Life with anxiety and panic attacks can feel like navigating a minefield of unpredictable triggers and overwhelming sensations. For Stanley, his experience was marked by a constant fear of impending death fueled by health anxiety. “Life before my recovery journey was such a scary time,” he recalls. “It was so many different new things that were happening to me. So many new sensations that I was going through. And to always feel as if, at least for me in my head, I felt like, oh my god, I’m gonna die. I’m gonna die.” This intense fear, coupled with the difficulty of explaining his internal turmoil to others, left him feeling isolated and desperate.
Stanley’s story, however, is also one of hope and recovery. He bravely sought help and embarked on a journey that led him to a place where anxiety no longer dictates his life. His insights offer valuable guidance for anyone struggling with similar challenges. Here are 7 key steps, inspired by Stanley’s experience, to help you find your calm and navigate the path to recovery from panic attacks and anxiety.
1. Recognizing When Enough Is Enough
The turning point for Stanley came when his anxiety began to severely impact his daily life. Simple activities like showering became overwhelming, and leaving the house felt impossible.
“I knew it was time to get some help when I couldn’t do regular everyday things anymore,” he explains. “When it would be hard for me to take a shower. I remember my body used to be so overstimulated that even warm water would make me feel more anxious or just feeling my heart beating so fast. Literally, it would stop me from being able to take a shower.”
Recognizing when anxiety is significantly disrupting your ability to function is the first crucial step towards seeking help. Don’t wait until you feel completely overwhelmed; acknowledging the impact of anxiety on your life is a sign of strength, not weakness.
2. Reaching Out for Support
Stanley’s decision to reach out for help was pivotal. He contacted his school’s counseling department and connected with a therapist. “What I did to help me up on a path of recovery is that I reached out to a therapist. I reached out to my school at the time,” he shares.
This proactive step demonstrates the power of seeking professional guidance. Therapists are trained to understand anxiety disorders and can provide evidence-based strategies and support tailored to your specific needs. Recovery.com can help you find mental health professionals and support resources.
Additionally, Stanley found it helpful to communicate his struggles to friends and professors, fostering a supportive environment. Sharing your experiences with trusted individuals can alleviate feelings of isolation and encourage understanding.
3. The Power of Breath
One of the foundational tools Stanley learned in his recovery journey was the importance of mindful breathing. “Are you breathing properly? Are you taking deep breaths? That has saved me a million times over.”
Deep, diaphragmatic breathing can activate the parasympathetic nervous system, which helps to calm the body’s stress response. When you focus on your breath, you bring yourself into the present moment, disrupting the cycle of anxious thoughts about the future or worries about the past. Studies have highlighted the effectiveness of breathing exercises in reducing anxiety symptoms1. Practice taking slow, deep breaths, inhaling through your nose and exhaling slowly through your mouth, to anchor yourself in the present.
