the restricting and binge-eating/purging, and one-third developed bulimia. But interestingly, people initially diagnosed with bulimia nervosa rarely developed anorexia. So while diagnostic crossover is common in eating disorders, it tends to follow specific patterns.
Both of these sets of behaviors serve as strategies for coping with difficult emotions and life stress. Behaviors like restricting food or binge-purge cycles temporarily relieve anxiety, distress, or emptiness. That emotional relief and sense of control11 make both conditions very hard to overcome without addressing the underlying psychological needs they’re meeting.
Impacts on People’s Lives
Finally, both of these common eating disorders seriously impact people’s quality of life, causing distress and making it hard to function at work or in social settings. They isolate people from their support networks at a time when they need connection the most.
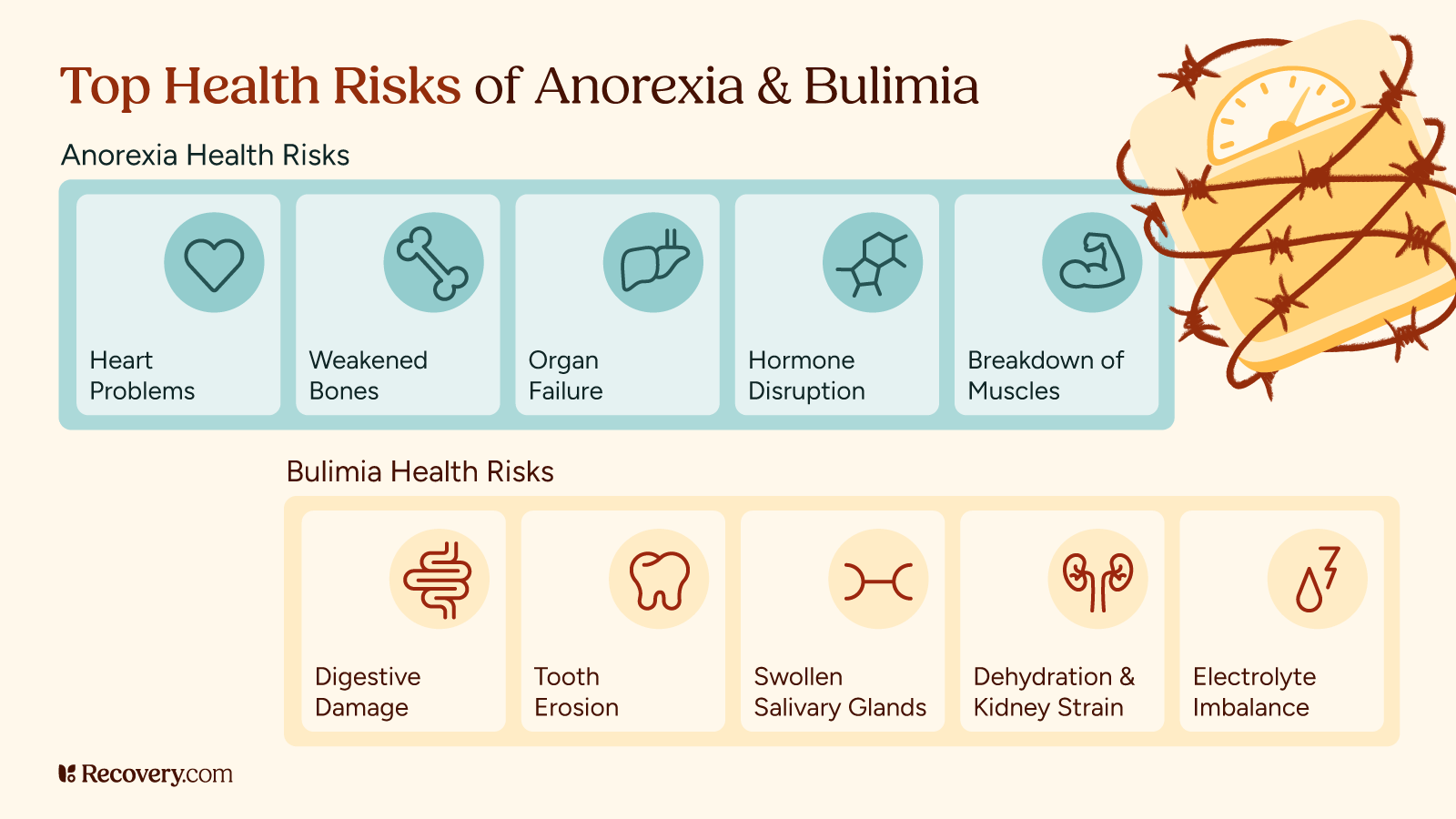
Health Risks and Complications
Anorexia and bulimia both cause serious health problems, but in different ways.
Health Risks of Anorexia
Anorexia has the highest death rate12 of any mental illness, with risks coming mainly from malnutrition that affects every system in the body. Severe malnutrition can cause:
- Heart problems
- Bone loss
- Muscle wasting
- Hormone imbalances
- In the worst cases, organ failure
Health Risks of Bulimia
Bulimia’s health risks13 come mainly from purging behaviors. Frequent vomiting can cause:
- Irregular heartbeat from electrolyte imbalance
- Cardiac arrest in severe cases
- Damage to the digestive system
- Tooth erosion
- Swollen salivary glands
Overusing laxatives or diet pills can lead to:
- Laxative dependence
- Chronic digestive problems
Hormonal Imbalance
Both disorders can affect fertility and hormones. In anorexia, periods often stop14 due to low body weight and fat percentage. While people with bulimia may continue having periods, hormone disruptions can still happen, which can affect their fertility and bone health.
Long-Term Problems
Long-term problems differ somewhat between these 2 conditions. With anorexia, long-term malnutrition15 can lead to:
- Permanent bone density loss and an increased risk of fractures
- Heart complications (bradycardia, arrhythmias, hypotension)
- Brain changes and cognitive impairment
- Reproductive issues
- Pregnancy complications
- Gastrointestinal problems
- Weakened immune function
- Electrolyte imbalances that affect multiple organ systems
- Increased overall mortality risk if left untreated
Bulimia’s long-term effects16 include:
- Chronic digestive problems
- Dental complications (tooth decay, gum disease)
- Higher risk of esophageal cancer from repeated exposure to stomach acid
- Osteoporosis due to nutritional deficiencies
- Menstrual irregularities and reproductive problems
- High cholesterol
- Increased risk of diabetes
- Heart irregularities and arrhythmias
- Severe dehydration and electrolyte imbalances
- Anemia
While some health issues like amenorrhea, acute dehydration, and certain heart problems may go away after recovery, others like osteoporosis, reproductive issues, diabetes risk, and cholesterol problems may need ongoing medical monitoring.
Medical Emergencies
If you experience fainting, chest pain, difficulty breathing, seizures, or blood in vomit, please seek emergency medical care immediately—these are not symptoms to ignore or push through. These signs indicate your body is in serious distress and requires urgent professional attention. We know reaching out to someone about an eating disorder can feel overwhelming, but regular medical supervision is absolutely essential to monitor and address these potentially life-threatening complications.
What approaches are most effective for families supporting a loved one in the early stages of eating disorder recovery?
It is important for families of loved ones in eating disorder recovery to be gentle and firm simultaneously. Be gentle in a way that validates one’s feelings, but be firm in not accommodating anxiety around eating. What would that look like? One may say to their loved one, ‘I can understand how you feel, and it is important to follow your therapist’s recommendations and eat to nourish your body.’ Using the word ‘and’ instead of ‘but’ validates both aspects of one’s experience and their long-term goal.
Jennifer Chicoine, MA, LCPC, CCTP | Peaceful Healing Counseling Services
Treatment Approaches
There’s real hope for recovery from eating disorders—both anorexia and bulimia respond well to proper treatment,17 and many people go on to live healthy, fulfilling lives free from these struggles. While the journey has its challenges, effective treatments exist and are continually improving.
Treatment approaches for anorexia and bulimia share some similarities, but also have important differences tailored to each condition. For someone with anorexia, especially when their weight has become dangerously low, the first priority is ensuring medical stability and safety. This compassionate healthcare might include time in a hospital or inpatient treatment center where a team of medical professionals can help restore weight in a gentle, supportive way.
With bulimia, treatment typically focuses on breaking the cycles of binging and purging and rebuilding a healthier relationship with food. Outpatient therapy is often the starting point, but some people might need additional medical support to address health complications.
People can and do recover, and build lifelong healthy relationships with food.6 As Aas says,
You deserve to eat, you deserve to recover from an eating disorder, you are worthy of love, you are worthy of acceptance—mainly from yourself.
Learn more about evidence-based approaches that can transform your journey to recovery in our guide to finding treatment for eating disorders.
Therapy
Both conditions benefit from psychotherapy, but the approaches might differ. For people with anorexia, family-based treatment (FBT)18 shows strong results, especially for adolescents. This approach empowers their family members to take an active role in their recovery.
For bulimia, cognitive behavioral therapy (CBT) is often the go-to treatment. It helps people identify unhelpful thought patterns, develop regular eating habits, and learn healthier ways to cope with their feelings.
Both conditions can also benefit from dialectical behavior therapy (DBT),19 which teaches skills for managing emotions and relationships.
Nutritional Counseling
Nutritional counseling plays a major role in treating both disorders, though the goals differ. For anorexia, the focus is on gradually increasing food intake and expanding variety. For bulimia, establishing regular eating patterns and challenging food rules is key to breaking the binge-purge cycle.
Medication
Medication has a more established role in bulimia treatment, with certain antidepressants showing effectiveness in reducing binge-purge behaviors.20 For anorexia, medication is less commonly the primary treatment but may help with co-occurring conditions like anxiety or depression.
Compassionate, Comprehensive Recovery and Support for Eating Disorders
Healing from an eating disorder takes both professional guidance and loving support. The journey looks different for everyone—people with anorexia may start with rebuilding their physical health, while people with bulimia may focus on establishing gentle routines.
When friends and family create spaces free of food judgment, recovery flourishes. And with compassionate professionals by your side, even setbacks become stepping stones.
Many people with these conditions find their way to complete recovery. Your struggle isn’t a personal failure—it’s a health condition that responds to care. If you’re suffering, find an eating disorder treatment program that meets your needs and reach out to a specialist today.
You deserve support, and healing is within reach.
FAQs
Q: What causes anorexia and bulimia?
A: These eating disorders develop from a mix of genetics, personality traits, family dynamics, and social pressures. Things like perfectionism, stress, and cultural beauty standards also play a huge role. They’re not choices or personality flaws—they’re serious health conditions that need supportive care.
Q: How do you know if someone has bulimia?
A: Signs of bulimia include sneaking off to the bathroom after meals, swollen cheeks, calluses on knuckles, excessive exercise, dental issues, and missing food. People with bulimia often succeed in keeping it hidden because their weight might not change much, but they struggle in secret.
Q: Will I ever accept being at a normal body mass index (BMI)?
A: Healing takes time, but yes, many people learn to feel comfortable in their bodies with the right support. Therapy helps challenge negative thoughts, and focusing on what your body can do instead of just how it looks can make a big difference.
Q: What are the first steps in getting help?
A: Start by talking to your therapist, doctor, or someone you trust. You can also use an independent, non-biased treatment finder or call the National Eating Disorders Association helpline (1-800-931-2237). A specialist can help figure out the best plan for you.
Kratom Withdrawal: 8 Steps for Easing Symptoms and Promoting Healing
Kratom seems like a mild, harmless drug, but it affects the brain in similar ways to opioids, and withdrawals can be very uncomfortable. Many people feel sick or have intense cravings when they try to cut back or stop using kratom similar to symptoms of opioid use disorder.
Everyone’s experience with kratom withdrawal is different. Some people have mild symptoms while others struggle more. Here’s what to expect to help you mentally prepare, make the process easier, and set yourself up for success.
We’ll take a deeper look at what kratom withdrawal feels like, how long it lasts, and what you can do to help yourself feel better and improve your chances of staying sober. We’ll also talk about when it might be time to get professional support.
What Is Kratom?
Kratom (Mitragyna speciosa) is a tropical tree1 related to coffee that grows naturally in Thailand, Malaysia, Indonesia, and other parts of Southeast Asia. For centuries, local workers chewed the leaves or brewed them into tea to fight fatigue and increase productivity during long workdays. It’s gained popularity in recent years as a recreational drug.
Today, people use Kratom for pain relief or to help with opioid withdrawal. While it might seem helpful at first, regular use can cause you to become physically dependent, making it hard to stop.
