A podcast dedicated to reducing the isolation and stigma of depression, one story at a time. Listen to our latest episode below, or search for “Giving Voice to Depression” wherever you listen to podcasts to access 400 other interviews in our archive.
4 Stages of Alcoholism: What to Know About How Drinking Problems Evolve
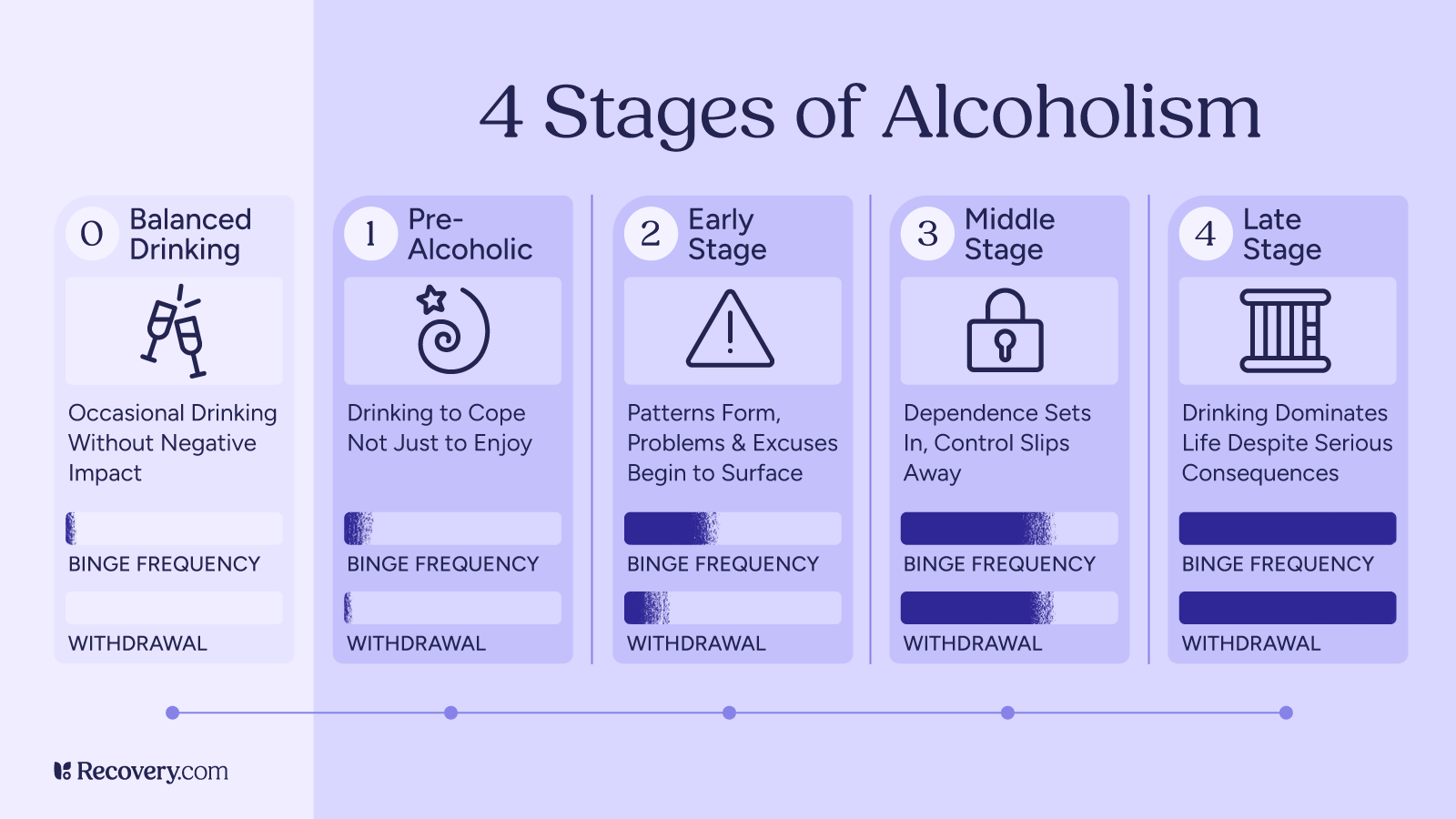
Alcoholism doesn’t happen overnight. For many people, it develops gradually through several stages, each with its own set of signs and challenges. Understanding these stages can help you recognize problems in yourself or your loved one and intervene before the consequences get worse.
The Disease Model: How Alcoholism Progresses
This framework for understanding alcoholism progression comes from E.M. Jellinek, the first to propose the disease model of alcohol addiction that’s now widely accepted by medical professionals. His model outlines 4 distinct stages that show how alcohol dependence develops.1
Let’s break down each stage in simple terms so you know what to watch for.
Stage 1: Pre-Alcoholic Stage
In this early stage, a person starts using alcohol not just for enjoyment, but to feel better. They might drink to relax after work or to feel more comfortable at parties. This might not seem like a problem yet, but it’s the start of using alcohol as a solution rather than a choice.
Signs you might be in the pre-alcoholic stage:
- You look forward to drinking alcohol as a way to unwind or feel comfortable
- You can handle more alcohol than before (increased tolerance)
- You sometimes drink alone
- You finish alcoholic beverages faster than others around you
- You feel a little anxious when you can’t drink
Most people in this stage still function normally in daily life. Friends or family may not notice anything unusual about your drinking habits.
This is the easiest stage to make changes. Try setting limits on your drinking, tracking how much you consume, or finding alcohol-free ways to relax and socialize.
Alcohol use doesn’t just suddenly become a problem—issues with alcohol use can build slowly over time, in ways that are easy to overlook. By understanding the stages of alcoholism, we can better identify early warning signs and intervene before more challenges and consequences occur.
— Caroline Beidler, MSW
Stage 2: Early Stage
In the early stage, casual drinking shifts toward a more concerning pattern and early warning signs begin to appear. The person develops regular drinking routines, and alcohol starts causing problems.
Finding the Right Support
- You experience occasional blackouts (can’t remember what happened while drinking)
- You feel defensive when someone mentions your drinking
- You make excuses for drinking or downplay how much you consume
- Your relationships start to suffer because of alcohol
- You drink to deal with problems caused by previous drinking
During this stage, a dangerous cycle begins. Drinking causes problems, which creates stress, which leads to more drinking to cope with that stress. Getting help at this stage is still relatively easy, and the chance of successful recovery is high with proper support.
Stage 3: Middle Stage
The middle alcoholic stage (or “crucial” stage) is when physical dependence takes hold. Your body now expects alcohol regularly, and you feel uncomfortable without it. Many people realize they have a problem at this point and try to control their drinking.
Signs of the middle stage:
- You feel withdrawal symptoms when you’re not drinking2 (shakiness, anxiety, sweating)
- You’ve tried to cut back or quit but couldn’t maintain it
- You hide your drinking from others
- You sometimes need a morning drink to steady your nerves
- You black out more often
- You feel deep shame or guilt about your drinking
- Hangovers get worse because your body’s ability to process alcohol is compromised as liver function declines
- Physical health problems start to appear
People often try ineffective methods to control their drinking, like switching from liquor to beer or limiting drinking to weekends. These attempts usually fail without adequate support.