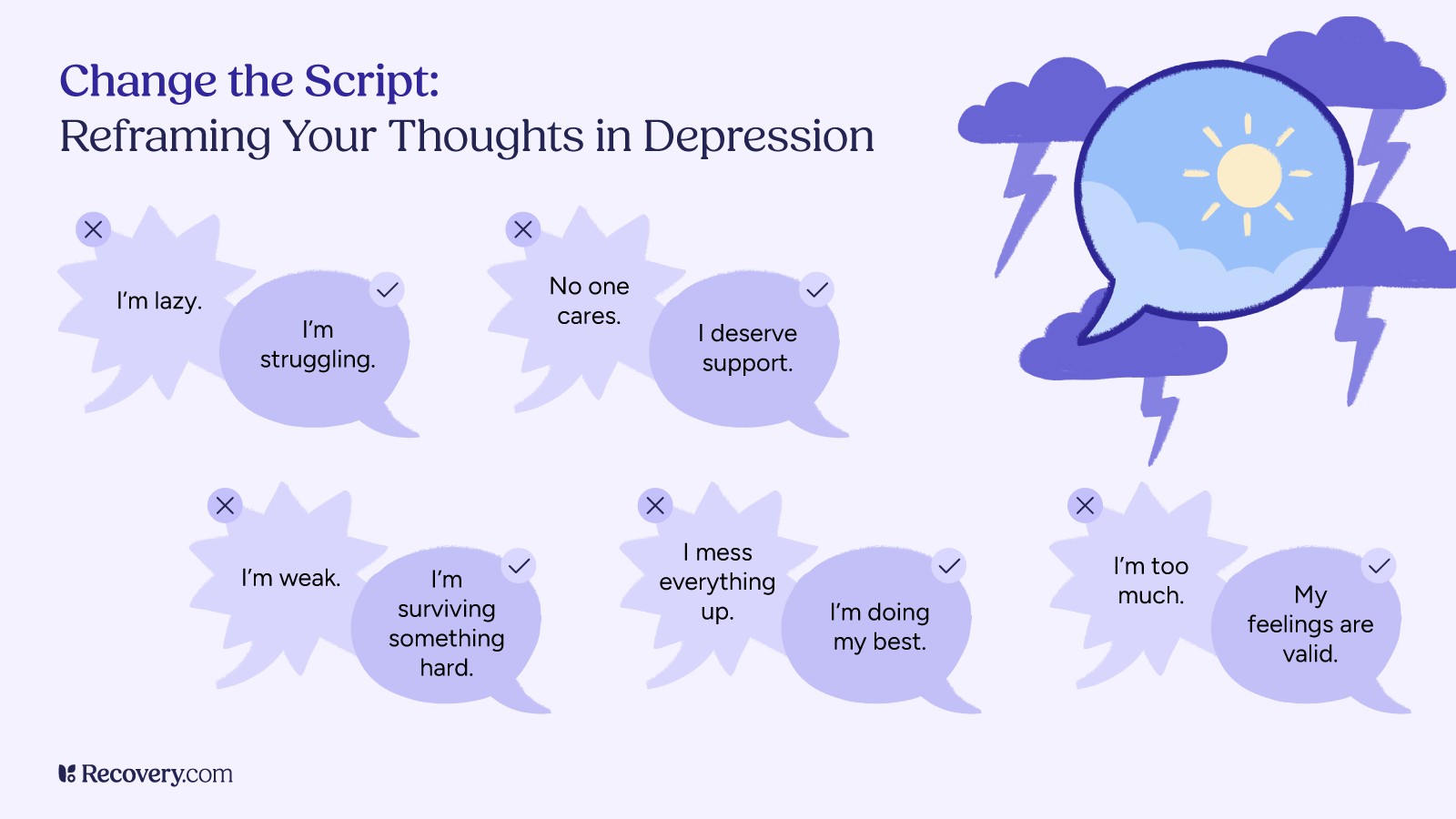
4. Reframing Your Thoughts
Anxiety often involves negative thought patterns that can fuel panic and distress. Stanley learned to observe his thoughts and challenge their validity. “If you are in your body, and if you’re in the present moment, then you’re able to observe your thoughts, and you’re able to say, Hey, I’m thinking negative right now. Is that a thought that I wanna have?” This mindful awareness allows you to identify and interrupt negative thought loops before they escalate.
Cognitive Behavioral Therapy (CBT), a common therapeutic approach for anxiety, focuses on identifying and modifying these unhelpful thought patterns. By consciously reframing negative thoughts into more balanced and realistic ones, you can gradually reduce their impact on your emotional state.
5. Learning to Accept, Not Fight
A key insight Stanley gained in therapy was to shift his relationship with panic attacks from resistance to acceptance. His therapist’s advice was transformative: “‘Don’t fight the panic attack. Feel it, let it process through. You don’t judge it.’ And that’s easier said than done, obviously, if you feel like your world is coming to an end. But, in therapy, my therapist said that when you feel anxiety, tell it to come on more. Say, come on, gimme more. Gimme more. I want more.”
This counterintuitive approach can be incredibly powerful. Fighting anxiety often intensifies it, creating a cycle of fear and avoidance. By learning to accept the physical sensations of anxiety without judgment and reminding yourself that they are temporary and not dangerous, you can reduce their power over you.
6. Cultivating Self-Compassion
Living with anxiety can be emotionally draining, and it’s crucial to practice self-compassion. Stanley’s journey highlights the importance of being kind and understanding towards yourself. “Love on yourself and know that you deserve help, you deserve support. You doing this is in the best interest of yourself. It’s loving yourself, and it’s taking care of yourself to get help.”
Recognize that experiencing anxiety is not a sign of weakness or failure. Treat yourself with the same kindness and understanding you would offer a friend going through a difficult time.
7. Embracing Hope and Progress
Stanley’s life today is a testament to the possibility of recovery. “My life now is so much better,” he shares. “Of course I still experience anxiety from everyday challenges and living in general, but I rarely ever have panic or anxiety attacks anymore. And if I do, I know how to bring myself down from them with all the tools and everything that I’ve learned.”
Recovery is not always linear, and there may be ups and downs. However, with consistent effort, self-awareness, and the right tools, it is possible to significantly reduce the impact of anxiety on your life. Embrace the progress you make, no matter how small it may seem, and hold onto hope for a calmer and more fulfilling future. Find anxiety treatment options.
In conclusion, Stanley’s powerful message to those on the fence about seeking help underscores the transformative potential of recovery: “I promise you it’s so worth it. You learn so much about yourself, who you are as a person, your history. You’re gonna feel so much better. You’re gonna thank yourself. Your future self is thanking you right now. You never know how beneficial it’s gonna change your life for the better.” Take that courageous first step, knowing that you are not alone and that a brighter future is within reach.