How Kratom Works in Your Body
When you take kratom, chemicals in the plant called alkaloids2 (mainly mitragynine and 7-hydroxymitragynine) interact with receptors in your brain. At low doses, these chemicals create mild stimulant effects, making you feel more energetic. At higher doses, the create opioid-like effects,3 producing pain relief and feelings of pleasure or relaxation.
Kratom use is complex because it affects multiple brain systems at once. It activates opioid receptors (like morphine or oxycodone would), but also impacts other systems that regulate your energy and mood. This complex pharmacology explains why kratom can be both stimulating and sedating.
Kratom is not as high-risk as some other substances, but it can have serious side effects that should be taken seriously. Per the National Institute on Drug Abuse (NIDA).
Rare but serious effects have been reported in people who use kratom,4 including psychiatric, cardiovascular, gastrointestinal and respiratory problems.
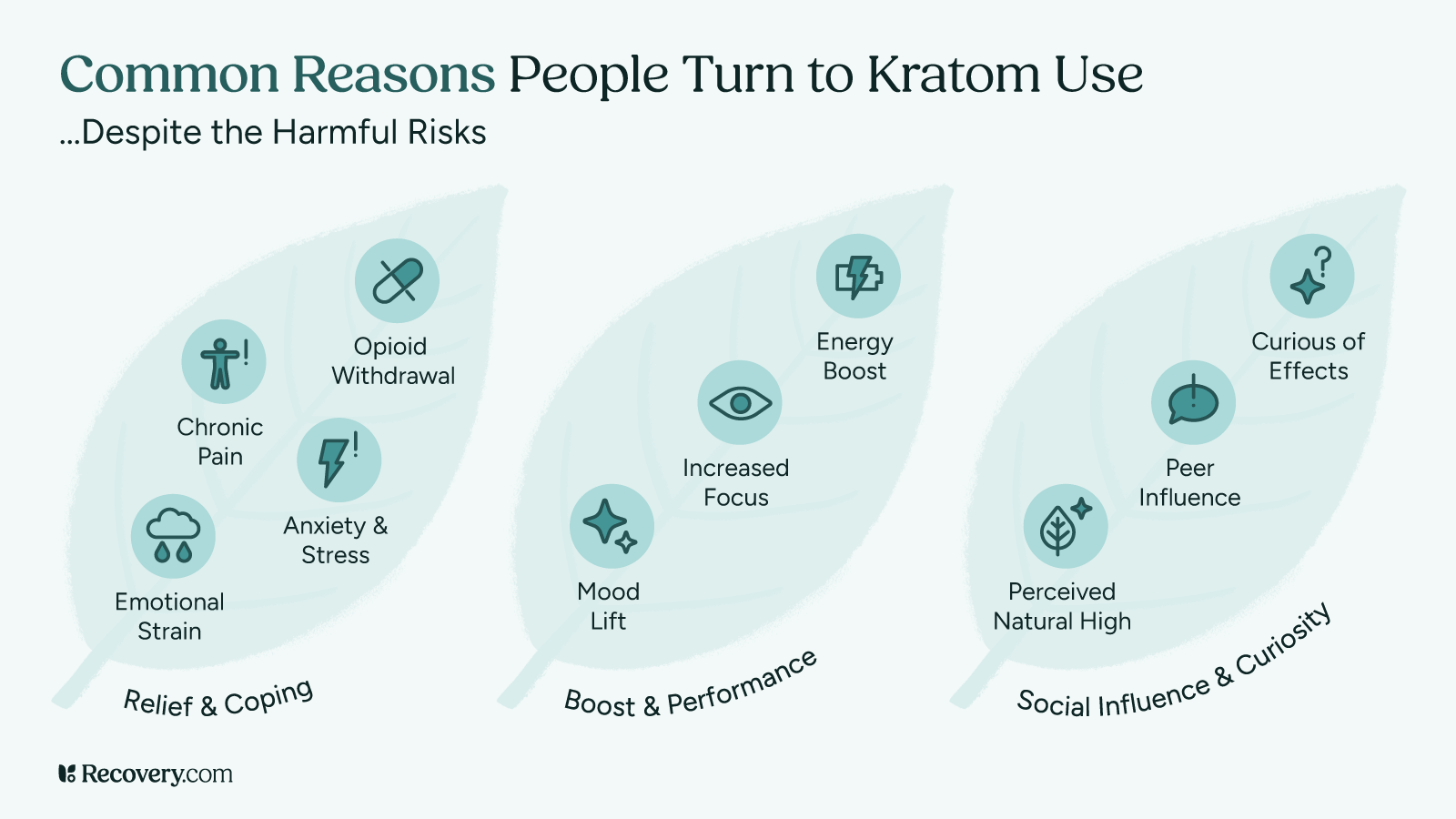
How People Use Kratom
In the U.S. and other Western countries, people use kratom for various reasons:5
- Managing chronic pain
- Easing opioid withdrawal symptoms
- Self-medicating anxiety or depression
- Boosting energy or focus
- Recreational purposes
Kratom comes in different forms: Powder, capsules, extracts, and teas. Some people chew the leaves directly, while others mix the powder into drinks or food.
See our article on self-medicating with substances to understand if you might be using kratom to cope with underlying issues.
Kratom’s Legal Status
Kratom’s legal status is unclear in many places. The U.S. Food and Drug Administration (FDA) has issued warnings about the safety of kratom6 and has not approved it for any medical use. While kratom remains legal federally in the U.S., several states and cities have banned it.
The Drug Enforcement Administration (DEA) classifies kratom as a “Drug and Chemical of Concern.” Internationally, some countries where kratom grows naturally have made it illegal, and regulations vary widely elsewhere.
This uncertain legal status makes it hard for manufacturers to ensure kratom’s purity and safety7 for those who use it.
Kratom Dependency and Addiction
Like many substances that affect your brain, regular kratom use can cause you to become physically dependent.8 This means your body adapts to having kratom in your system and starts relying on it to function normally.
How Dependency Develops
When you use kratom regularly, your brain adjusts to the chemicals it provides. Over time, your brain may produce fewer of its own, natural feel-good chemicals because it’s getting them from kratom instead. When this happens, you might need higher doses to feel the same effects of kratom (tolerance), and your body might react negatively when you don’t have it (withdrawal).
Kratom dependency9 can ramp up in as little as a few weeks of daily use, though it varies from person to person. How quickly you become physically reliant on kratom depends on:
- How often you use kratom
- How much you take each time
- Your personal body chemistry
- Whether you use other substances at the same time
Dependency vs. Addiction
While dependency is mainly about your body’s physical reliance on kratom,10 addiction involves both physical dependency and behavioral changes. If you find yourself doing any of the following, it could be a sign that you’re developing a kratom addiction:
- Continuing to use kratom despite its negative effects on your life
- Spending a lot of time getting, taking, or recovering from kratom
- Neglecting responsibilities or missing out on important activities because of your kratom use
- Being unable to reduce or control your use of kratom
- Having strong cravings for kratom
Risk Factors for Kratom Dependency
Some factors that might make you more likely to develop dependency include:
- A history of substance abuse problems
- Using kratom to self-medicate mental health issues
- Starting to take larger doses of kratom or graduating to more highly concentrated extracts
- Taking kratom daily or throughout the day
- Using it for extended periods
- Combining it with other substances
Understanding the difference between casual use, dependency, and addiction helps you identify where you might be on this spectrum. If you notice signs of dependency or addiction, it may be time to reevaluate your relationship with kratom and start making some changes.
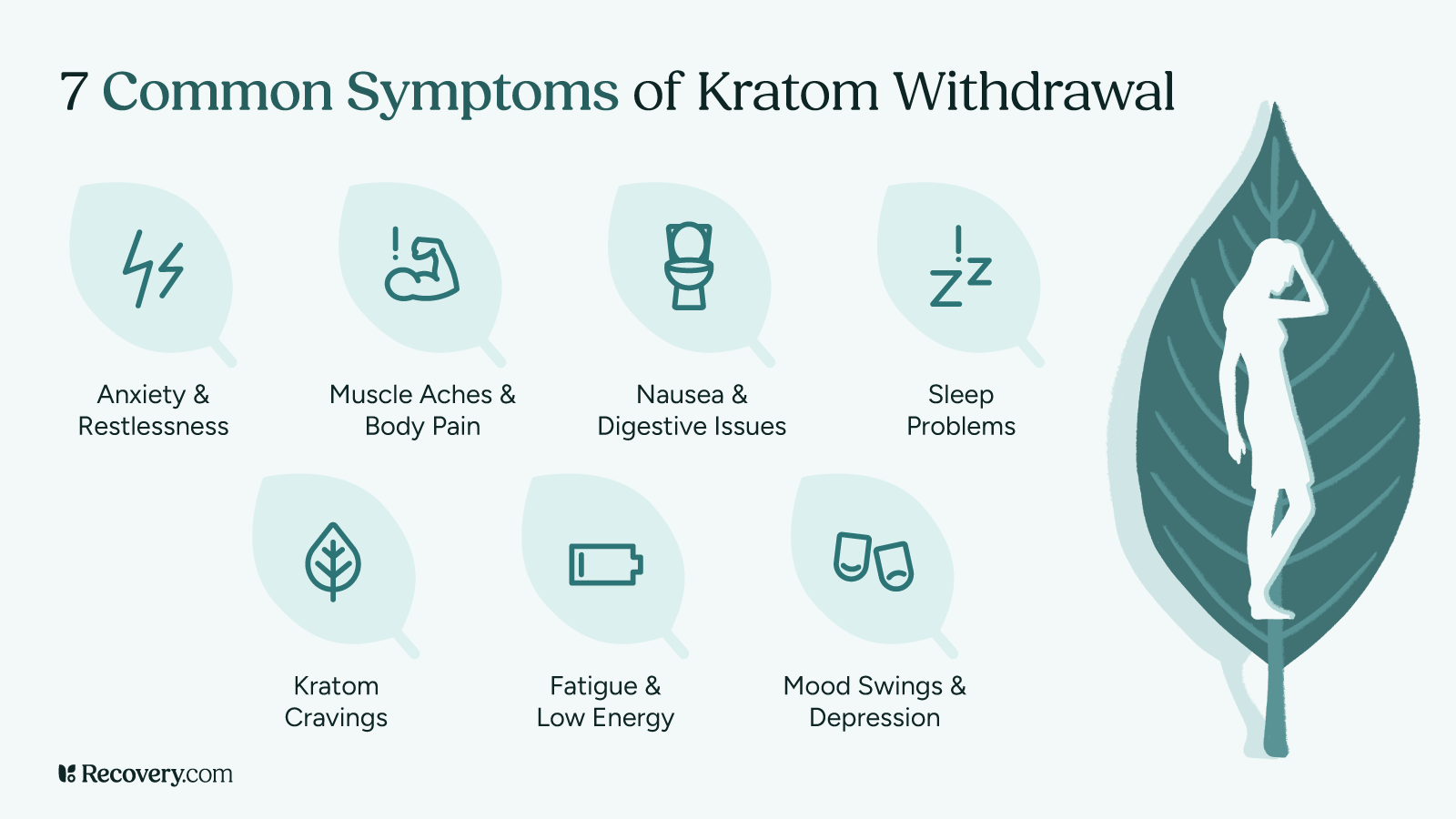
Kratom Withdrawal Symptoms
When you stop taking kratom after regular use, your body needs time to adjust to functioning without it. This adjustment period can bring on a range of uncomfortable symptoms that affect both your body and mind.
Physical Symptoms You Might Experience
Your body can react in several ways when you stop taking kratom:11
- Muscle aches and pains: Many people say they feel like they have the flu, with sore, achy muscles and joints. Moving around feels harder than usual.
- Nausea and stomach problems: Your digestive system often reacts strongly during withdrawal. You might feel queasy or sick to your stomach. Some people have vomiting, diarrhea, or loss of appetite.
- Sweating and chills: Your body’s temperature regulation can go a bit haywire. You might find yourself sweating heavily one moment and feeling cold the next. Night sweats are especially common.
- Runny nose and watery eyes: Just like with a cold, you might have a runny nose and eyes that tear up for no reason.
- Tremors or shaking: Some people notice their hands trembling or have full-body shakes during withdrawal.
- Headaches: These can be accompanied by sensitivity to light or sound.
- Fatigue and weakness: You might feel completely drained of energy, making even simple tasks feel exhausting.
Psychological Symptoms
There are also mental symptoms of kratom withdrawal:12
- Anxiety and restlessness: You may feel on edge, unable to relax, have racing thoughts, or feel a sense of worry that’s hard to shake.
- Mood swings: You might be on an emotional roller coaster, feeling irritable, angry, or sad for no clear reason.
- Depression: Some people have a persistent low mood, lack of motivation, or feelings of hopelessness during withdrawal.