Many people in this stage keep up appearances outwardly while struggling privately. They might hold down jobs and maintain relationships—however problematic—while denying the severity of their problem.3
Stage 4: Late Stage
The late stage (or “chronic” stage) is when alcohol abuse completely takes over and a person feels a total loss of control over their drinking. It’s no longer a choice but a powerful compulsion that directs most of their decisions and behaviors.
Signs of the late stage:
- You can’t control when or how much you drink
- You have severe withdrawals when not drinking
- You’ve abandoned activities and interests you once enjoyed
- Your work performance has significantly declined
- Relationships are severely damaged or broken
- You continue drinking despite serious physical and mental health problems
- You may have had alcohol-related legal issues like DUIs
Alcohol-related health complications4 are an increased risk at this stage. Liver damage or cirrhosis, heart problems, digestive bleeding, and changes in brain function are common. You may have visible symptoms even when you’re not drinking.
Despite how serious this stage is, recovery is still possible with professional help. Medical treatment is usually necessary, starting with medically supervised detox followed by comprehensive addiction treatment.
Things began innocently enough when I began drinking socially in high school, but quickly escalated when I realized how much more confident I felt when intoxicated. It was a bad combination that I used for many years in social settings, to numb out “bad feelings” and ultimately use alcohol as daily self-medication. I trained my brain and body to think they “needed” alcohol for any kind of stressful situation or negative emotion. This was very destructive for me and eventually I had to make a change or I didn’t know what might progress even further.
— Ericka Anderson
Understanding Alcohol Addiction
Substance use is commonplace in many aspects of our daily lives. From celebrating achievements to unwinding after a stressful day, drinking is normalized in ways that can mask developing problems. This cultural acceptance can make it hard to recognize when casual drinking is crossing into problematic territory.
Health experts increasingly recognize “gray area drinking“—a space between moderate consumption and severe alcohol use disorder. In this middle ground, you might not meet the clinical criteria for addiction, but your relationship with alcohol is causing subtle problems in your health, relationships, or daily functioning.
Many people exist in this gray area without realizing it: The 2023 National Survey on Drug Use and Health by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) found that 10.2% of people in the U.S had an alcohol use disorder.5 People regularly exceed the limits for moderate drinking (or even heavy drinking or binge drinking) without noticing. (According to medical guidelines, moderate drinking6 means up to 1 drink daily for women and 2 for men.)
While most people can drink moderately without causing immediate problems in their lives, research increasingly shows there is no completely “safe” amount of alcohol consumption7 when it comes to long-term health outcomes.
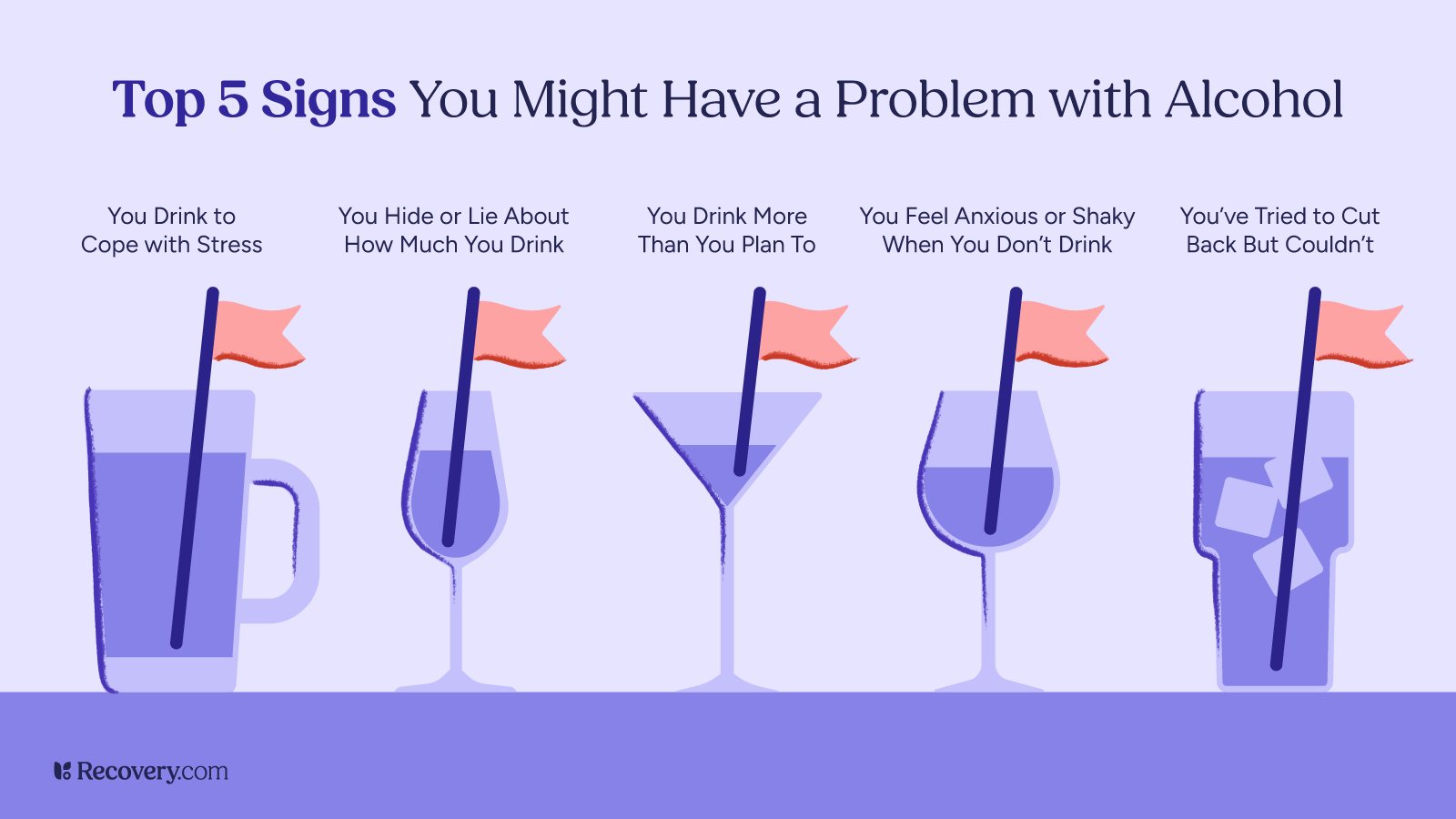
Consider these warning signs about your drinking habits:
- Do you often drink more or for longer than planned?
- Have you found it hard to stop or cut back, despite wanting to?
- Do you find yourself preoccupied with thoughts of drinking?
- Have you noticed yourself prioritizing drinking over activities or hobbies you used to enjoy?
- Are your relationships with family or friends being affected by your alcohol misuse?
- Do you sometimes take risks while drinking, like driving or having unsafe sex?
- Do you need more drinks to feel the same effects of alcohol?
- When you stop drinking, do you have any physical discomfort like shakiness, trouble sleeping, or nausea?
If you answered yes to more than one of these questions, it could indicate problem drinking.8 Recognizing these patterns doesn’t necessarily mean you have a diagnosable addiction, but they are important signs that your relationship with alcohol could benefit from some attention and possibly professional help.
Recovery Is Possible at Any Stage
No matter which stage of alcoholism you may be experiencing, recovery is always possible. Many people have found their way to healthier, happier lives after struggling with alcohol, and you can too.
