Mixing Xanax and alcohol is more common than you might think—and that’s concerning because this combination carries some serious risks. Both substances affect your brain in similar ways, and when they’re taken together, they can amplify each other’s effects to a potentially life-threatening degree.
Most people don’t realize that having “just a few drinks” while taking Xanax can harm their health.
Some people mix these substances on purpose; others don’t fully understand their risks. Either way, the combination can cause lasting damage to your physical and mental health.
We’ll help you understand how Xanax and alcohol affect your body, why the combination is so risky, and how to get help if you’re concerned that you or your loved one is becoming dependent.

What Happens When You Mix Alcohol and Xanax?
When you mix Xanax (the brand name for alprazolam) and alcohol, you’re combining two substances that both slow down your central nervous system. Xanax works by boosting the effects of GABA1 (Gamma-aminobutyric Acid), a natural neurotransmitter that reduces brain activity. Alcohol affects many of the same brain systems, also increasing GABA’s effects while blocking other brain chemicals.
This creates what behavioral health experts call a synergistic effect. This means that when combined, Xanax and alcohol don’t just add their effects together—they multiply them. This is why the combination is especially dangerous.
Why do people mix Xanax and alcohol?
People mix Xanax (alprazolam) and alcohol primarily for enhanced sedative effects, as both substances depress the central nervous system which can lead to increased relaxation, euphoria, or intoxication. Some individuals may do this intentionally to heighten the effects, while others may mix them unintentionally, not realizing how dangerous the combination can be. It is important to ask what intention the person had when mixing the substances or if it was consumed unintentionally.
Andrew J. Schreier, ICS, CSAC, LPC, ICGC-II, BACC
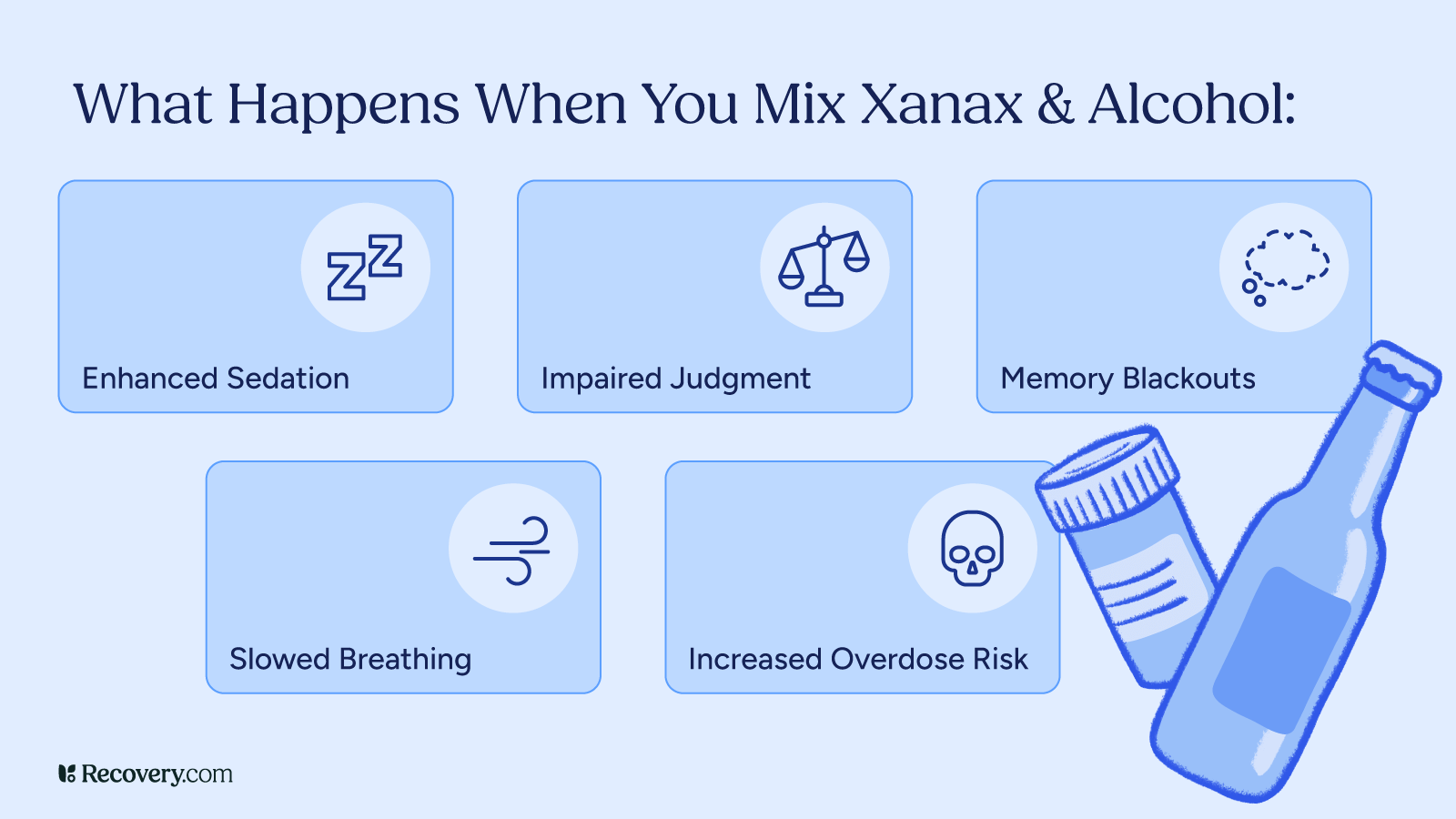
1. Enhanced Sedation
Both Xanax and alcohol are central nervous system depressants2 that cause sedation on their own. When combined, this sedative effect becomes much stronger.
You might feel extremely drowsy, dizzy, or uncoordinated. Tasks that require alertness, like driving or using machinery, become highly dangerous. Even just walking around normally is more dangerous, as you’re more likely to fall and hurt yourself.
2. Life-Threatening Breathing Problems
One of the most life-threatening side effects of mixing Xanax and alcohol is respiratory depression—when your breathing becomes dangerously slow or shallow. Both substances suppress the part of your brain that controls breathing.
Together, they can slow your breathing to the point where your body doesn’t get enough oxygen, potentially leading to brain damage, coma, or death.
When combined, Xanax and alcohol suppress your autonomic respiratory drive.3 That means they interfere with the brain stem’s ability to detect carbon dioxide in your blood—the primary trigger that tells your body to breathe. Without this signal functioning properly, your breathing can slow or even stop completely without even feeling like you’re having trouble breathing.