- Cravings: You might find yourself thinking about kratom often and having strong urges to take it again.
- Brain fog: Many people report having difficulty focusing or thinking clearly during withdrawal.
A Closer Look at Kratom Withdrawal Insomnia
Sleep problems deserve special attention because they can make everything else feel worse. During kratom withdrawal, you might:
- Have trouble falling asleep, even though you’re exhausted
- Wake up throughout the night
- Have vivid, disturbing dreams
- Feel like you haven’t truly rested even after sleeping
Kratom withdrawal insomnia generally peaks during the first week but can linger for several weeks. Getting even small amounts of quality sleep can make a big difference in how you feel.
Sleep struggles during withdrawal? Learn more about managing withdrawal insomnia and get tips for better rest during recovery.
What Makes Withdrawal Better or Worse?
Several factors affect how intense your withdrawal symptoms will be:
- How much kratom you used: Generally, higher doses lead to more intense withdrawal.
- How long you’ve been using it: Longer-term use typically means more pronounced withdrawal.
- Your overall well-being: Being in good health otherwise can make withdrawal more manageable.
- Support system: Having people who understand what you’re going through can make a huge difference.
- Previous withdrawal experiences: If you’ve gone through withdrawal before, your body might react more strongly the next time (this is called the kindling effect).13
As you go through this process, it’s good to keep in mind that withdrawal symptoms are temporary. They’re your body’s way of healing and finding a new balance without kratom. While they are uncomfortable, they’re not dangerous for most people and will improve with time.
Kratom Withdrawal Timeline
If you’re planning to stop using kratom, having a roadmap of what to expect can help you prepare mentally. While everyone’s experience differs, most kratom users follow a somewhat predictable timeline of symptoms.
When Do Withdrawal Symptoms Start?
For most people, kratom withdrawal begins within 12-24 hours14 after your last dose. If you’ve been using very high doses or potent extracts, you might notice symptoms starting even sooner—sometimes within just 6 to 12 hours.
The onset often feels like a growing sense of discomfort, restlessness, or anxiety. You might notice minor physical symptoms like yawning, watery eyes, or a runny nose before more intense symptoms kick in.
Early Acute Phase (Days 1-3)
The first few days are typically the most challenging:
- Day 1: You’ll have anxiety, restlessness, and physical discomfort. Sleep might be difficult, and you may have strong cravings for kratom.
- Days 2-3: Physical symptoms usually intensify during this period. Muscle aches, sweating, nausea, and digestive issues peak. A lot of people describe this stage as feeling like a bad flu.
During this phase, remind yourself that what you’re experiencing is normal and temporary. The discomfort means your body is beginning to adjust to functioning without kratom.
Peak Symptoms (Days 2-5)
For most people, withdrawal symptoms reach their worst point somewhere between days 2 and 5. This is when the combination of physical discomfort and psychological symptoms can feel overwhelming.
The good news is that once you get through this peak period, your body starts to heal, and symptoms gradually become less intense. Many people find that reaching this turning point gives them the motivation to continue.
Subacute Phase (Days 6-14)
After the peak, you’ll enter the subacute phase:
- Most severe physical symptoms (like nausea, vomiting, and body aches) start to fade
- Sleep gradually improves, though it may still be disrupted
- Mood symptoms like anxiety and depression may linger
- Energy levels slowly begin to return
By the end of the second week, most people find that they’re functioning reasonably well, though not entirely back to normal.
Post-Acute Withdrawal Syndrome (PAWS)
Some people have lingering symptoms for weeks or even months after quitting substances. This is known as post-acute withdrawal syndrome,15 or PAWS. These symptoms are usually milder than acute withdrawal but can still affect your quality of life:
- Periodic mood swings
- Anxiety or depression that comes and goes
- Trouble with motivation or concentration
- Sleep disturbances
- Occasional cravings for kratom
PAWS symptoms typically come in waves: You might feel fine for several days, then have a few hard days before improving again. Each wave tends to be less intense than the one before.
Remember that healing isn’t a linear process. Having good and bad days during recovery is completely normal. With time, these waves become less frequent and less intense as your brain chemistry rebalances.
Are you having lingering symptoms after the initial withdrawal phase? Learn about post-acute withdrawal syndrome (PAWS) and how to manage these longer-term recovery challenges.
Managing Kratom Withdrawal at Home
Many people successfully navigate kratom withdrawal from the comfort of their own homes. With the right approach and preparation, you can make this challenging process more manageable.
1. Is Home Detox Right for You?
Home detox might be appropriate if:
- You’ve been using moderate amounts of kratom
- You don’t have other serious health conditions
- You have a support person who can check on you
- You don’t have a history of severe withdrawal
- You’re not using other substances like alcohol or opiates
However, home detox isn’t right for everyone. Your safety comes first. Here’s how to know when it’s time to seek professional help:
2. When to Seek Professional Help
Watch for these warning signs that indicate you may need medical support:
- Severe depression or thoughts of harming yourself
- Extreme dehydration from vomiting or diarrhea
- Racing heartbeat, chest pain, or difficulty breathing
- Seizures or hallucinations
- Inability to keep any food or water down for more than 24 hours
- Withdrawing from multiple substances at once
If you experience any of these, do not hesitate to reach out to a healthcare provider.
3. Tapering: A Gentler Approach
Instead of stopping kratom cold turkey, some people find that gradually reducing their dose helps minimize withdrawal symptoms. Here’s a simple tapering approach:
- Start by measuring your current daily amount accurately
- Reduce your total daily amount by about 10-15% every 2-3 days
- Space out your doses evenly throughout the day
- Go slower with reductions if withdrawal symptoms become too uncomfortable
- Keep a log to track your progress
Tapering off of kratom takes longer than quitting cold turkey, but it’s often much more comfortable. Be patient with yourself—a gradual taper over several weeks is typically easier on your body than a rapid one.
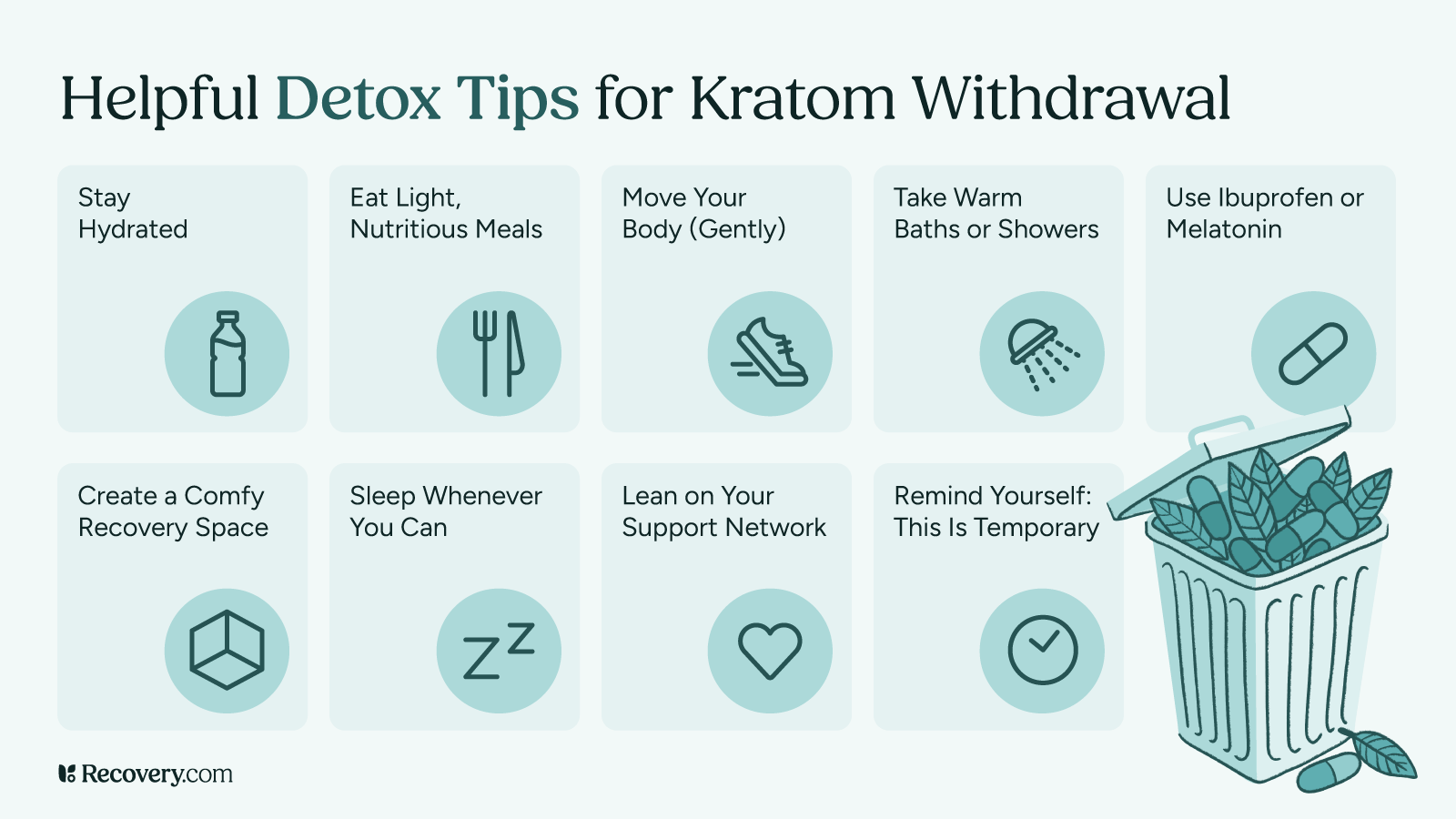
4. Self-Care Strategies That Help
These simple kratom withdrawal remedies16 can make a big difference in how you feel:
- Stay hydrated: Drink plenty of water and fluids to replace hydration lost through sweating or digestive issues.
- Nourish your body: Even if you don’t feel hungry, try to eat small, nutritious meals. Foods rich in magnesium (like nuts) and potassium (like bananas) may help with muscle cramps.
- Move your body (gently): Light exercise like walking or stretching can release natural endorphins that improve your mood and help with sleep.
- Warm showers or baths: The warmth can temporarily relieve muscle aches and help you relax.
- Create a comfortable recovery space: Clean sheets, comfortable clothes, and a quiet environment can help ease your mind.
5. Helpful Over-the-Counter Options
While these aren’t cures for withdrawal, they may help manage specific symptoms:
- For aches and pains: Non-prescription pain relievers like acetaminophen or ibuprofen (always follow package directions)
- For diarrhea: Over-the-counter anti-diarrheal products
- For nausea: Ginger tea, ginger candies, or motion sickness remedies
- For sleep: Melatonin, valerian root tea, or magnesium supplements before bedtime
*Note that these are general suggestions, not medical advice. Check with your doctor first if you’re unsure about taking any medication or supplement, especially if you have other health conditions or take prescription medications.
Professional Treatment Options
Sometimes, getting expert help makes the difference between struggling through withdrawal and finding a smoother path to recovery. Professional drug addiction treatment provides structure, medical supervision, and tools to address not just your kratom use, but also what led you to addiction in the first place.
6. Medical Detox Programs
Medical detox programs are safe settings where healthcare professionals monitor your withdrawal symptoms and provide relief. These programs typically last 3-7 days and focus on helping you get through the acute withdrawal phase comfortably. Because the discomfort of withdrawal causes many people to start using again, supervised detoxification can improve your chances of recovery success.
Other benefits of professional kratom detox include:
- 24/7 medical supervision
- Medications to ease specific symptoms
- Prevention of complications
- Emotional support during a challenging time
Many insurance plans cover detox services, especially if your provider determines it’s medically necessary.
7. Helpful Approaches in Treatment
Effective treatment programs typically include:
Medications: While there’s no FDA-approved medication specifically for kratom withdrawal, providers may prescribe medications to target specific symptoms, like clonidine for anxiety or trazodone for sleep problems.
Talk therapy: Interventions like cognitive behavioral therapy (CBT) help you identify and change patterns that led to kratom use, plus develop healthier coping skills.
Group support: Connecting with others who understand what you’re going through can be incredibly healing. Many programs include group therapy or facilitate attendance at support groups.
Addressing co-occurring issues: If you’ve been using kratom to self-medicate anxiety, depression, pain, or trauma, treatment will include addressing these underlying concerns.
Discover effective ways to reclaim your life from pain through specialized rehab programs in our article on managing chronic pain.
Choosing Between Inpatient and Outpatient Care
After detox (or sometimes instead of it), you might consider:
Inpatient or residential rehab: You live at the facility for a set period, usually 28-90 days. This option provides the most structure and removes you from environments that might trigger kratom use.