Alcohol treatment options include:
- Medical detox to safely manage alcohol withdrawal and cravings
- Inpatient alcohol rehab for structured, intensive care
- Outpatient programs that allow you to live at home while attending intensive therapy
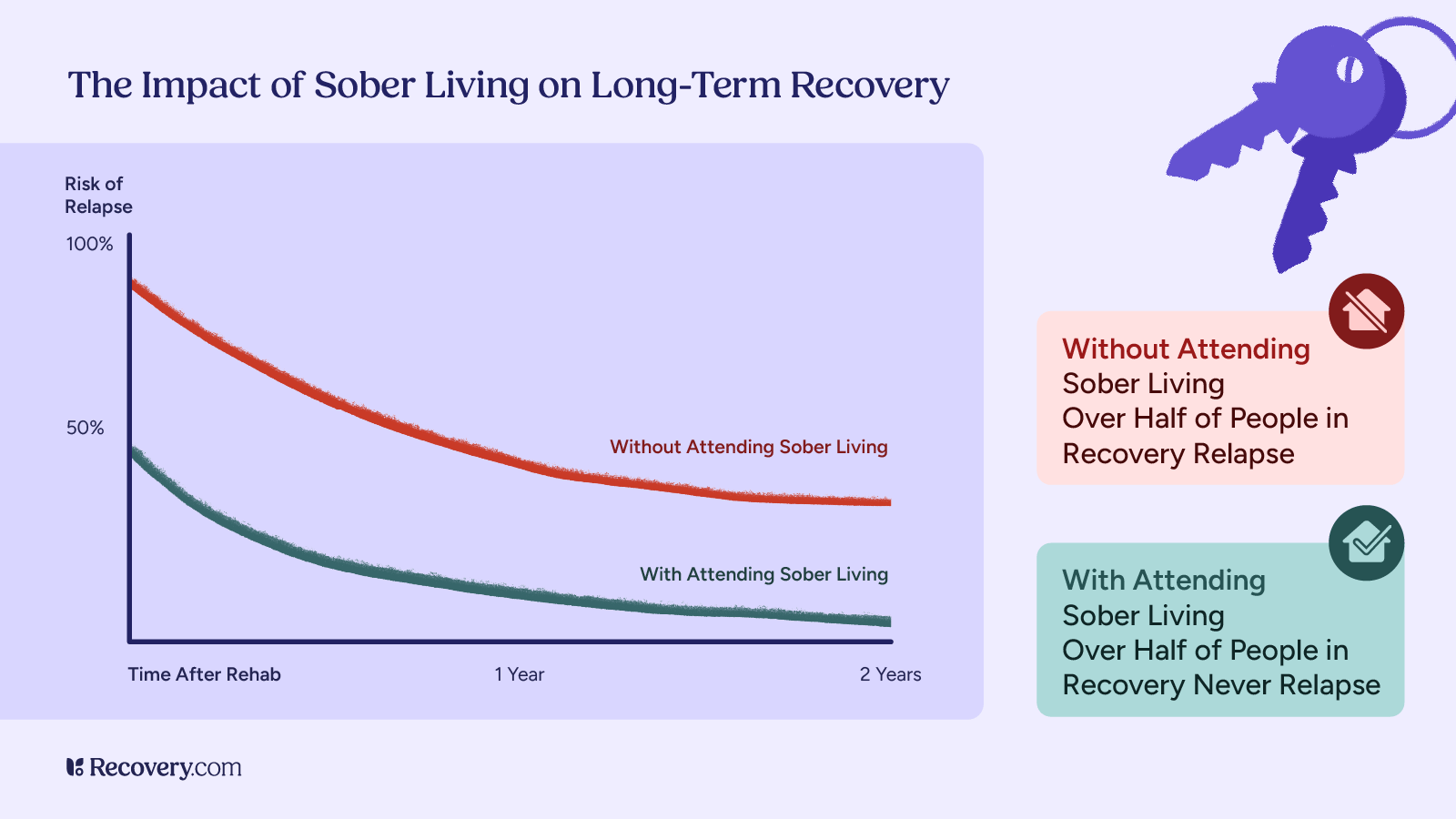
- Sober living homes that provide a supportive, alcohol-free environment as you transition to independent living
- Continuing care: Ongoing counseling, support groups like AA or SMART Recovery, and social support
These resources can help you start the process:
- Your primary care doctor (who can refer you to addiction specialists)
- The Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline: 1-800-662-HELP (4357)
- Local Alcoholics Anonymous (AA) or other support group meetings
Wondering what might work best for you? Check out our complete guide to finding an addiction treatment program for an easy-to-use breakdown of programs, costs, and how to choose the right fit for your needs.
Recovery is not only possible, it is probable when we have the right supports and treatment.
— Caroline Beidler, MSW
A Note on the Modern Understanding of Alcohol Use Disorder
While Jellinek’s stages offer a helpful framework for understanding how alcohol problems typically progress, modern medicine has evolved toward a more nuanced approach. The current Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR) views alcohol problems as existing on a spectrum9 rather than in distinct stages.
Today, healthcare professionals diagnose alcohol use disorder (AUD) as mild, moderate, or severe based on how many criteria a person meets out of 11 possible symptoms. This spectrum approach recognizes that alcohol problems can develop in different ways for different people. Some individuals may experience certain symptoms but not others, and the progression isn’t always linear. Both models offer valuable perspectives for understanding how casual drinking can develop into more serious problems over time.
Find the Right Support for Your Journey
If you’re concerned about your relationship with alcohol, reaching out for professional guidance is a great first step. Whether your goal is to reduce harm from drinking or stop entirely, an addiction specialist can point you in the right direction and help you stay on track.
Our addiction treatment finder helps you explore options that match your specific needs, connecting you with qualified treatment providers who can support your path to a healthier life.
FAQs
Q: What are the 4 stages of alcoholism?
A: The 4 stages of alcoholism in Jellinek’s disease model are:
- Pre-alcoholic stage, where drinking is used to cope with stress
- Early stage, where patterns form and blackouts may begin
- Middle stage, where physical dependence develops with withdrawal symptoms
- Late stage, where excessive drinking becomes compulsive and health complications become serious
Q: How does alcohol addiction progress through different stages?
A: Alcohol addiction typically begins with using alcohol to cope with problems (pre-alcoholic stage). It progresses to regular patterns of drinking that cause life problems (early stage), then to physical dependence with withdrawal symptoms (middle stage), and finally to compulsive drinking despite serious consequences (late stage).
Q: What are the early signs of alcohol dependence?
A: Early signs of alcohol dependence include:
- Needing more drinks to feel the same effect (increased tolerance)
- Looking forward to drinking as your main way to relax
- Drinking alone more frequently
- Feeling anxious when you can’t drink
- Occasional blackouts
- Becoming defensive when others mention your drinking
Q: How can I identify the different stages of alcoholism?
A: You can identify the stages of alcoholism by looking for specific signs:
- Pre-alcoholic stage shows increased tolerance and drinking to cope
- Early stage includes blackouts and making excuses for drinking
- Middle stage involves withdrawal symptoms and failed attempts to quit
- Late stage is marked by compulsive drinking, severe health conditions, and an inability to control consumption
Q: What is late-stage alcoholism and what are the effects?