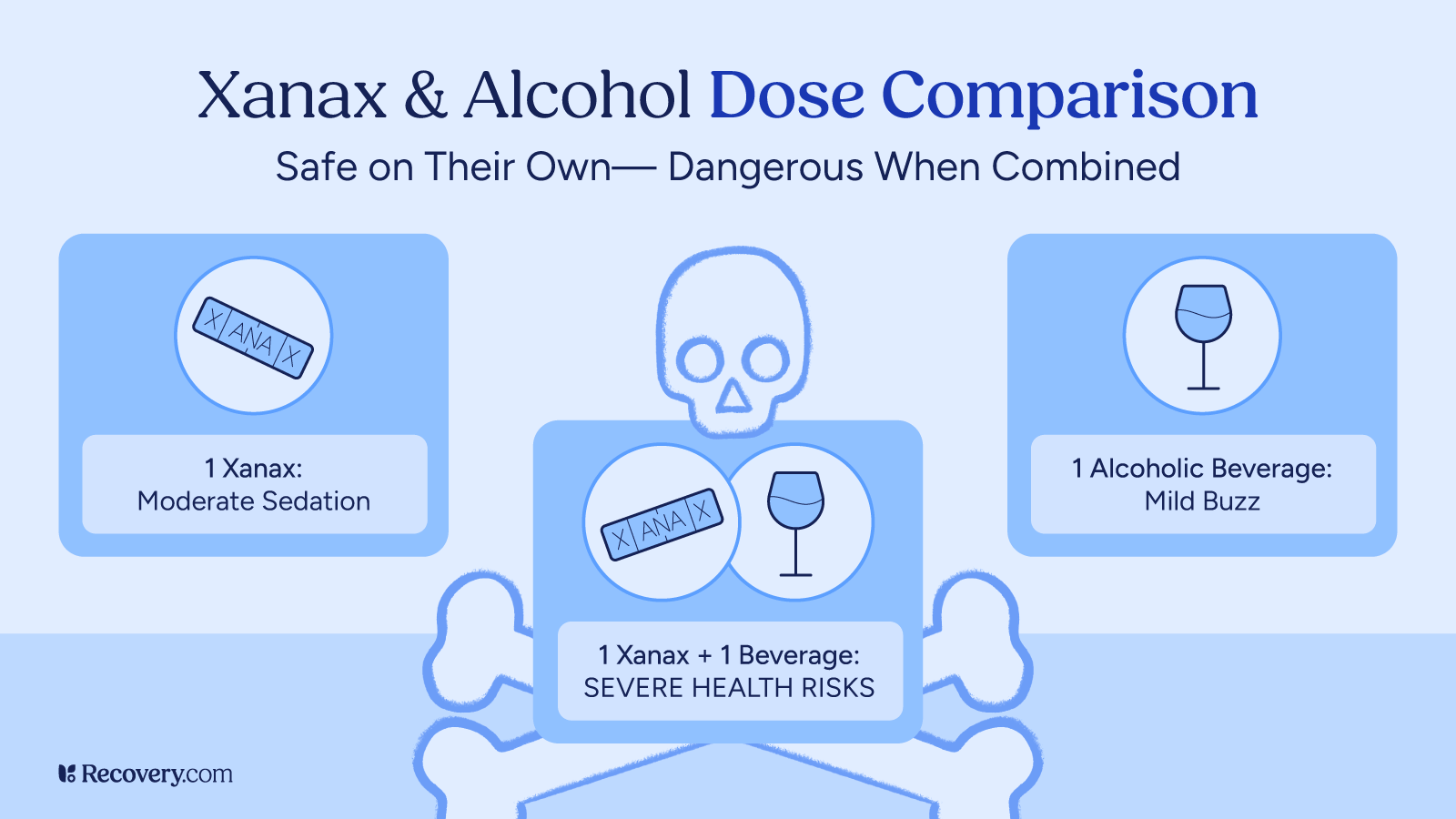
3. Increased Overdose Risk
This combination increases your risk of overdose. Even amounts of each substance that would be safe individually can become deadly when combined. In fact, one report finds Alprazolam (Xanax) is even more toxic than other benzodiazepines in overdose,4 warning that “severe toxicity is often related to co-ingestants, especially alcohol.”
This is particularly dangerous because the effects of alcohol and Xanax can be unpredictable—what might seem like a small amount of alcohol can dramatically increase the effects of Xanax in your system.
Maybe you’ve taken your normal prescribed dose of Xanax with a moderate amount of alcohol before without serious consequences. But taking higher doses, changes in your physical condition, timing between doses, or even what you’ve eaten that day can suddenly make the same amounts deadly.
4. Memory Impairment and Blackouts
Both Xanax and alcohol affect your memory. Used together, they can cause severe memory problems. You might find yourself having more blackouts or periods of time you can’t remember at all.
One participant in a study on benzo use by young people in the UK5 reflects on his experience with frequent blackouts:
I don’t know how many memories or experiences I have lost due to my benzo use back then, but they are parts of my life that I will never be able to get back.
These memory gaps can be frightening—and potentially dangerous—if you made decisions or took actions you can’t recall.
What are the risks of combining alcohol and Xanax?