Intensive outpatient programs (IOPs): You attend treatment several days a week for a few hours each day while living at home. This allows you to maintain work or family responsibilities while getting substantial support.
The right level of care depends on your specific situation, including the severity of your kratom use, your support system at home, and any other challenges you’re facing.
8. Building Long-Term Recovery Support
Recovery continues long after formal treatment ends. Many programs help you develop a continuing care plan that might include:
- Ongoing therapy sessions
- Support group meetings
- Wellness practices like meditation or exercise
- Regular check-ins with a recovery coach
- Medication management if needed
Remember that seeking professional help isn’t a sign of weakness—it’s a proactive commitment to your health. Many people who go through formal treatment of some kind find that the structure and support give them a helpful foundation to create lasting change.
Preventing Relapse
After you’ve gone through the challenge of kratom withdrawal, the next order of business is to stay kratom-free. Relapse prevention isn’t just about willpower —it’s about understanding your triggers and building healthy strategies to navigate life’s ups and downs.
Recognizing Your Personal Triggers
Most people have specific situations, feelings, or environments that make them want to use kratom again. Common triggers include:
- Stress and difficult emotions: Feeling overwhelmed, anxious, angry, or sad
- Physical discomfort or pain, especially if you used kratom for pain management
- Social situations: Being around others who use kratom or in places where you used it
- Boredom or lack of structure: Having too much unoccupied time
- Celebrating or rewarding yourself: Thinking “just this once” won’t hurt
Learning to identify your personal triggers is the first step in reducing your risk of relapse. When you notice a trigger, pause and remind yourself that the urge to use will pass, even if it feels intense in the moment.
Building Your Support Network
Recovery thrives in connection. Consider building support through these avenues:
- Friends and family: Let trusted loved ones know what you’re going through and how they can help
- Support groups: Consider SMART Recovery, Narcotics Anonymous (NA), or online forums focused on kratom recovery
- Behavioral health professionals: A therapist or counselor who understands substance use disorders
- Recovery apps: Many free apps offer tools for tracking your progress and connecting with others
Having people you can reach out to when cravings hit can make all the difference in preventing a momentary urge from becoming a relapse.
Practicing Healthy Coping Strategies
Life is hard at times and we need healthy ways of managing it! A large part of recovery is learning and practicing more helpful ways of dealing with challenges:
- Physical activity: Exercise naturally boosts your mood and energy levels
- Mindfulness practices: Meditation, deep breathing, or yoga can help manage stress
- Creative outlets: Music, art, writing, or other creative pursuits
- New hobbies: Activities that engage your mind and bring satisfaction
- Helping others: Volunteering or supporting someone else’s recovery
The more tools you have in your toolkit, the better equipped you’ll be to handle difficult times. The key is to get those resources in place before those moments arrive.
Building a Recovery-Friendly Lifestyle
Small daily habits can strengthen your recovery:
- Regular sleep schedule: Aim for 7-9 hours of quality sleep each night.
- Balanced nutrition: Eat regular meals that support brain and body health.
- Limit caffeine and sugar: These can mimic anxiety symptoms and trigger cravings.
- Practice self-compassion: Recovery isn’t perfect—learn from setbacks rather than beating yourself up.
- Celebrate milestones: Acknowledge your progress, whether it’s days, weeks, or months kratom-free.
Recovery is a process, not an event. Each day you make choices that support your health is a success, and even if you experience a setback, you haven’t lost the progress you’ve made.
Learn how proper nutrition can fuel your recovery journey in our article on nutrition for addiction and mental health healing.
Moving on From Kratom
Recovery from kratom dependency is a journey that takes time, patience, and sometimes a helping hand. While the withdrawal process has its challenges, remember that thousands of people have successfully navigated this path before you!
If you’re struggling with kratom addiction or withdrawal, you don’t have to go through it alone. Professional care can mean the difference between a difficult, uncertain recovery and one with proper guidance and support.
Treatment specialists understand what you’re going through and can help you with tools, medication, and strategies that significantly improve your chances of success.
Ready to take the next step? Search for a treatment provider today. Many treatment centers offer free, confidential assessments to help determine what level of care might be right for you. You’ll thank yourself for having the courage to ask for help when you needed it.
FAQs
Q: What is kratom addiction?
A: Kratom addiction occurs when regular use leads to dependence, causing physical or psychological cravings and withdrawal symptoms when not taken.
Q: How long do kratom withdrawals last?
A: Withdrawal symptoms typically begin within 6–12 hours after the last dose and can last from 3 to 10 days, depending on frequency and amount used.
Q: How long does kratom withdrawal insomnia last?
A: Insomnia during kratom withdrawal can last from a few days up to a week. Sleep patterns may gradually improve as the body adjusts.
Q: What are the withdrawal symptoms of Ketum?
A: Ketum (another name for kratom) withdrawal symptoms may include anxiety, irritability, muscle aches, insomnia, sweating, nausea, and cravings.
Q: What drug has the worst withdrawal symptoms?
A: Opioids, alcohol, and benzodiazepines are often considered to have the most severe withdrawal symptoms, sometimes requiring medical detox. Kratom withdrawal is usually milder but still uncomfortable.
Q: What are kratom withdrawal symptoms?
A: Common symptoms include anxiety, restlessness, muscle aches, insomnia, nausea, diarrhea, and emotional distress.
Q: Should I detox from kratom at home?
A: Detoxing at home may be possible for mild cases, but medical supervision is recommended if symptoms are severe or if there are co-occurring mental health conditions.
Q: Does kratom affect blood pressure?
A: Yes, kratom can affect blood pressure. It may cause either elevated or lowered blood pressure depending on dosage and individual response.
Q: What is kratom used for?
A: Kratom is often used for pain relief, mood enhancement, increased energy, and in some cases, self-management of opioid withdrawal—though it is not FDA-approved for medical use.
Q: Are you covered for addiction treatment?
A: Coverage depends on your health insurance provider and plan. Many policies include behavioral health services. Contact your insurer to confirm benefits for substance use treatment.
Q: How is kratom addiction treated?
A: Treatment may involve tapering off use, behavioral therapy, support groups, and in some cases, medications to manage symptoms or co-occurring conditions.
Q: What are effective ways to manage kratom withdrawal symptoms?
A: Staying hydrated, using over-the-counter medications for symptom relief, maintaining a sleep routine, and seeking counseling or medical support can help manage withdrawal.
Q: How can I manage kratom withdrawal symptoms effectively?
A: Similar to above—gradual tapering, professional support, proper nutrition, and self-care strategies can reduce discomfort during withdrawal.
Q: What are the stages of kratom withdrawal?
A: Withdrawal typically progresses through early symptoms (6–12 hours), peak discomfort (2–4 days), and gradual resolution (5–10 days), though timelines vary by individual.
Chelsea Ocean on Losing a Loved One to Alcohol Addiction and Navigating Grief
“I used to call him Jekyll and Hyde because he was a perfect man when he was sober. Handsome and perfect and sweet and kind and loving and hardworking… And then when he was drunk, he was the worst human being on the planet, the most manipulative, conniving, careless…” These powerful words from Chelsea Ocean on Recoverycast paint a stark picture of the duality that often characterizes life with someone struggling with alcoholism. Her raw and honest account of loving and ultimately losing her partner, Dan, to this insidious disease offers invaluable insights for anyone navigating the turbulent waters of addiction in their relationships.
Chelsea’s story is a testament to love, resilience, and the heartbreaking realities of alcoholism. Through her journey, we can glean crucial lessons about recognizing the signs, understanding the progression, and coping with the profound impact of addiction on individuals and their loved ones.
The Illusion of Perfection and the Mask of Addiction
Chelsea recounts the early days of her marriage with Dan as “literally perfect.” This highlights a common phenomenon where individuals struggling with early-stage alcoholism can maintain a seemingly normal and even exceptional facade. As Chelsea notes, “people used to come over and be like, how do you guys have such a perfect marriage? Tell us.” This can make it incredibly difficult to recognize the subtle beginnings of a problem.
However, beneath this veneer of perfection, the insidious nature of addiction can take root. As Chelsea later realized, looking back with knowledge about alcoholism’s progression, they were already in the later stages of addiction by the time she recognized a significant issue. This underscores the importance of understanding the stages of alcoholism to identify potential problems early on.
The Gradual Progression and Missed Warning Signs
Chelsea’s initial unawareness of Dan’s increasing tolerance exemplifies how easily the early stages of alcoholism can be missed, especially by those unfamiliar with heavy drinking. “Before he left, we were in stage two, I would say, where he was building a tolerance. But to me who had not been around alcohol… I never noticed anything. He was fine. He never got drunk.” In a culture where social drinking is prevalent, and a high tolerance can even be seen as somewhat impressive, these early signs can be easily dismissed.
It’s crucial to remember that building a tolerance is a physiological adaptation to regular alcohol consumption and a key indicator of developing dependence. What might seem like simply holding one’s liquor well can be a sign of the body adjusting to increasing amounts of alcohol.
The Impact of Environment and Culture
Chelsea poignantly describes the drinking culture within the military and how it may have contributed to Dan’s early drinking habits. “Dan was that kid where he was drinking very young… he was in the military and they all drink in the military.” The high-stress environment, coupled with a bonding culture centered around alcohol, can create a breeding ground for problematic drinking.
The military has acknowledged the challenges of alcohol misuse within its ranks and has implemented programs aimed at shifting the culture and providing support. However, Chelsea’s experience highlights the potential disconnect between stated policies and the lived realities of service members.
The Isolation and Fear of Seeking Help
Chelsea’s account of the military’s unsupportive stance towards active-duty personnel struggling with addiction is deeply concerning. “If you’re active duty and you are an alcoholic or you’re struggling with some sort of addiction or mental health issue, you are afraid to tell anyone because you will lose your job.” This fear of repercussions can create a significant barrier to seeking help, trapping individuals in a cycle of secrecy and isolation.
This situation underscores the critical need for destigmatizing addiction and mental health issues within high-stakes professions and ensuring accessible and confidential support systems.
Recovery.com offers resources for finding support and treatment options.
The Strain on Relationships and the Burden on Loved Ones
Chelsea vividly portrays the emotional turmoil and practical challenges of living with someone whose personality drastically changes under the influence of alcohol. The “Jekyll and Hyde” analogy perfectly encapsulates this jarring contrast. The unpredictability, disappearances, and the constant state of worry take a significant toll on the mental and emotional well-being of the partner and family.
“And I’m home with a newborn baby without another vehicle and just kind of like, okay, well, if he dies, no one’s going to know because I have no clue where he is.” This desperate situation highlights the profound sense of helplessness and fear experienced by loved ones.
The Futility of Control and the Need for Boundaries
Chelsea’s early attempts to control Dan’s drinking – yelling, fighting, hiding credit cards – are common reactions from loved ones desperately seeking to stop the destructive behavior. However, as she learned, “none of that works. All it does is drive you insane.” Addiction is a complex disease, and the individual struggling with it must ultimately choose recovery.
Establishing healthy boundaries becomes crucial for the well-being of the non-addicted partner. This might involve detaching emotionally from the addict’s behavior and focusing on one’s own self-care and safety.
Read how to set healthy boundaries in relationships affected by addiction.
The Rollercoaster of Hope and Disappointment
The cycle of Dan getting “better and then spiral and then get better and then spiral” is a heartbreakingly common experience for families dealing with addiction. These brief periods of sobriety can offer a glimmer of hope, leading loved ones to believe that change is possible. However, without sustained recovery efforts and addressing the underlying issues, relapse is a significant risk.
“Just enough for me to, like, hold on, like, just enough for me to have hope. Well, okay, he was sober for four weeks this time. So he can be sober.” This highlights the emotional manipulation inherent in the cycle of addiction, where intermittent sobriety can reinforce the partner’s hope and commitment.
The Physical Dependence and the Struggle to Stop
Chelsea’s description of Dan’s physical withdrawal symptoms illustrates the powerful grip of physical dependence in later stages of alcoholism. “He wants to be sober. He doesn’t want to drink, but he can’t, he can’t say no… he has tremors or he would get sweats or he would, you know, get anxiety attacks.” This highlights the medical necessity of proper detoxification and medical supervision for individuals with significant alcohol dependence.
The Erosion of Trust and the Impact of Dishonesty
The lack of “rigorous honesty” that often accompanies active addiction erodes the foundation of trust in a relationship. Even seemingly small lies about drinking habits chip away at intimacy and connection. “How many beers did you have?” becomes a loaded question, and the constant deception creates a climate of suspicion and distrust.