A: Late-stage alcoholism involves compulsive drinking where a person loses control over their alcohol consumption. Side effects include severe withdrawal symptoms, abandoned interests and activities, declining work performance, broken relationships, serious health complications (liver damage, heart problems, brain damage), and alcohol-related legal issues.
Q: Where can I find help for alcohol addiction?
A: Help for alcohol addiction is available through your primary care doctor, local support groups, and specialized treatment centers. Recovery.com is here to help. Options range from medical detox and inpatient programs to outpatient care and harm reduction approaches like setting drinking limits or creating alcohol-free days.
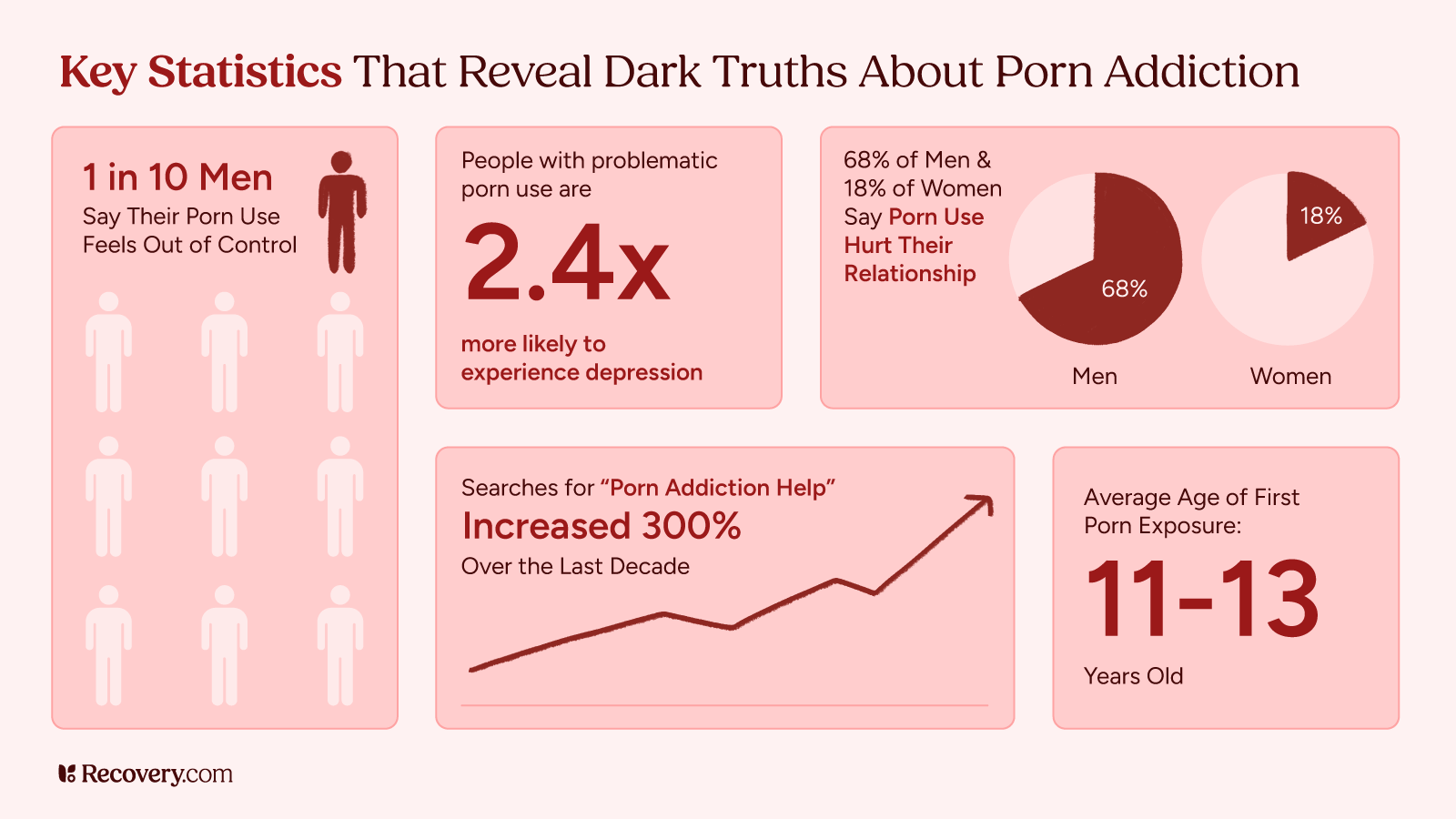
Porn Addiction: 9 Signs and How It Impacts Your Well-Being
Porn addiction, like other behavioral addictions, can negatively impact mental health, relationships, and daily life. But how do you know if you have a problem? Are there signs that can help you determine if you or a loved one has a porn addiction?
If this issue impacts you, a loved one, or friend, you are not alone. Recognizing the signs of porn addiction is the first step in seeking professional help and treatment options.
What are the top 10 signs of pornography addiction and how they affect overall well-being?
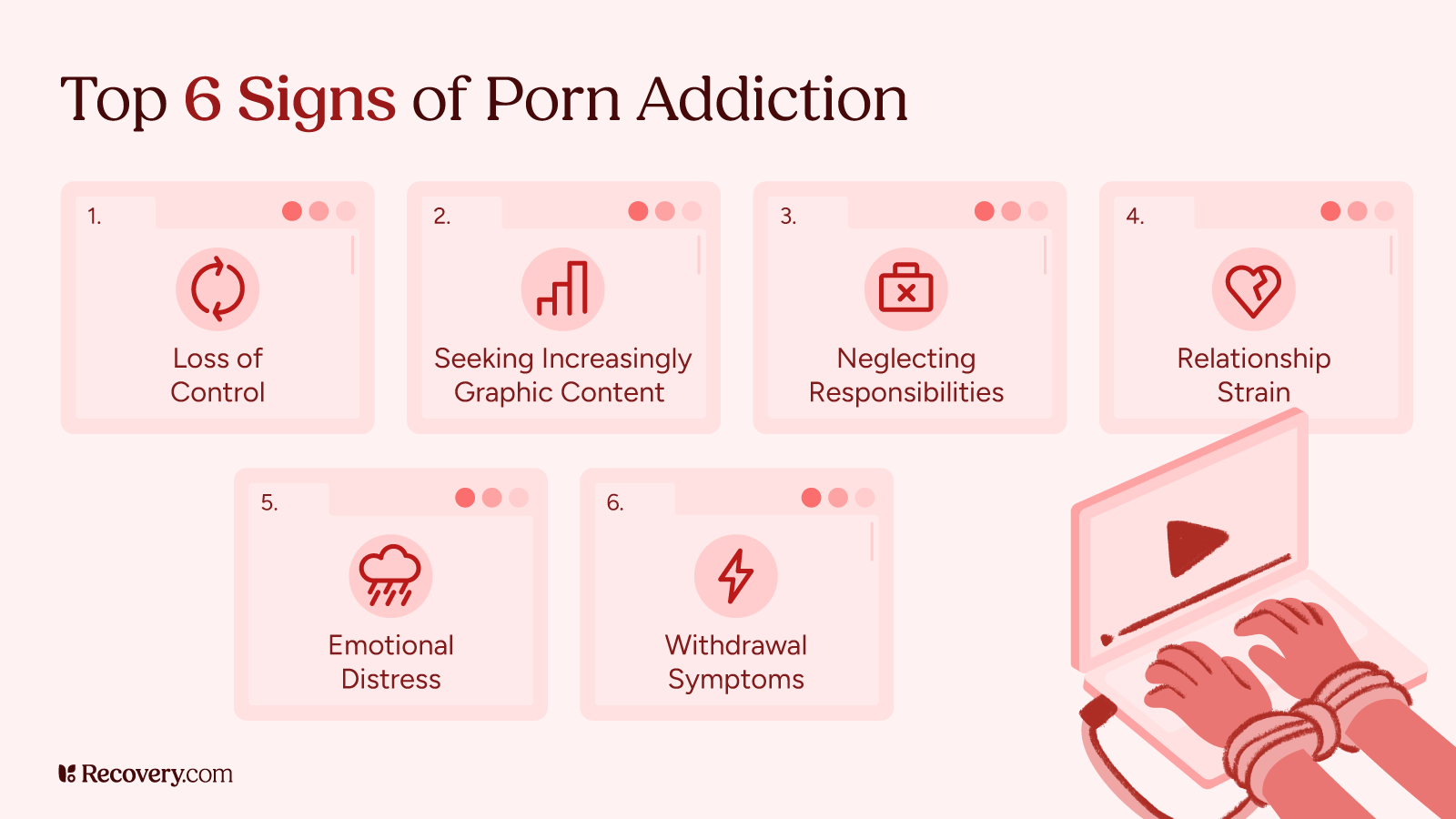
1. You Can’t Stop
One of the most evident signs of porn addiction is the inability to stop viewing pornography despite repeated attempts. This compulsive behavior can interfere with daily life, relationships, and responsibilities. Individuals may experience withdrawal symptoms,1 such as mood swings and cravings, when trying to cut back.