In your brain, alcohol increases the release of the neurotransmitter GABA, which produces slower brain activity that you perceive initially as relaxation. But both alcohol and Xanax also enhance the effect of the GABA-A receptor, making the increased GABA levels much more potent. This creates a particularly dangerous situation since a dose of either Xanax or alcohol that might be “safe” on its own can combine in the brain in dramatically more powerful and unpredictable ways. They also have synergistic effects on muscle control, short-term memory, judgment, and breathing- meaning that alcohol and Xanax are incredibly dangerous and potentially fatal when combined.
W. Lee Warren, MD
5. Behavioral Changes
Over time, the combination of substances can cause noticeable changes in how you feel and act. You might become more aggressive, emotional, or take risks you normally wouldn’t. Severely impaired judgment can lead you to make poor decisions with lasting consequences. While most people start taking Xanax for anxiety or panic disorders, abusing Xanax can make you feel more anxious or agitated rather than calmer.
Why Do People Mix Xanax and Alcohol?
People mix Xanax and alcohol for several reasons, often without realizing how serious the risks are.
- Seeking Stronger Effects: Some people combine these substances intentionally to feel a stronger effect. Since both Xanax and alcohol reduce anxiety and make you feel relaxed, some people think taking them together will increase these pleasant feelings. They might be seeking deeper relaxation or trying to escape stress, anxiety, or other emotional discomfort.
- Self-Medication: Someone whose prescribed Xanax isn’t fully controlling their anxiety disorder might drink alcohol for additional relief. This often happens when anxiety breaks through between doses6 or when someone has developed tolerance to their medication.
For more information on how substances can interact with each other and affect your body’s response to medication, see our article on cross-tolerance. Understanding this concept is especially important if you take Xanax or other prescription drugs.
- Unintentional Mixing: Many people mix these substances unintentionally. Someone might take their prescribed Xanax and later attend a social event where they have a drink, not realizing the interaction they’re creating. Others might simply not know about the risks or might think that “just one drink” won’t cause problems.
- Social Pressure: Social pressure can play a role too. In settings where drinking is expected, someone who takes Xanax might feel awkward explaining why they can’t drink, especially if they don’t want to discuss their mental health.
Regardless of the reason, mixing Xanax and alcohol is never safe, even in small amounts—the risks far outweigh any perceived benefits.
How Long After Taking Xanax Can You Drink?
If you’re taking Xanax, you might wonder if there’s a safe time to wait before having alcohol. The short answer is that there’s no truly safe window—the risks remain even after you think the Xanax has worn off.
Xanax has what medical professionals call a half-life, which is how long it takes for half of the drug to leave your system. For Xanax, the average half-life is about 11 hours,7 but this can range from 6 to 27 hours depending on several factors.
This means that even if you took Xanax in the morning, a significant amount could still be in your body when you have a drink that evening.
A few factors affect how long Xanax stays in your system:
- Your age (older adults eliminate the drug more slowly)
- Your liver function (liver problems can slow down elimination)
- Your weight and metabolism
- Whether you’re taking other medications that interact with Xanax
- How long you’ve been taking Xanax (regular users may metabolize it differently)
Even if you can’t feel the long-term effects of Xanax, the drug is still in your body and can still interact with alcohol. Just because you don’t feel sedated from a dose you took earlier doesn’t mean it’s safe to drink.
If you’re taking Xanax, it’s best to avoid alcohol completely. If you’re concerned about interactions, talk to your healthcare provider about your specific situation.
How do you treat alcohol and Xanax addiction?
Xanax and alcohol use can lead to psychological and physiological dependence after long-term use. If a person is thinking about quitting Xanax or alcohol after prolonged use, it is crucial for them to consider the need for medically monitored withdrawal management, as these are two substances that can lead to death as a result of withdrawal. It’s important to assess the history of withdrawal, the intensity of those experiences, and the need for current medical support. Post-withdrawal management placement criteria should be performed to assess the level of care a person may need to move forward with their recovery goals. Outpatient and residential treatment, individual therapy, and self-help groups are all appropriate levels of care for people who struggle with Xanax and alcohol addiction.