The Cycle of Guilt, Shame, and Relapse
Chelsea astutely points out the vicious cycle of guilt and shame that can perpetuate addiction. The negative behaviors and consequences of being drunk lead to feelings of remorse when sober. However, these feelings can be overwhelming and difficult to manage, often triggering a return to drinking as a way to numb the pain.
“When they get sober, what do they have, like you said, you have the guilt and the shame and you don’t want to feel those things, especially as an alcoholic. You can’t manage it… So what do you do? You drink again because you don’t [want to feel it].” Breaking this cycle requires addressing the underlying emotional and psychological issues that contribute to both the addiction and the inability to cope with sobriety.
The Misguided Attempts to “Fix” and the Powerlessness of Love
Chelsea’s heartbreaking account of trying everything to help Dan, including having another child, reveals the desperate measures loved ones often take in their attempts to “fix” the situation. “You think if I could just give them more good, if I could just put more good in their life, it’ll be enough… I can fix it. I can fix it. But you cannot.”
This realization is crucial. While love and support are essential, they cannot force someone into recovery. The individual with the addiction must ultimately make the choice to seek help and commit to the challenging journey of sobriety. Al-Anon is a support group for families and friends of alcoholics that emphasizes detaching with love and focusing on one’s own well-being.
The Breaking Point and the Need for Self-Preservation
The devastating incident following the birth and open-heart surgery of Chelsea’s second child served as a profound breaking point. Dan’s disappearance during this critical time underscored the severity of his addiction and the threat it posed to the well-being of their family.
“So that happened and after that, I was like, Oh, this is it, like, this is the end. I will raise two children by myself. We are done.” This moment of clarity highlights the critical need for self-preservation when living with active addiction. Setting firm boundaries and being prepared to prioritize one’s own safety and the safety of children is paramount.
Choosing Light and Living Fully
Chelsea’s journey, though marked by profound loss, has evolved into a testament to resilience and healing. Today, she lives a full and meaningful life, carrying Dan’s memory forward with love and honesty. She openly speaks about him with her children, ensuring his place in their family narrative while also imparting the crucial lessons learned from his struggles.
Importantly, Chelsea emphasizes that she carries no burden of blame for Dan’s passing, understanding that addiction is a formidable disease. Her focus now is on living her truth, advocating for awareness, and supporting others navigating similar paths, transforming her personal tragedy into a source of hope and empowerment.
Finding Strength in Vulnerability and Sharing Our Stories
Chelsea Ocean’s courageous sharing of her personal story on Recoverycast offers a beacon of hope and understanding for those touched by alcoholism. Her journey underscores the complexities of loving someone with addiction, the importance of recognizing the signs and stages, and the vital need for support and self-care.
Chelsea’s vulnerability is a powerful reminder that by sharing our experiences, we can break the stigma surrounding addiction, raise awareness, and ultimately help others navigate their own journeys toward healing and recovery. If you or someone you know is struggling with alcohol addiction, please know that help is available.
Recovery.com offers a comprehensive directory of treatment centers and resources.
Katlyn’s 9 Steps Towards Healing from Trauma, Abuse, and an Eating Disorder
In a deeply candid and moving conversation, Katlyn, a survivor in recovery from narcissistic abuse, Complex PTSD, and anorexia, shared invaluable insights into her journey. Her words offer a beacon of hope and practical guidance for anyone grappling with the aftermath of trauma and the challenging path of recovery.
Katlyn’s experience highlights the tumultuous nature of healing, emphasizing that it’s not a linear ascent but rather a complex dance of progress and setbacks. Yet, through vulnerability and the development of crucial coping mechanisms, a more grounded and present life is possible.
1. Recognizing the Need and Finding Inner Strength
Before recovery, Katlyn described emotional instability and chaos, feeling disconnected from the present. The turning point came when she recognized her strength in escaping a harmful situation. “Once I got myself out of that situation, it was a wake up call for me that I had the strength and resilience to remove myself from the situation to even identify the abuse as it is.” This acknowledgment of inner resilience is the crucial first step towards healing.
2. Seeking Support and Building a Foundation
A cornerstone of Katlyn’s recovery was actively seeking support from trusted individuals and professionals. “To help set myself on a path to recovery, I reached out for help, first of all, to people that I trusted with my vulnerable state. Um, I then got myself into some therapy specifically for what I am going through in recovering from.” Therapy, support groups, and even nutritional guidance create a vital network for navigating the complexities of trauma recovery.
Explore treatment options for trauma and eating disorders.
3. Establishing Structure and Self-Care Rituals
Creating daily routines provided Katlyn with stability and fostered self-care. “Just kind of establishing daily rituals for myself, kind of a container and structure for my day…made me feel healthy, clean, loved, and taken care of by myself.” Consistent rituals, even small ones, offer comfort and reinforce self-compassion.
4. Processing Emotions Through Expression
Katlyn found significant benefit in expressing her emotions, whether through journaling or talking. “I think journaling was something else that I started doing daily…my main advice would be to get it out, vomit out the emotion, however you need to do that.” Externalizing feelings prevents them from becoming internalized and allows for greater self-awareness and emotional regulation.
5. Rebuilding the Self with Compassion and Connection
Recovery involves redefining one’s relationship with oneself, moving away from being defined by trauma. “Seeing me for the first time with all of the things that I’ve experienced as a beautiful, strong person versus feeling like those things are me, are defining me.” Connecting with others who have similar experiences breaks isolation and reinforces that healing is possible. Group and family therapy can provide a safe place to foster meaningful connections. Cultivating self-compassion is also key.
6. Allowing Time and Embracing the Nonlinear Journey
Katlyn emphasized the importance of patience in the healing process. “That’s something else that I learned that helped me stay in recovery is that I need time. Time changes things. It gives us new perspectives.” Trauma processing is not linear; it involves ups and downs. Accepting this reality and allowing time for healing is crucial.
7. Cultivating Present Moment Awareness and Reclaiming Joy
Finding grounding in the present and rediscovering joy are vital aspects of recovery. “Having started my recovery journey, my life now is definitely a lot more present…my life is filled with…just a lot of good freaking food.” Engaging with the present and allowing oneself to experience pleasure, even in small ways, counteracts the negative impacts of trauma.
8. Setting Boundaries and Communicating Needs
Learning to identify fear, set boundaries, and communicate needs empowers survivors. “I have had to retrain myself to defend myself and recognize when I’m having, um, an intuition of fear…I have the tools and, um, capacity to communicate that versus being stuck.” Developing these skills is essential for self-protection and building healthy relationships.
9. Embracing Change and Recognizing Inner Strength
Katlyn offered a powerful message of hope and resilience. “The advice that I would give someone who is a survivor of anything traumatic is that things will change and that you deserve to see out the change…remind yourself how strong you are, how worthy you are.” Recognizing one’s inherent strength and the impermanence of difficult times fuels the ongoing journey of recovery. Even acknowledging the desire for change is a significant and brave first step.
Katlyn’s journey underscores that healing from trauma is a multifaceted process that requires courage, support, and self-compassion. By embracing these essential steps, individuals can begin to find their footing and move towards a more grounded and hopeful future.
Neurodivergent Symptoms: Insights and Resources for Enhanced Well-Being
Neurotypical people follow conventional paterns of thinking and behavior that align with societal expectations whereas neurodivergent brains function in unique ways. Neurodivergence is not a medical term, though some people with neurodivergence have a formal diagnosis of medical conditions like autism, ADHD, or dyslexia.
The idea of neurodiversity1 was introduced by Judy Singer in 1998 to highlight natural variation in brain development.
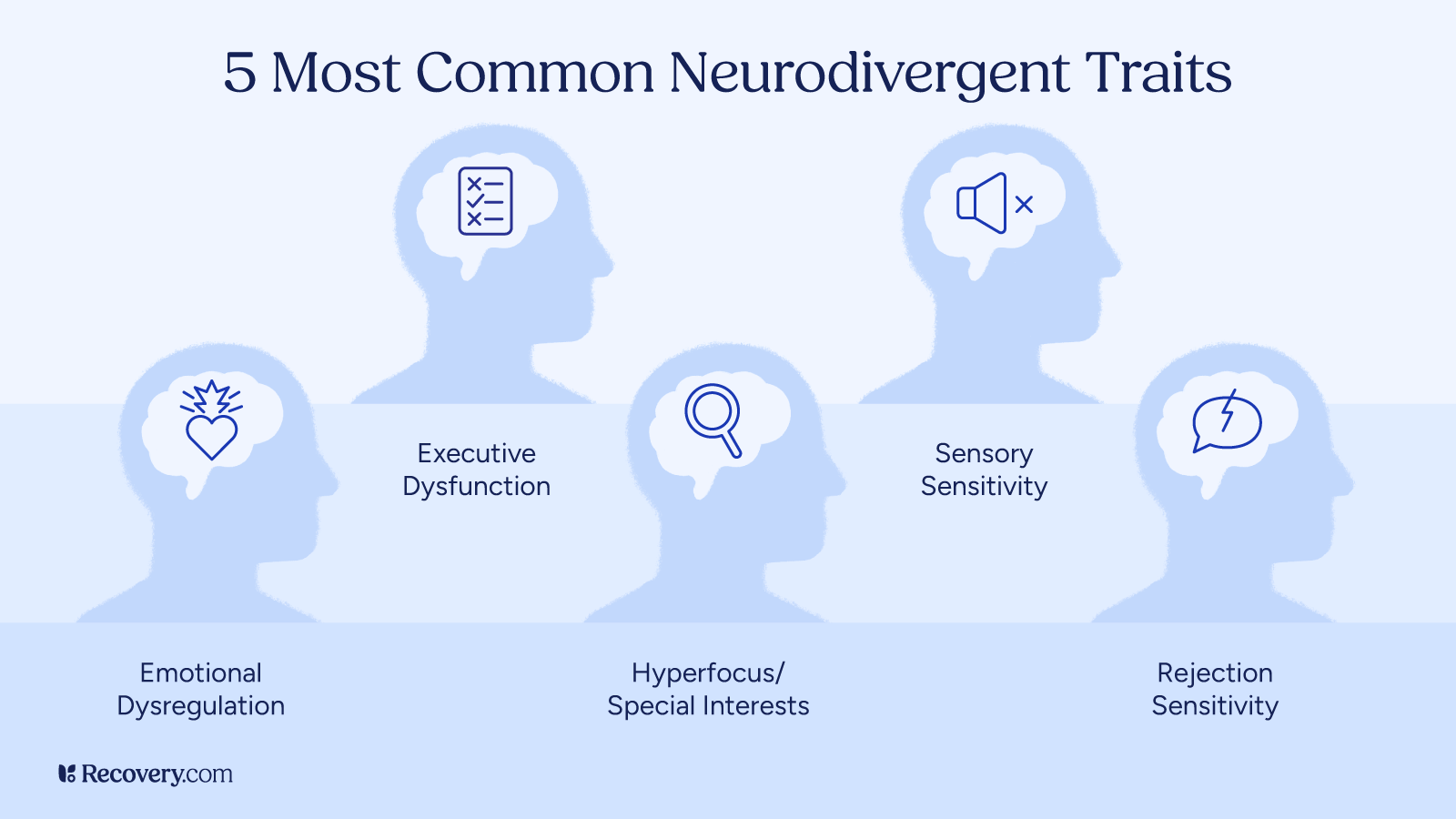
What It Means to Be Neurodivergent
Neurodivergent refers to individuals whose brains function differently from what is considered typical. This includes conditions like autism spectrum disorder (ASD), ADHD, dyslexia, and more.
These differences are not deficits, but rather natural variations in human brain function.
Neurodivergent individuals may face challenges2 in areas like communication, social interaction, or sensory processing, but they also possess unique strengths, such as creativity, problem-solving, or attention to detail.
People with neurodivergence can thrive by focusing on their abilities rather than limitations.
What are some effective strategies for supporting neurodivergent individuals in social settings, especially those struggling with social cues or anxiety?
When it comes to supporting neurodivergent people, it’s all about coming from a place of understanding and honoring neurocognitive differences. It’s not about teaching them how to socialize like a neurotypical person — it’s about guiding and supporting them so they can engage socially in ways that are meaningful to them.
When they understand their own sensory processing, they can begin to advocate for sensory-friendly environments when going out with friends. They may discover strategies or tools that support them socially, like fidgets, noise-dampening headphones, or choosing lower-stimulation settings.
Sarah Anderson, OTD, OTR/L | Elevated Wellbeing OT
Neurodivergent Conditions
The following are considered to be neurodivergent conditions:
- Autism spectrum disorder (ASD)
- Attention-deficit hyperactivity disorder (ADHD)
- Dyslexia
- Dyscalculia
- Intellectual disabilities
- Sensory processing disorders
- Social anxiety
Notably, neurodivergence is not a medical term but a framework for understanding diverse ways of thinking and processing the world.