Research suggests that behavioral addictions like pornography addiction2 activate the same reward pathways in the brain as substance addictions, making compulsive use a serious concern.
Recognizing the signs of porn addiction is the first step toward recovery.
How can I tell if I have a porn addiction?
Like other forms of addiction, porn addiction is primarily marked by a loss of control. Here, an individual’s thoughts, behaviors, and emotions ultimately become consumed by pornography to the point where they begin neglecting other priorities and even people. It often leads to a state of distress whereby even when one wants to take pause and distance themselves, they cannot. Interpersonal relationships, especially romantic or sexual ones, become compromised too, as the obsession with pornography takes priority over real-life interactions and can develop to the point where true physical connection is no longer desirable.
Matt Glowiak, PhD, LCPC, CAADC, ACS, NCC | Hazelden Betty Ford Graduate School
2. You Want More
Pornography consumption can lead to tolerance, similar to substance addiction. Over time, an individual may seek out more explicit or extreme pornographic content to achieve the same level of excitement. This escalation can reinforce dependency and increase the risk of sexual dysfunction.
Social media can also promote unrealistic standards of physical attractiveness and sex, making the lure from these sites to pornographic ones a quick one.
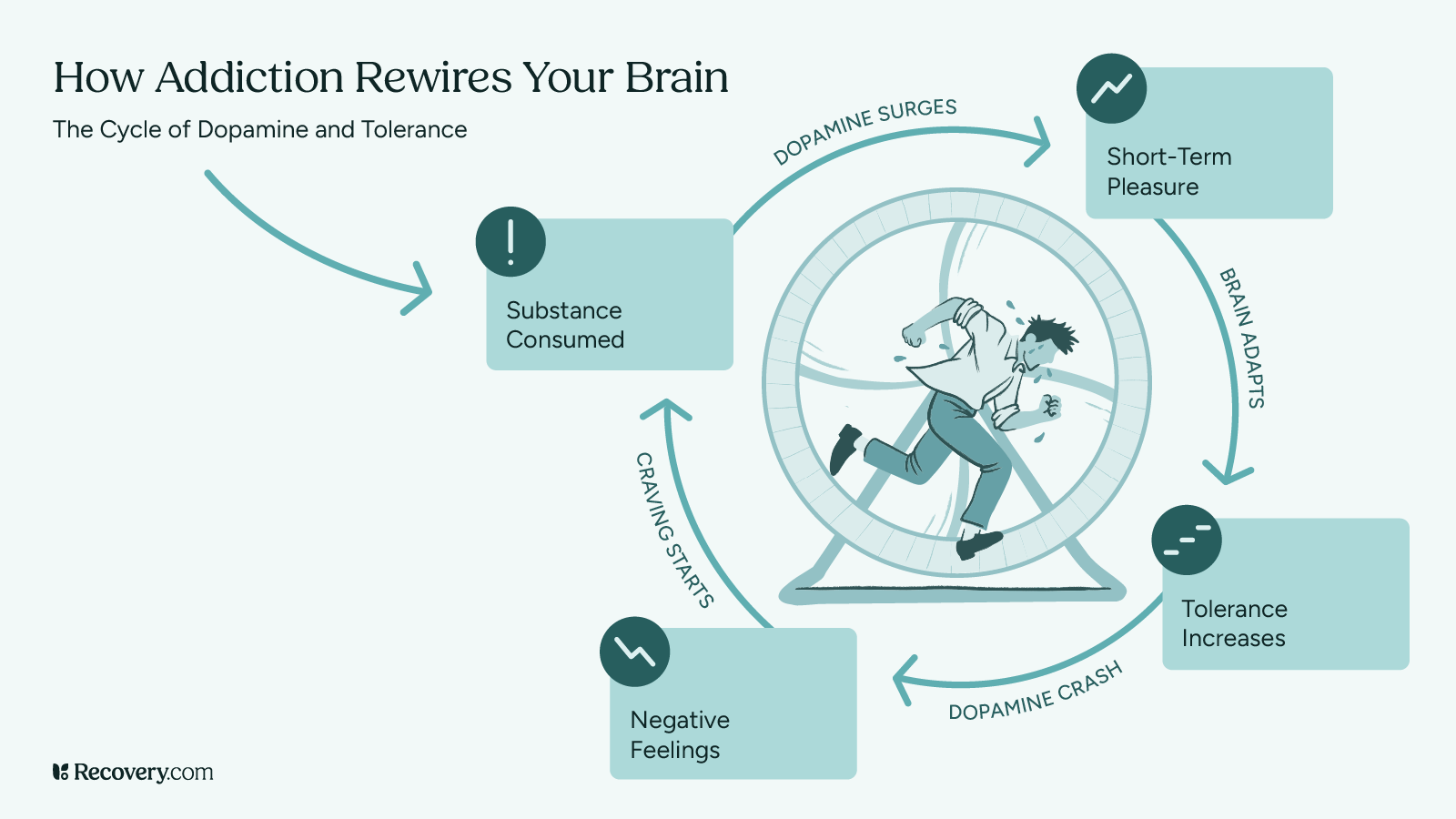
Pornography can create a vicious cycle in the brain, largely due to its impact on dopamine,3 the neurotransmitter responsible for pleasure and motivation.
- When someone watches porn, their brain releases a surge of dopamine, leading to intense feelings of reward. However, overstimulation can cause the brain to downregulate dopamine receptors4—essentially, reducing their sensitivity to dopamine over time.