Tanya Kraege LCSW, CSAC, CCAR RC, WI CPS | Ventus Rex
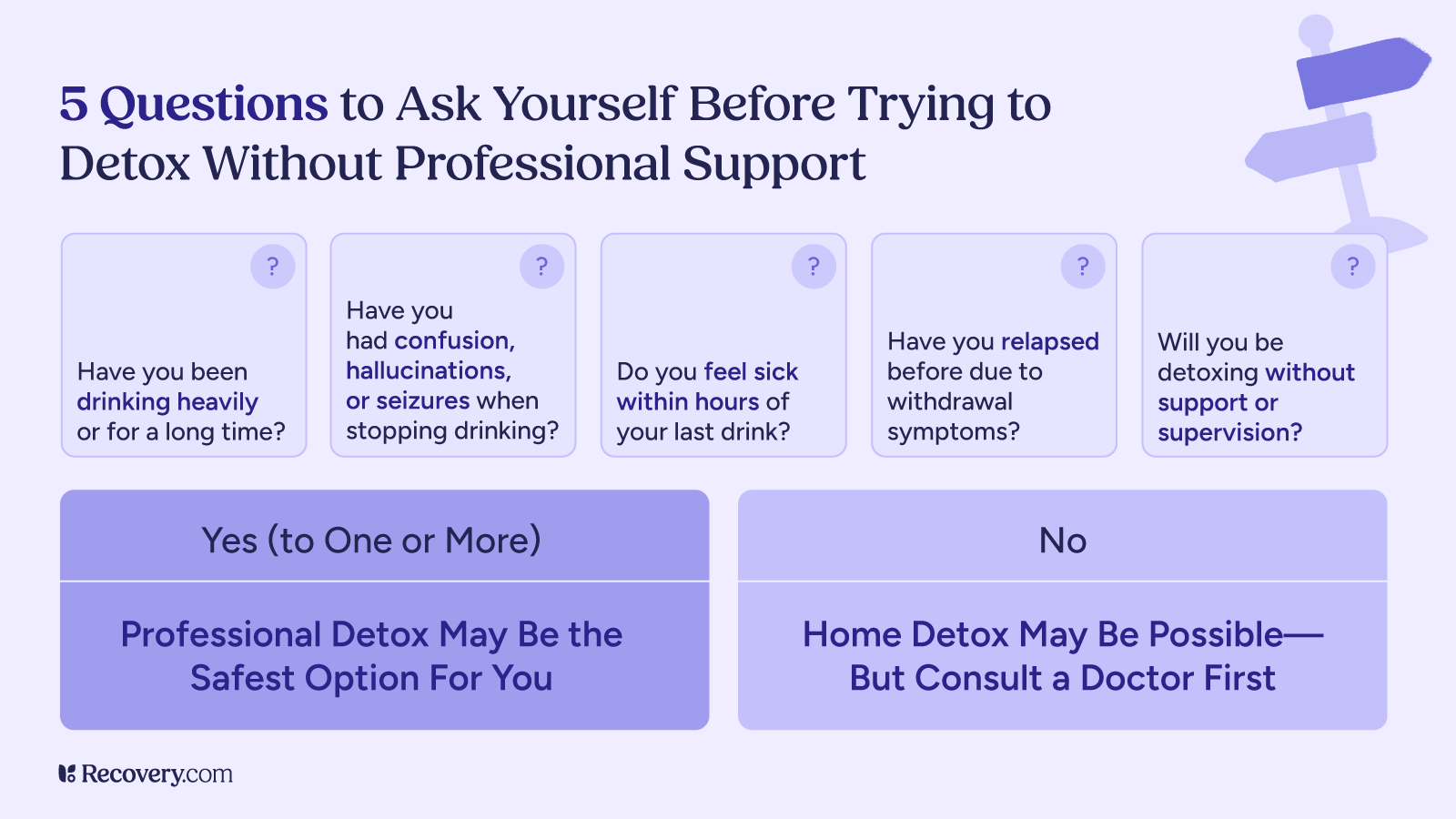
Do You Need Medical Detox for Alcohol and Xanax?