Recognizing the Symptoms of Neurodivergence
Neurodivergence encompasses a range of cognitive and developmental conditions that can manifest in various ways.
Common conditions under this umbrella3 include autism, ADHD, dyslexia, dyspraxia, and dyscalculia. Each of these conditions presents a unique set of symptoms, but there are general patterns that may be signs of neurodivergence.
- People with autism often face challenges with understanding social cues which can make social situations uncomfortable and lead to difficulty in forming relationships. Additionally, people with autism and may display repetitive behaviors, demonstrate sensory sensitivities, and/or show intense interests in specific topics.
- ADHD is commonly associated with difficulty in sustaining attention, impulsivity, and hyperactivity, though individuals with ADHD may also exhibit periods of hyperfocus, especially on areas of interest.
- Dyslexia primarily impacts reading, spelling, and writing, with individuals often struggling with word recognition and decoding skills.
- Dyscalculia is often referred to as, “math dyslexia” and can make it challenging for individuals to understand number concepts, perform basic arithemtic, tell time, and/or estimate quantities.
- Dyspraxia affects coordination and motor skills, making everyday tasks like tying shoes or writing challenging for those affected.
While these neurodivergent symptoms may be noticeable from an early age, it’s important to recognize that they can vary significantly in severity from person to person.
Additionally, many neurodivergent individuals also experience co-occurring mental health conditions, such as anxiety or depression, which can further complicate symptom recognition. By understanding these diverse traits and challenges, we can better identify when someone may be neurodivergent and offer the right support and accommodations.
Impact on Daily Life
Being neurodivergent comes with both strengths and challenges that impact daily living.
Neurodivergent individuals often experience the world in unique ways, which can influence how they interact with their environment, approach tasks, and manage social situations. For instance, people with ADHD and autism have difficulties with time management, completing tasks, or understanding social cues.
Neurodivergence is often linked to an increased likelihood of experiencing mental health conditions like anxiety and depression. At the same time, neurodivergent people may demonstrate exceptional creativity, problem-solving abilities, or hyperfocus in certain areas of interest.
Ultimately, understanding and embracing neurodiversity can lead to better support systems in schools, workplaces, and social settings, helping individuals thrive despite these challenges.
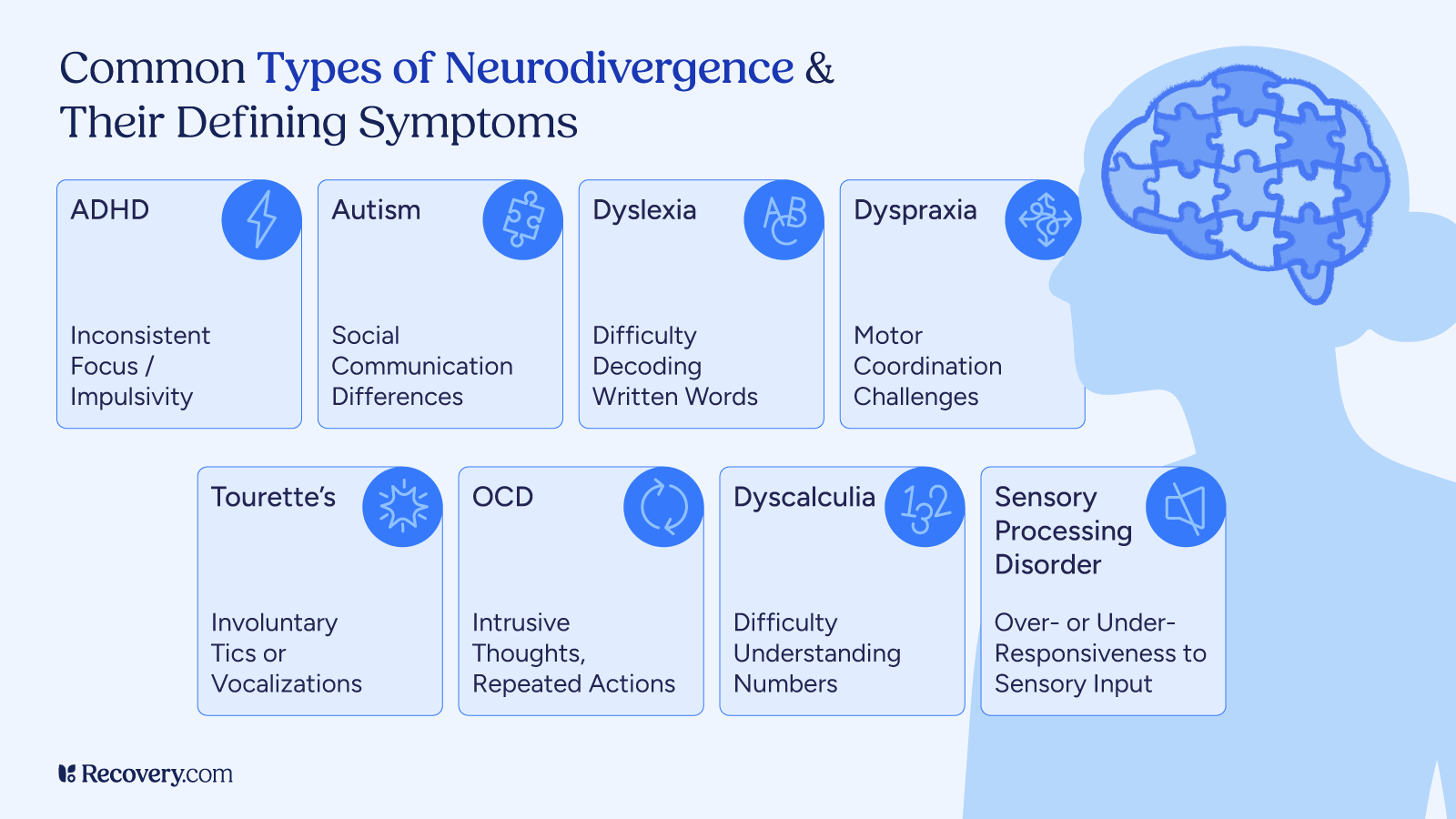
Mental Health, Addiction, and Neurodivergence
Neurodivergent individuals, particularly those on the autism spectrum, often face heightened mental health challenges, including higher rates of anxiety and depression. These difficulties are influenced by a range of neurodevelopmental, genetic, and environmental factors.
Personalized mental health support4 that is informed by neurodivergence, recognizes the unique ways brains work in neurodivergent individuals. It is crucial that healthcare professionals provide a personalized, holistic approach to treatment when supporting neurodivergent individuals in navigating their mental health struggles and fostering resilience.
While the connection between neurodivergence and addiction is complex, it’s essential to recognize that mental health challenges, and potential mental illnesses, faced by neurodivergent individuals can contribute to the risk of developing addictive behaviors. Co-occurring mental health conditions, such as anxiety or depression, may lead some individuals to turn to substances or other coping mechanisms as a way to manage their symptoms.
Understanding how neurodivergence and mental health challenges intertwine is key to developing effective strategies for addressing addiction in people with neurodivergence.
How can we best address the mental health challenges that often co-occur with neurodivergence, and what role do individualized support systems play in promoting well-being?
Many of the same evidence-based therapies that exist for anxiety, depression, PTSD, and other mental health challenges can be helpful for autistic and ADHD folks, as long as they’re provided in a neurodiversity-affirmative way. Dialectical Behavior Therapy, for example, can help many people who struggle with intense emotions or impulsivity, and it can be adapted to accommodate various sensory, learning, and executive functioning needs.
Therapy is always going to be most effective when the client believes the therapist understands them and is considering their unique preferences, values, and goals. Individualized support systems are so important for promoting well-being, for anyone, but especially for neurodivergent people.
Kiki Fehling, PhD, DBT-LBC
Embracing the Unique Strengths of Neurodiversity
Neurodivergent individuals are often misinterpreted and undervalued; there are many unique cognitive abilities that are frequently viewed as challenges rather than strengths.
Embracing neurodiversity means recognizing the value of the unique ways in which neurodivergent brains work such as exceptional creativity, attention to detail, and intense focus. These strengths can drive innovation and problem-solving in various fields, from technology to the arts.
By fostering inclusive environments that celebrate cognitive diversity throughout society including in schools, universities, and workplaces, we can unlock the full potential of neurodivergent individuals, benefiting both society and the economy. Understanding and embracing these differences in the ways people’s brains work helps create more inclusive spaces where everyone can thrive.
Tips for Promoting Inclusion
Promoting inclusion involves creating environments that recognize and embrace neurodiversity. For schools and workplaces, this means offering individualized support or reasonable accommodations, to ensure that neurodivergent individuals can fully participate and thrive. Encouraging neurodivergent individuals to share their unique perspectives can enhance creativity and problem-solving within teams, ultimately driving innovation.
Training staff and peers on neurodiversity, along with providing accessible resources, further empowers individuals to feel accepted and valued in their communities or workplaces.
It is crucial that all areas of society work to foster a culture of empathy and respect—where differences in thinking and learning are celebrated rather than viewed as deficits. This approach not only benefits neurodivergent individuals but enriches the broader environment by promoting understanding and reducing stigma.
What are some of the most common misconceptions about neurodivergence, and how can we work to challenge these misunderstandings in schools, workplaces, and society at large?
One of the biggest misconceptions about neurodivergence is that it only shows up as visible or disruptive behavior, when in reality, many people mask their differences to fit in, often at the cost of their mental health. Another is assuming neurodivergent individuals are either ‘too much’ or ‘not enough’, rather than recognizing their unique strengths. We can start to challenge these misunderstandings by listening to lived experiences, making room for multiple ways of thinking and processing, and shifting from compliance-based environments to connection-based ones.
Amanda Stretcher Lewis, MA, LPC-S | Crescent Counseling
Improving Well-Being
Improving the well-being of neurodivergent folks requires a multifaceted approach that focuses on enhancing personal strengths, developing appropriate coping mechanisms, and keeping executive functioning in check.
Key resilience factors,5 such as effective emotion regulation, self-determination, and self-understanding, play a crucial role in promoting mental health and quality of life. Neurodivergent individuals who develop strong emotional regulation and adaptive coping strategies are better able to manage stress, reduce anxiety, and improve their overall resilience.
Similarly, fostering self-esteem and self-efficacy—through a sense of agency and competence—has been linked to improved mental health outcomes, including better social functioning and reduced depressive symptoms.
Additionally, cultivating a positive self-identity, including embracing one’s neurodivergence, can contribute to a stronger sense of self-worth and resilience, buffering against the challenges that arise from societal stigma.
Participation in meaningful activities, including leisure, recreation, and community engagement, also plays a vital role in enhancing well-being. These activities not only improve social functioning and life satisfaction but also buffer against negative factors like depression and loneliness. Regular engagement in physical activities, in particular, has been shown to foster resilience, reduce stress, and improve both mental and physical health.
By focusing on building self-awareness, offering opportunities for growth, and ensuring access to supportive environments, it is possible to significantly enhance the well-being of neurodivergent individuals, promoting greater life satisfaction and emotional health.
FAQs
Q: What are 3 signs of being neurodivergent?
A: Neurodivergence can manifest in various ways depending on the individual and their specific condition. A person qualifies as neurodivergent if they process information differently from the general population. Three signs of being neurodivergent are:
- Behavioral traits that reflect atypical cognitive processing, such as challenges in social interactions, learning, or attention.
- Diagnosis of a neurodivergent condition (such as autism, ADHD, or dyslexia).
- Experiencing co-occurring conditions like anxiety or depression.
Q: What makes you considered neurodivergent?
A: You may be considered neurodivergent if you have a neurological condition that leads you to think or behave in ways that are different from the general population.
Q: What is a low-support neurodivergent?
A: A low-support neurodivergent individual is someone who, despite having a neurodivergent condition is able to manage day-to-day tasks, maintain executive functioning, and navigate social situations with minimal support. Many people considered to be low-support face challenges that are not always visible. Note that in the past, this was referred to as “high-functioning.” There is a move away from this language as some with personal experience note that determining a level of functioning does not always match the actual persons internal experience of their needs level.
Q: What is neurodivergence?
A: Neurodivergence refers to the natural variation in how people’s brains work, leading to unique ways of thinking, behaving, and learning. Conditions such as autism, ADHD, dyslexia, and others fall under the neurodivergent umbrella, challenging the concept of a “one-size-fits-all” way of thinking.
Q: Are people born with neurodiversity?