- As a result, the person may start feeling depleted or less satisfied with the same content, leading them to seek out more stimulating material or spend longer periods watching porn to achieve the same high. This is similar to what happens in substance addiction, where repeated exposure leads to tolerance and an increased need for stronger stimuli.5
3. You’ve Lost Time
Pornography use is on the rise due to a number of factors including “accessibility, affordability, and anonymity.”6 Many individuals report losing track of time, which affects productivity, work performance, and personal relationships. Excessive time spent on porn use can lead to neglecting important daily responsibilities.
- Over time, a pattern of pornography use can make it harder to enjoy everyday pleasures, as the brain becomes wired to seek its dopamine fix through pornography rather than real-life experiences.
- Some studies suggest that excessive porn use may even contribute to issues like desensitization, difficulty in forming relationships, and sexual dysfunction.
- In short, by constantly chasing the dopamine high, some people find themselves caught in an escalating loop—needing more extreme content or longer sessions just to feel the same level of excitement, all while their brain becomes less responsive to natural rewards.
4. You’ve Lost Interest in Sex
Frequent viewing of pornographic material can lead to a decline in real-life sexual relationships. Unrealistic expectations created by pornography consumption may result in reduced attraction to a loved one, leading to intimacy issues and relationship problems.
- The Journal of Sex Research notes that porn websites are more frequently visited7 than any other type of website on the internet and for a longer duration of time.
- The current market value of the porn industry8 is expected to surpass one billion dollars annually and has experienced a 58% growth in the market since 2018. These are overwhelming statistics that highlight the prevalence and availability of porn that competes with real-life sexual relationships.
5. You’re More Demanding
As porn addiction progresses, individuals may develop unrealistic expectations of sexual activities. They may pressure their partner into engaging in behaviors seen in pornographic content, leading to dissatisfaction and strain in romantic relationships.
- Porn use becomes a coping mechanism that creates mental health issues and disrupts and replaces natural sexual behavior. While porn addiction is not officially recognized as a diagnosis in the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition), it does not mean that it does not significantly impact relationships and cause mental health conditions.
- While the DSM-5 doesn’t classify it as an addiction, the World Health Organization’s ICD-11 (International Classification of Diseases) does recognize compulsive sexual behavior disorder (CSBD),9 which can include problematic porn use.
So, while there’s still debate over whether “porn addiction” is the right term, research suggests that compulsive porn use can have real effects on mental health and behavior.
What is the difference between sex addiction and pornography addiction?
Sex and porn addiction both involve compulsive sexual behaviors that manifest differently. Sex addiction typically includes a pattern of seeking out sexual experiences (such as multiple partners, risky encounters, or excessive masturbation) despite negative consequences. Porn addiction, which is a subset of sex addiction, is characterized by compulsive pornography use that interferes with relationships, work, or emotional well-being. Both can stem from deeper emotional or psychological struggles, and addressing them often requires exploring underlying issues, developing healthier coping strategies, and developing meaningful connections.
Andrew J. Schreier, ICS, CSAC, LPC, ICGC-II, BACC
6. You’ve Lost Attraction
Another warning sign of porn addiction is a loss of attraction to a romantic partner. The overstimulation of the brain’s reward system due to frequent viewing of pornography7 can alter real-life perceptions of beauty and desirability, affecting the ability to maintain healthy relationships.
- Sexual health is impacted in a way that influences romantic relationships in real life. Social media can also play a role in disrupting healthy, human relationships. Struggling with porn addiction can also lessen the amount of time spent with partners in romantic relationships.
- Young adults are also impacted by symptoms of porn addiction like mental health disorders and low self-esteem.
7. You’re Losing Money
Some people who struggle with pornography addiction may spend significant amounts of money on subscriptions, premium content, or even engaging in online sexual activities.
This financial strain can impact daily life, leading to stress and potential conflicts with a family member or loved one. Use of pornography can also have a heavy financial burden, with some sites requiring increasing fees for use.
8. You’re Distracted
In today’s digital age, pornography is more accessible than ever, making it easy to develop compulsive behaviors without realizing the impact on mental health, relationships, self-esteem, and daily life.
While many people consume porn casually, for some, it becomes a habit that feels impossible to break. If you’ve ever found yourself struggling to stop, needing increasingly explicit content, or noticing a decline in real-life intimacy or continual distraction, you’re not alone.
Porn addiction can make it difficult to focus on tasks, leading to decreased productivity and performance at work or school. Individuals may frequently think about viewing porn, leading to an inability to concentrate on important responsibilities.
How can pornography addiction get in the way of my everyday life?
Pornography addiction goes beyond casual viewing—it consumes your time and energy affecting your work, relationships, and mental well-being. The constant need for stimulation rewires your brain creating unrealistic expectations and making real-life intimacy feel unfulfilling. Over time, isolation, secrecy, and shame take over, leading to withdrawal from loved ones and neglect of personal growth. True wellness comes from balance, and breaking free from addiction means reclaiming control over your time, relationships, and sense of self.
Rebecca E. Tenzer MAT, LCSW, CCTP, CGCS, CCATP, CCFP, CIMPH | Astute Counseling & Wellness Services
9. You’re Angry
Feelings of guilt, shame, and frustration can contribute to increased irritability and anger in individuals struggling with pornography addiction. Withdrawal symptoms from excessive porn use may lead to mood swings, emotional instability, and relationship problems.
Research suggests that when people become deeply engrossed in internet pornography, their brains react in a way similar to substance addiction8—certain neural pathways light up, triggering a direct and intense response to the content.
- Just like in drug addiction, watching porn releases a surge of dopamine, the brain’s pleasure and reward chemical, reinforcing the habit and making it harder to stop.
- However, over time, dopamine receptors become less responsive, meaning the same content no longer provides the same thrill. This can lead to frustration, irritability, and even anger issues, especially when a person tries to cut back or when real-life experiences don’t match the high of pornography.
Some studies even link compulsive porn use to emotional dysregulation, making individuals more prone to mood swings and impulsivity.
In extreme cases, this cycle of addiction and emotional instability can increase aggression, particularly when someone experiences withdrawal-like symptoms from trying to quit or faces obstacles to accessing porn. This makes it even harder to break free from the cycle, as stress and negative emotions can push them back toward their habitual coping mechanism—watching more porn.
Talking About Porn Addiction
Discussing pornography addiction can be challenging, especially for individuals who experience feelings of guilt or shame. Support groups such as
Sex and Love Addicts Anonymous (S.L.A.A.) can provide a safe space for people to share their struggles and receive guidance from others who have faced similar challenges.
Porn addiction is often linked with other behavioral addictions and substance use disorders, such as alcohol addiction and drug dependency.
Research suggests that behavioral addiction, like pornography addiction, affects the same brain regions10 as substance addiction, reinforcing compulsive behavior.
Seeking Treatment and Recovery
Overcoming pornography addiction requires a combination of self-awareness, support, and professional intervention. Treatment options such as CBT, psychotherapy, and addiction treatment programs can help individuals break free from compulsive pornography use and improve their quality of life.
Recognizing the signs of porn addiction is the first step toward recovery. By seeking help and implementing positive changes, individuals can restore their well-being, maintain healthy relationships, and regain control over their lives.
Porn addiction can feel isolating, but recovery is possible with the right support and strategies. Recognizing the signs of problematic use is the first step toward making meaningful changes. Help and treatment are available.
Overcoming compulsive pornography use isn’t just about quitting—it’s about regaining control, rebuilding healthy relationships, and improving overall well-being.