If you’ve been using both Xanax and alcohol regularly, especially in combination, you should not try to quit on your own. Withdrawal from either substance can be dangerous, but withdrawing from both at the same time can be life-threatening.
Withdrawal symptoms from Xanax8 and alcohol can include:
- Seizures
- Hallucinations
- Severe anxiety and panic
- Dangerous changes in blood pressure and heart rate
- Delirium tremens (DTs),9 a severe (and potentially deadly) symptom of alcohol withdrawal
Professionally supervised detox is a safe environment where healthcare specialists can monitor your health and help you manage withdrawals. In a medical detox program, your doctor may give you medications to ease withdrawal symptoms and prevent complications.
Detox typically lasts 5-7 days but can take longer depending on your history of use. During this time, your medical team will gradually taper your dosage to minimize symptoms as your body adjusts to functioning without these substances.
After detox, it’s important to continue with a comprehensive treatment program to address your underlying reasons for substance use and learn strategies for long-term recovery.
Treatment Options for Alcohol and Xanax Addiction
Recovery from Xanax and alcohol addiction involves several phases of treatment:
Medication-Assisted Treatment
Some medications can help manage cravings and support recovery. While there are no specific medications approved for benzodiazepine addiction, certain medications may help with anxiety symptoms or co-occurring conditions.
If you’re curious about medication options that can help with recovery from substance abuse, see our article on medication-assisted treatment (MAT) to learn if this approach might be right for you.
Inpatient Rehab
In inpatient Xanax and alcohol rehab, you live onsite and receive round-the-clock care in a structured, substance-free environment. Residential rehab typically lasts 30 to 90 days and includes:
- Evidence-based and holistic therapies
- Addiction education and recovery coaching
- Learning and practicing healthy coping skills
- Treatment for co-occurring mental health conditions
Outpatient Programs
For those with less severe substance use disorders or who have completed inpatient treatment, outpatient programs allow you to live at home while attending treatment sessions several times a week. These programs offer similar therapies to inpatient care but with more flexibility.
Support Groups and Aftercare
Long-term recovery often involves ongoing support through:
- Ongoing one-on-one therapy
- Alumni programs through your treatment center
- Meeting regularly with sober community via AA, SMART Recovery, or other support groups
- Building your social support network
The best treatment plans are individualized and created specifically for you and your unique situation. They don’t just focus on helping you stop using substances—they also address any underlying trauma or mental health concerns that might have led you to use them in the first place. Everyone’s journey to well-being looks different, and finding the right combination of support is the key to long-term success.
Ready to find help for Xanax and alcohol use disorder? Our treatment finder can show you rehab options that match your location and specific needs—just a few clicks can connect you with centers that can help.
FAQs
Q: What happens when you mix alcohol and anxiety medication?
A: When you combine alcohol with anxiety medications like Xanax, you significantly increase the sedative effects of both substances. This can lead to extreme drowsiness, breathing problems, memory impairment, and increase your risk of overdose. The combination affects brain function more severely than either substance alone and can be life-threatening even “moderate” amounts.
Q: Do people go to rehab for Xanax?
A: Yes, many people go to rehab specifically for Xanax addiction. Benzodiazepine addiction is a serious condition that often requires professional help to overcome safely. Because Xanax withdrawal can be dangerous, addiction specialists typically recommend medically supervised detox, followed by comprehensive addiction treatment that addresses both physical dependence and underlying causes.
Q: Can you drink on Xanax if you wait long enough?
A: There is no completely safe time frame for drinking after taking Xanax. Even if you wait 24 hours or longer, residual amounts of the drug may remain in your system. Individual factors like age, liver function, and metabolism affect how long Xanax stays in your body. The safest approach is to avoid alcohol completely while taking Xanax.
Q: What are the main risks of combining Xanax and alcohol?
A: The main risks include respiratory depression (dangerously slow breathing), enhanced sedation, memory blackouts, impaired coordination, behavioral changes, increased addiction risk, and increased risk of fatal overdose. This dangerous combination creates unpredictable effects that can vary significantly from one person to another.