A: Yes, neurodivergence is often present from birth or early childhood. Some conditions, like autism, ADHD, and dyslexia, can be detected early, while others may become apparent as individuals grow older.
Neurodivergence is typically believed to be part of an individual’s genetic makeup, though environmental factors can also influence how traits manifest.
Q: What is regressive autism?
A: Regressive autism refers to a form of autism spectrum disorder (ASD) where children appear to develop typically for a period of time before losing previously acquired skills, such as speech or social abilities. This regression is a subject of ongoing research.
Q: What skills do neurodivergent people have?
A: Neurodivergent individuals often have exceptional skills, particularly in areas like attention to detail, creativity, problem-solving, and pattern recognition.
For instance, people with autism may have intense focus on specific topics, while individuals with ADHD may exhibit creativity and the ability to think outside the box.
Q: What does neurotypical mean?
A: Neurotypical refers to individuals whose cognitive functioning and behavior align with societal norms or expectations. They don’t have conditions like autism or ADHD that lead to unique ways of processing information, learning, or interacting socially.
Q: What are neurodivergent symptoms in adults?
A: In adults, neurodivergent traits may include unique challenges with time management, organization, maintaining focus, or navigating social relationships. These differences are part of the unique way in which you engage with the world and approach daily tasks.
It’s also common for adults with conditions like ADHD or autism to experience co-occurring mental health challenges, such as anxiety or difficulty managing stress.
Understanding these traits allows you to develop strategies that work for you and seek the support that empowers your well-being and success.
Q: How can I tell if I’m neurodivergent?
A: If you find that you approach focus, learning, social interaction, or communication in ways that are unique to you, you may be neurodivergent. These differences are part of the rich diversity of human experience and thinking.
Tools for self-assessment or evaluations from professionals can help you explore whether you identify with conditions like ADHD, autism, or dyslexia. While these traits often become apparent in childhood, they can also evolve and become clearer in adulthood, offering opportunities for self-discovery and growth.
Understanding these traits can empower you to embrace your strengths and seek support in areas where you may need it.
Q: How can I recognize neurodivergent traits in children?
A: In children, neurodivergent traits can manifest as unique ways of engaging with the world, such as deep and focused interests, heightened sensory awareness, and a distinctive approach to social interactions.
These children may demonstrate a strong ability to focus intensely on subjects they are passionate about, often displaying remarkable expertise in those areas.
While they may face challenges with attention, adapting to routine changes, or navigating social situations, these traits are part of their incredible diversity of thought and perspective.
Teen Depression: 5 Ways to Recognize the Signs and Support Your Child’s Mental Health
Depression in teens is a growing concern and causes can vary, significantly impacting their emotional health, academic performance, and social relationships. As they navigate the challenges of adolescence, feelings of sadness, hopelessness, or withdrawal can sometimes go unnoticed or be mistaken for typical teenage mood swings.
However, untreated depression can lead to serious consequences, including declining school performance, strained relationships, and even self-harm. Understanding the difference between occasional moodiness and clinical depression is crucial in ensuring that struggling teens receive the help they need.
This article explores the key signs of depression in teens, practical ways for parents and caregivers to support them, and when to seek professional intervention. By fostering open communication and creating a supportive environment, caregivers can play a vital role in helping teens navigate their mental health challenges and build resilience.
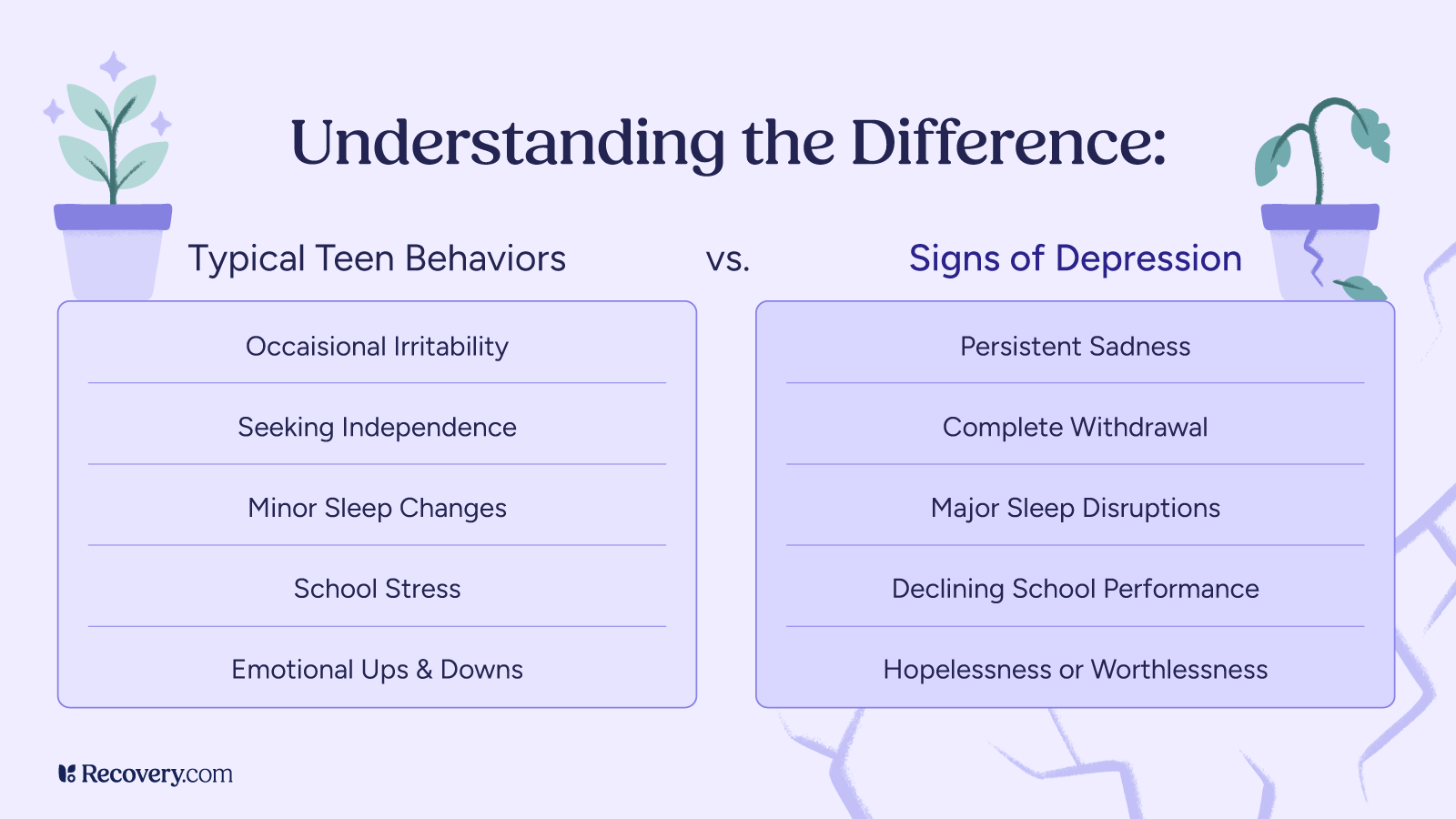
1. Recognizing the Signs of Depression in Teens
Emotional and Behavioral Signs
One of the most common symptoms of depression in teens is a persistent feeling of sadness, hopelessness, or irritability that lasts for weeks or even months. Unlike temporary mood swings that come and go, this emotional distress lingers and affects their overall outlook on life.
Teens struggling with depression may express feelings of worthlessness, despair, or a sense that things will never get better. They might also become more easily frustrated or lash out unexpectedly, even over minor issues, which can be mistaken for typical teenage behavior.
Another key indicator is a noticeable loss of interest in activities1 they once enjoyed or engage in risky behaviors. Whether it’s sports, hobbies, or social gatherings, they may withdraw from things that previously brought them happiness. This disengagement is often a sign that they are struggling to find motivation or pleasure in their daily lives.
Additionally, depressed teens tend to be more sensitive to rejection or perceived failure. Small setbacks—such as a poor grade, a disagreement with a friend, or not making a sports team—can feel overwhelming and trigger intense emotional responses. This heightened sensitivity can lead them to isolate themselves further, reinforcing feelings of loneliness and discouragement.

Physical and Cognitive Signs
Depression doesn’t just affect a teen’s emotions—it also takes a toll on their physical health. One of the most noticeable signs is a disruption in sleep patterns, which can manifest as sleeping too much or struggling with insomnia.
Some teens may spend excessive time in bed, feeling exhausted and unmotivated to get up, while others may lie awake for hours, unable to quiet their racing thoughts. Poor sleep can further contribute to irritability, difficulty concentrating, and an overall sense of exhaustion, making daily tasks feel overwhelming.
In addition to sleep disturbances, depression often leads to unexplained physical issues,2 such as headaches, stomachaches, or body aches. These symptoms may not have a clear medical cause, yet they persist and interfere with daily activities, sometimes leading to frequent absences from school. The cognitive effects of depression can also be profound, with teens struggling to focus, retain information, or make decisions.
They may find it difficult to complete schoolwork, follow conversations, or even make simple choices, such as deciding what to wear or eat. These challenges can lead to frustration and self-doubt, further impacting their academic performance and overall well-being.
What are the most effective ways for parents to approach a teen who is reluctant to talk about their depression?
Make sure to approach your teen in a setting where they feel safe and comfortable, free from pressure or distractions. Stay calm and open—focus on listening with curiosity rather than reacting, and notice your own emotional responses in the moment. Validate their feelings without pushing for details, letting them know you’re there when they’re ready. When appropriate, gently offer treatment options to support their autonomy and sense of control.
Sarah Anderson, OTD, OTR/L | Elevated Wellbeing OT
Social and Academic Indicators
Depression can cause young adults to isolate3 themselves, avoiding friends, family members, and social gatherings. They may prefer to spend time alone, withdrawing from relationships that once brought them joy. For some, excessive time on social media replaces in-person interactions, leading to deeper isolation. Mental health problems like adolescent depression also interfere with self-confidence, making depressed teens hesitant to participate in group activities, sports, or clubs. Over time, this social withdrawal can increase the risk of suicidal thoughts or self-harm, especially if they feel unsupported by peers or loved ones.
Academically, teen depression can result in declining grades, missed deadlines, and overall disengagement from schoolwork. Teachers and school counselors may notice sudden changes in participation, attendance, or motivation. Struggling students may experience mental disorders like major depression alongside other health conditions including addiction, making it difficult to focus or retain information. In severe cases, academic failure can contribute to thoughts of suicide, reinforcing the need for early intervention.