If you or someone you know is struggling, seeking help is a courageous step toward a healthier and more fulfilling life. Explore porn addiction rehabs now and speak to an admissions specialist today.
FAQs
Q: What is porn addiction?
A: Pornography addiction, also known as problematic pornography use (PPU), is characterized by an individual’s inability to control their consumption of pornographic material, leading to significant distress or impairment in personal, social, or occupational areas of life. This compulsive behavior persists despite negative consequences.
Q: What are 5 warning signs of addiction?
A: Identifying addiction involves recognizing certain behavioral patterns. Five warning signs include:
- Preoccupation: Constantly thinking about engaging in the addictive behavior.
- Loss of Control: Unsuccessful attempts to reduce or stop the behavior.
- Tolerance: Needing increasing amounts of the behavior to achieve the desired effect.
- Withdrawal: Experiencing negative emotions or physical symptoms when unable to engage in the behavior.
- Neglecting Responsibilities: Prioritizing the behavior over important personal or professional obligations.
Q: What does porn addiction do to your brain?
A: Chronic consumption of pornography can lead to neurobiological changes similar to those observed in substance addictions. These changes may include altered brain structure and function, affecting areas related to reward, motivation, and decision-making. Such alterations can reinforce compulsive viewing behaviors and diminish sensitivity to natural rewards.
Q: How to treat pornography addiction?
A: Effective treatment approaches for pornography addiction often involve:
- Psychotherapy: Cognitive Behavioral Therapy (CBT) has been shown to reduce the severity of PPU and associated symptoms like anxiety and depression.
- Support Groups: Participating in peer support groups provides community support and shared coping strategies.
- Medication: In some cases, pharmacotherapy may be considered as part of a comprehensive treatment plan.
A combination of these approaches is often recommended for optimal outcomes.
Q: What causes problematic pornography use?
A: The development of problematic pornography use can be influenced by various factors, including:
- Psychological Factors: Stress, anxiety, and depression are strongly related to increased pornography consumption.
- Behavioral Factors: Habitual use as a coping mechanism for negative emotions or boredom.
- Social Factors: Exposure to environments where pornography use is normalized or encouraged.
Understanding these underlying causes is crucial for effective intervention and treatment.
Q: What is the difference between sex addiction and pornography addiction?
A: While both involve compulsive sexual behaviors, they differ in focus:
- Sex Addiction: Encompasses a broad range of compulsive sexual activities, including promiscuity, excessive masturbation, and risky sexual behaviors.
- Pornography Addiction: Specifically relates to the compulsive consumption of pornographic material, often leading to isolation and neglect of real-life relationships.
Both conditions can co-occur and may require similar therapeutic approaches.
Q: How can pornography addiction affect your mental health?
A: Problematic pornography use is associated with various mental health challenges, including:
- Increased Anxiety and Depression: Excessive use can exacerbate feelings of anxiety and depression.
- Cognitive Distortions: Developing unrealistic expectations about sex and relationships.
- Emotional Distress: Feelings of guilt, shame, or hopelessness related to one’s behavior.
Addressing these mental health issues is a critical component of comprehensive treatment.
Q: How can I tell if I have a pornography addiction?
A: Self-assessment questions to consider:
- Frequency: Do you spend a significant portion of your time engaging with pornography?
- Control: Have you tried to cut back without success?
How Do I Stop Being Codependent? 5 Expert-Backed Steps to Transform Your Relationships
Do you find yourself constantly putting others’ needs before your own? Are you the person everyone relies on, even when it drains your energy and emotional resources? You might be experiencing codependency—a pattern where your own sense of purpose and self-worth become tangled up in another person’s life and problems
Codependent relationships create strong emotional patterns. “Helping” people can become almost addictive, even though it leaves you feeling empty and exhausted in the long run. Breaking free from these patterns takes time. But with consistent effort, you can build a healthier relationship with yourself and others.
Here are 5 key steps you can start taking now:
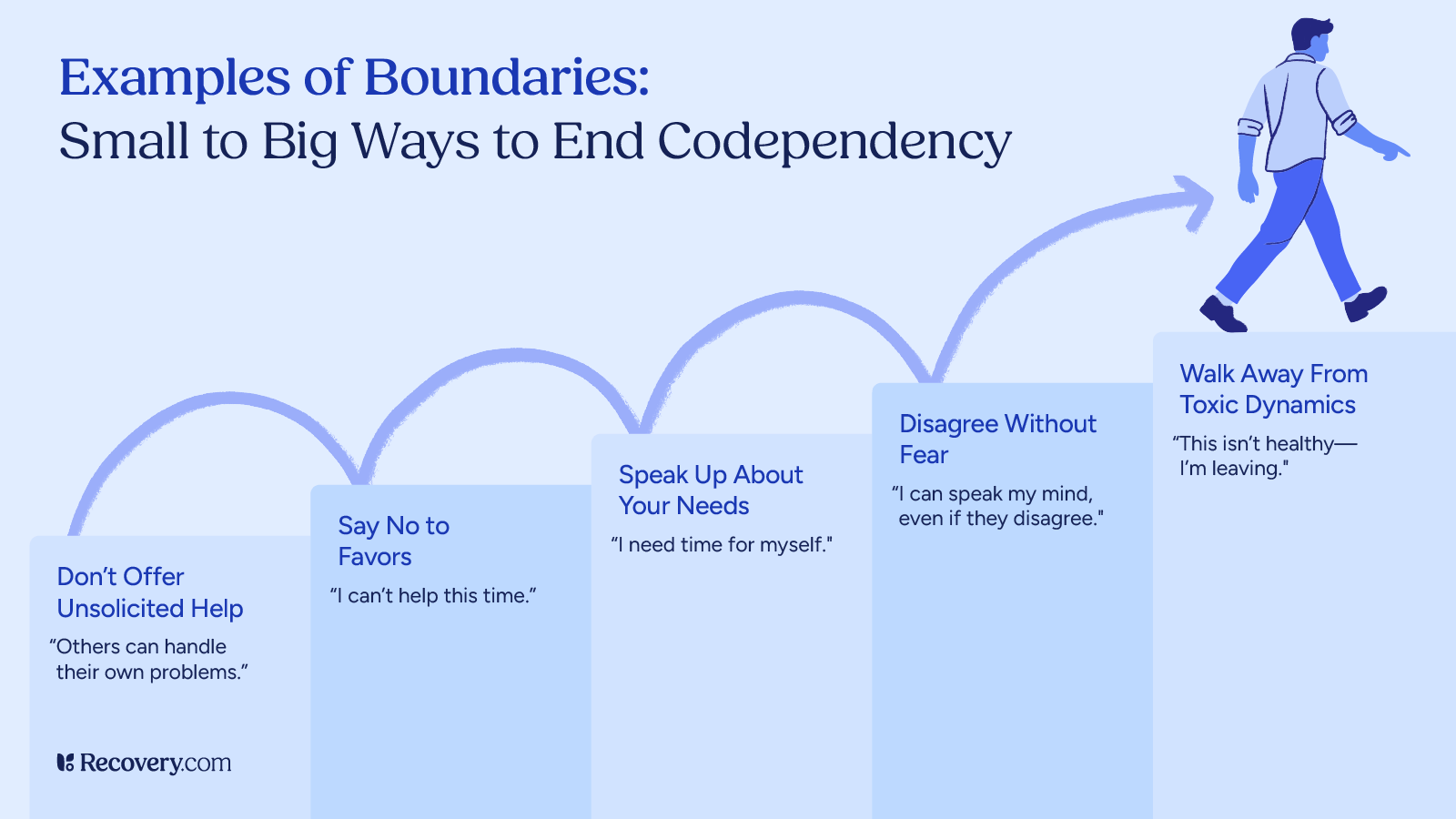
1. Recognize Your Codependent Patterns
The first step toward change is becoming aware of your codependent behaviors.1 Start paying attention to situations where you feel responsible for others’ emotions or problems. Notice when you automatically put someone else’s needs before your own or when you feel anxious about setting boundaries.