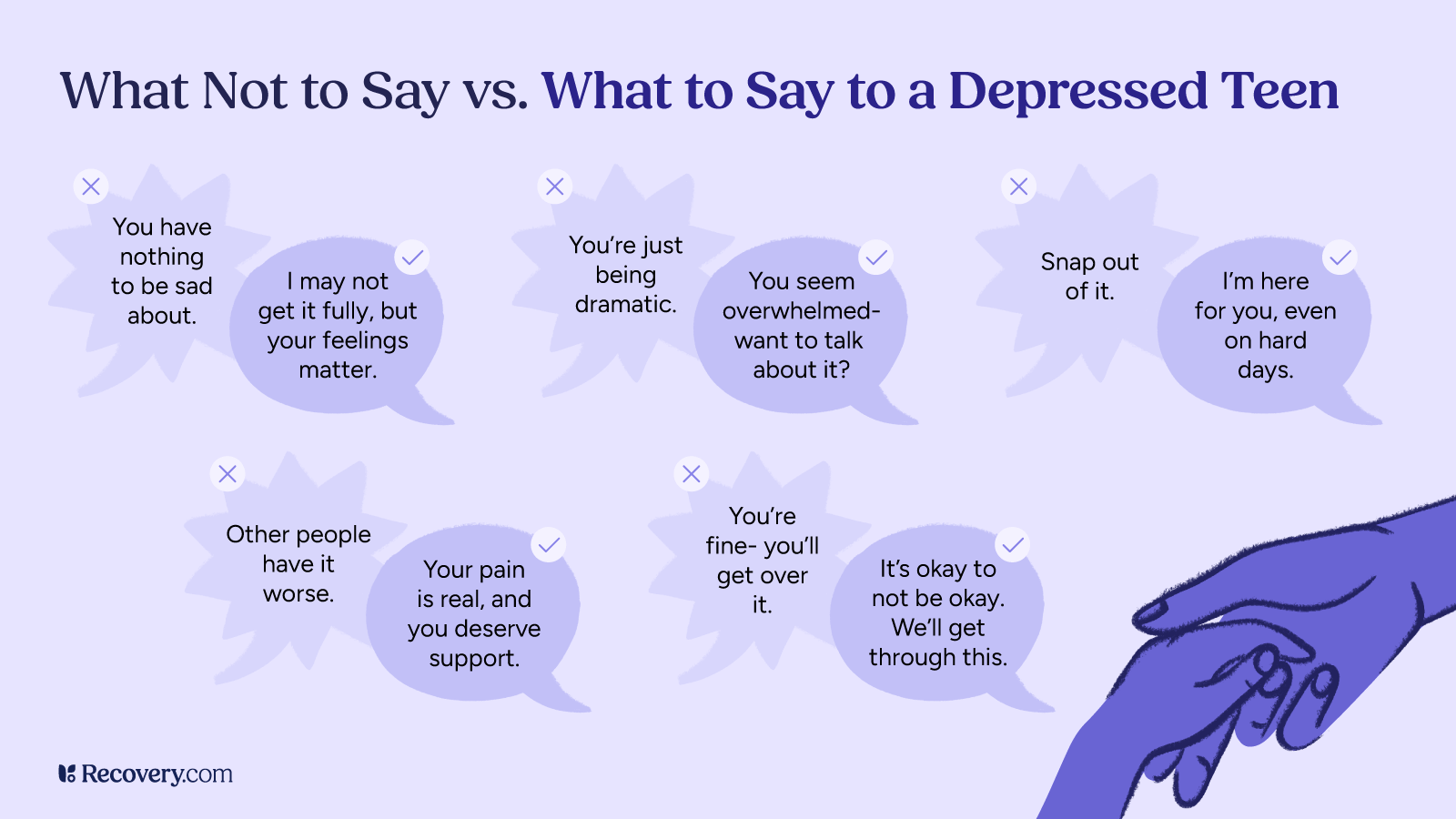
2. Creating a Supportive Environment
Open and Non-Judgmental Communication
One of the most important ways to support a teen feeling overwhelmed by depressive disorder is to create a safe space for open and judgment-free conversations. Many depressed teens struggle to express their emotions because they fear being misunderstood, dismissed, or seen as a burden. Family members and caregivers should encourage honest discussions about emotions without minimizing or invalidating what the teen is experiencing. Saying things like, “I hear you, and what you’re feeling is valid,” can help them feel supported rather than dismissed. It’s crucial to recognize that adolescent depression is more than just moodiness—it is a serious mental health problem that requires compassion and patience.
When a loved one opens up about their struggles, active listening is key. Instead of immediately offering solutions or trying to “fix” their emotions, simply acknowledging their pain can make a difference. Warning signs like expressions of hopelessness, thoughts of suicide, or feelings of worthlessness4 should never be ignored. If a teen expresses serious distress, it may be time to seek help from a mental health professional, such as a school counselor, therapist, or health care provider specializing in psychiatry.
How can caregivers differentiate between typical teenage mood swings and signs of clinical depression?
While mood swings are a normal part of adolescence due to fluctuating hormones and developmental changes, clinical depression has noticeable characteristics that impact more than just mood. Caregivers should pay attention to lasting changes in behavior such as isolation/withdrawal from family and friends, loss of interest in activities, changes in sleep or appetite, dramatic weight loss/weight gain, thoughts of hopelessness, or self-harm. If these symptoms last more than two weeks and interfere with daily functioning, it’s time to seek professional help. Trust your instincts! If something feels off, it’s always better to check in with a mental health provider as soon as possible.
Rebecca Tenzer, MAT, LCSW, CCTP, CGCS, CCATP, CCFP, CIMPH | Astute Counseling & Wellness Services
Building a Safe and Comforting Space
Maintaining a stable routine at home can provide a depressed teen with a sense of security and stability, which is especially important when they are struggling with mental health problems. Consistent meal times, a structured sleep schedule, and regular family interactions can help reduce feelings of uncertainty and stress. Additionally, encouraging positive coping mechanisms like journaling, art, or music can give them a healthy outlet to process their emotions.
These activities not only serve as forms of self-expression but can also support mental well-being by reducing anxiety and fostering creativity. Providing a nurturing and predictable environment can make a significant difference in helping a teen manage symptoms of depression and regain a sense of control over their life.
Promoting Healthy Habits
Encouraging regular physical activity, a balanced diet, and sufficient sleep can significantly improve a teen’s mental health, as exercise releases endorphins that help combat symptoms of depression. A nutritious diet supports brain function, while proper sleep is essential for emotional regulation and overall well-being.
Limiting excessive screen time and exposure to negative social media influences can help reduce anxiety, comparison, and isolation. Setting healthy boundaries around technology use encourages more meaningful real-world interactions and prevents mental health problems linked to social media overuse.
3. Encouraging Professional Help
Knowing When to Seek Help
If a teen’s symptoms of depression persist for more than two weeks and begin to interfere with their daily life, school, relationships, or overall well-being, it may be time to seek professional support. Signs such as ongoing low self-esteem, withdrawal from activities, and a decline in schoolwork could indicate the need for depression treatment. If they express suicidal thoughts, engage in self-harm, or talk about feeling hopeless, immediate intervention is crucial.
Types of Professional Support
- Therapy Options: Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) are effective in helping teens develop coping strategies,5 challenge negative thought patterns, and regulate emotions.
- Medication: Health care providers or psychiatrists may recommend antidepressant medication to help balance brain chemistry, though it is important to monitor for any side effects.
- School and Community Resources: Guidance counselors and support groups offer immediate assistance for teens in distress. Additionally, local mental health organizations and online resources agencies, such as the National Institute of Mental Health, provide valuable education and access to professional care. Suicide prevention resources, such as the 988 Suicide & Crisis Lifeline, can provide immediate support, while long-term depression treatment may include CBT, interpersonal therapy, support groups, or antidepressant medication.
Reducing the Stigma of Mental Health Treatment
It’s important to normalize therapy and medication as valid and effective forms of support for teen depression, just as we do for physical health conditions. Seeking help from a mental health professional, engaging in psychotherapy, or using antidepressant medication when prescribed by a health care provider should be seen as responsible steps toward healing rather than signs of weakness.
Sharing stories of public figures,6 role models, or even loved ones who have successfully managed depressive disorders can help reduce stigma and encourage teens to seek help without fear of judgment. Celebrities, athletes, and influencers who openly discuss their experiences with major depression, CBT, or interpersonal therapy can inspire young people to recognize that they are not alone and that recovery is possible with the right treatment options and support.
4. Strengthen the Parent-Teen Relationship
Balancing Support and Independence
Offering guidance to a depressed teen is crucial, but it’s important to do so without being overbearing or making them feel pressured. Providing gentle support, checking in regularly, and reminding them that help is available can make a significant difference in their mental well-being. At the same time, respecting their need for privacy is essential, as pushing too hard may cause them to withdraw even more. Staying engaged in their life—whether through casual conversations, shared activities, or simply being present—ensures they feel supported while maintaining a sense of independence.
Encouraging Social Connections
Supporting friendships and activities that boost self-esteem can help a depressed teen feel more connected and valued. Encouraging them to spend time with loved ones and engage in positive social interactions can counter feelings of isolation often associated with teenage depression.
Group hobbies like sports, clubs, or volunteering provide opportunities to build meaningful relationships while fostering a sense of accomplishment and belonging. These activities improve mental well-being and serve as healthy distractions from negative thoughts and mental health problems.
Monitoring Without Controlling
It’s important to stay aware of any noticeable shifts in a teen’s mood disorder symptoms, such as increased withdrawal, persistent sadness, or sudden behavior changes. Regular gentle check-ins can help them feel supported without making them feel pressured or scrutinized. Instead of invasive questioning, asking open-ended questions like, “I’ve noticed you seem a bit down lately—do you want to talk about it?” can encourage them to share their feelings in a safe and comfortable way.
What immediate steps should parents take if they suspect their teen is having suicidal thoughts?
Listen without judgment or emotional reactivity, as best you can–they need to be heard at this time without loud noises or raised voices. If the child is unsure that they can keep themselves safe, take them to the emergency room immediately for a psychiatric evaluation. If the child has self-harmed, calmly ask the following: Where? What did you use? Where is the weapon now?
Then, take steps to remove the weapon as well as potential weapons from the child’s reach by placing those objects in a lock box. This may seem inconvenient, but it is necessary to keep the child safe. Ensure the child will not act on any urges moving forward. Look into local Intensive Outpatient programs for mental health and schedule a screening as soon as possible. These 3-hour, daily therapeutic programs offer close monitoring, meetings with a psychiatrist, and individual plus group therapy offerings where the child will learn several skills to manage self-harm urges or suicidal ideation, and the family will learn how to best support their child during this difficult time.
Jennifer Chicoine, MA, LCPC, CCTP | Peaceful Healing Counseling Services
5. Address Crisis Situations
Recognizing Warning Signs of Suicide or Self-Harm
It’s crucial to recognize warning signs that may indicate a teen is struggling with suicidal thoughts or engaging in self-harm. Expressions of hopelessness, feeling like a burden, or frequently talking about death can be red flags that they need immediate support. Additionally, actions such as giving away personal possessions, saying goodbye in a meaningful way, or suddenly withdrawing from loved ones could signal an urgent need for intervention and professional help.
Taking Immediate Action
If a teen shows warning signs of suicidal thoughts or self-harm, it’s essential to stay calm and approach the conversation with empathy and openness. Creating a safe environment by removing access to harmful objects, substances, or anything they could use to hurt themselves can help prevent impulsive actions. If they express suicidal intent, seeking immediate professional help—whether by contacting a crisis hotline like the 988 Suicide & Crisis Lifeline, taking them to the emergency room, or reaching out to a mental health professional—can be life-saving.
Help is Available
Helping a depressed teen requires patience, empathy, and ensuring they have access to the right mental health resources. Providing early intervention and consistent emotional support can significantly improve their ability to cope with symptoms of depression and prevent their struggles from worsening. By fostering a safe, open, and nonjudgmental environment, we can empower teens to navigate teenage depression, seek help when needed, and build resilience for the future.
FAQs
Q: What is teen depression?
A: Teen depression is a serious mental health condition that affects how a teenager thinks, feels, and behaves. It goes beyond typical mood swings and involves persistent sadness, irritability, and loss of interest in activities, interfering with daily life and development.
Q: What are the symptoms of major depression in a teen?
A: Symptoms of major depression7 in teens include:
- Persistent sadness or hopelessness
- Irritability or anger
- Withdrawal from friends and activities
- Changes in appetite or sleep patterns
- Difficulty concentrating
- Low energy or fatigue
- Feelings of worthlessness or guilt
- Thoughts of self-harm or suicide
These symptoms must last at least two weeks and significantly impact functioning.
Q: What are the signs and symptoms of depression?
A: In addition to emotional changes, signs of depression may include physical complaints (like headaches or stomachaches), academic decline, social withdrawal, and changes in behavior such as reckless or risky actions.
Q: Is my teenager depressed or just moody?
A: It can be difficult to distinguish normal teenage moodiness from depression. If your teen’s sadness, irritability, or withdrawal lasts more than two weeks and interferes with school, relationships, or daily activities, it may be clinical depression and worth seeking help.
Q: What causes depression in teens?
A: Depression in teens can result from a combination of factors, including:
- Genetic predisposition or family history
- Hormonal changes
- Traumatic experiences or adverse childhood events
- Ongoing stress (e.g., academic pressure, bullying)
- Co-occurring conditions like anxiety or ADHD
Q: What are the five main causes of depression?
A: The most common contributing causes of depression include:
- Genetics and family history
- Brain chemistry imbalances
- Environmental stressors
- Trauma or abuse
- Chronic illness or substance use
Q: What are the coping skills for depression?
A: Effective coping skills include:
- Practicing mindfulness or meditation
- Engaging in regular physical activity
- Creating a consistent sleep schedule
- Journaling or expressing emotions through art
- Talking with a trusted friend, family member, or therapist
- Limiting social media use and screen time
Q: How can I support my teenager who is struggling with depression?
A: Support starts with creating a safe, open environment for communication. Listen without judgment, encourage healthy habits, validate their feelings, and seek professional support if symptoms persist. Be patient and consistently present.
Q: How do you help someone with depression who doesn’t want help?
A: Begin by expressing concern calmly and compassionately. Avoid forcing treatment but gently offer support and encourage small steps, like talking to a school counselor or joining a peer support group. Sometimes involving a trusted adult or professional can help open the door.
Q: When should I call my teen’s healthcare provider?
A: Contact your teen’s provider if you notice:
- Persistent sadness or hopelessness
- Withdrawal from activities or people
- Sudden changes in behavior or performance
- Expressions of self-harm or suicidal thoughts
Early intervention can make a significant difference in recovery and well-being.