Try keeping a journal to track moments when you feel resentful, exhausted, or unappreciated. Look for the situations or relationships that typically trigger these feelings. You can ask yourself questions like: “Am I doing this because I want to, or because I’m afraid of the consequences if I don’t?” You can even use journal prompts for codependency to help.
Pro tip: Keep in mind that awareness doesn’t mean judgment. These patterns developed for a reason—often as ways to cope with difficult situations. Observing them with curiosity rather than criticism will help you make lasting changes.

What Is Codependency?
Codependency is not officially recognized as a mental illness, but it is taken seriously by mental health professionals, who define it as “an unhealthy devotion to a relationship2 at the cost of one’s personal and psychological needs.” It describes a relational pattern where you become so focused on the problems and needs of others that you neglect your own well-being. It’s more than just caring deeply—it’s when your emotional state, identity, and sense of purpose become excessively wrapped up in someone else’s life.
- Codependency in Romantic Relationships: In romantic relationships, codependency can look like constantly sacrificing your own preferences, walking on eggshells to avoid conflict, or feeling responsible for your partner’s happiness. You might stay in unhealthy situations because you believe your love can “fix” the other person.
- Codependency in Family Systems: Within families, codependency often appears as enmeshment—where boundaries between family members become blurred. You might feel obligated to solve everyone’s problems, shield relatives from consequences, or struggle to make decisions without family approval. This is often the case when one family member is struggling with substance abuse.3
- Codependency in Friendships: In friendships, codependent behaviors include being the perpetual advice-giver or emotional support while rarely asking for help yourself. You might maintain one-sided friendships because you feel needed, even when these relationships drain you.
How can you discover the signs of being codependent?
Codependency is often rooted in an attachment wound where the nervous system learned early on that safety comes from attuning to others, sometimes at the expense of self. It can look like feeling responsible for managing other people’s emotions while ignoring your own. Another sign is the feeling of unease or even panic when someone is upset with you, leading to people-pleasing or over-functioning in relationships. This can present as feeling tightness in your chest, a constant state of hypervigilance, or struggling to feel grounded in your own body.
Amanda Stretcher, MA, LPC-S | Crescent Counseling
2. Work on Building Self-Esteem
Codependency and low self-esteem usually go hand in hand. When you don’t value yourself, you might look for validation through helping others or staying in unhealthy relationships.
You feel good about yourself mainly when you’re helping others or when people need you. Instead of feeling relieved when a loved one says they don’t need your help, you feel hurt or like you don’t matter anymore.
Start building your self-worth by practicing self-compassion.4 Talk to yourself the way you would talk to a good friend—with kindness and understanding. Make a list of your positive qualities that have nothing to do with what you do for others.
Small acts of self-care also build self-esteem. When you treat yourself with respect—by keeping promises to yourself, taking time for activities you enjoy, or meeting your physical needs—you send yourself the message that you matter.
Pro tip: Daily affirmations can help you shift away from negative self-talk and toward a more positive sense of self. Simple statements like “I’m worthy of love and respect” or “My needs matter” can start to shift your perspective when you say them regularly.
Why is boundary setting important in healing from codependency?
When it comes to codependency, one tends to slip away from autonomy, creating enmeshment with the enabler. Setting healthy boundaries, such as adopting and maintaining one’s own intellectual boundaries in a new relationship, is crucial for healing codependency. While maintaining codependency, and therefore not setting boundaries, one loses one’s own identity and essentially forgets how to behave independently due to the behavioral and emotional habits developed through the codependent relationship. Setting boundaries will contribute to an increased sense of self, more confidence, and may even decrease anxiety or depressive symptoms, which can significantly enhance the relationship as a whole.
Jennifer Chicoine, MA, LCPC, CCTP | Peaceful Healing Counseling Services
3. Set and Enforce Healthy Boundaries
Boundaries allow you to create rules or set limits that define where your responsibilities end and another person’s begin. They protect your emotional well-being while allowing you to support others in healthy ways.
Setting boundaries can be uncomfortable at first, especially when you’re not used to it. As you do so, keep in mind that boundaries are for you,5 says boundary expert Nedra Glover Tawwab, LCSW:
Changing your behavior and not forcing others to change can be a significant part of setting boundaries…It would be nice if everyone automatically knew how to respect our boundaries. We often have to communicate them clearly and enforce consequences when they are not respected. So, when someone crosses one of my boundaries, I will take action to protect myself and my needs.
Be clear and direct when communicating boundaries. Use “I” statements that focus on your needs rather than accusing the other person. For example, “I need some alone time to recharge” works better than “You’re demanding too much of my time.”
Prepare yourself for pushback. Some people in your life may resist your new boundaries because they benefit from your codependent behaviors. Remember that their reaction isn’t your responsibility, and temporary discomfort is part of creating lasting change.
Consistency is key. When you set a boundary, follow through with it. Each time you maintain a healthy boundary, even when it’s difficult, you’re building new patterns that will eventually replace codependent ones.
4. Learn to Prioritize Your Needs
For many people with codependent tendencies, identifying their own needs can feel foreign. Get in the habit of asking yourself: “What do I want right now?” or “What would feel good to me in this situation?”
Practice making decisions based on your preferences. Start with small choices like what to eat for lunch or what movie to watch, then work up to bigger decisions.
Prepare phrases for when you need to put yourself first. Simple statements like “I need to take care of myself right now” or “I’ll need to check my schedule before committing” give you space to consider your own needs.
Pro tip: Remember that prioritizing your needs isn’t selfish—it’s necessary for your well-being and actually leads to healthier relationships. When you’re not depleted from ignoring your own needs, you have more genuine energy to share with others.
Codependency vs. Interdependence
Unlike healthy independence—where 2 people mutually rely on each other while maintaining individual identities—codependency creates an imbalance. Healthy relationships involve give-and-take, with both people supporting each other while respecting boundaries. Both parties feel free to express needs, disagree respectfully, and maintain outside interests and relationships.
The key distinction here is that interdependence strengthens both individuals, while codependency tends to diminish at least one person’s wellness and autonomy over time.
Does your partner or loved one exhibit signs of being codependent?
“Loving someone who is codependent can feel like an emotional roller coaster, but it’s important to remember—you can’t fix them. Their actions often come from a place of love, but they struggle to put themselves first. The best thing you can do is communicate your needs clearly, set firm yet compassionate boundaries, and encourage them to cultivate their own interests. By modeling self-care, independence, and balance, you show them what a healthy, fulfilling relationship looks like.”
Rebecca Tenzer, MAT, LCSW, CCTP, CGCS, CCATP, CCFP, CIMPH | Astute Counseling & Wellness Services
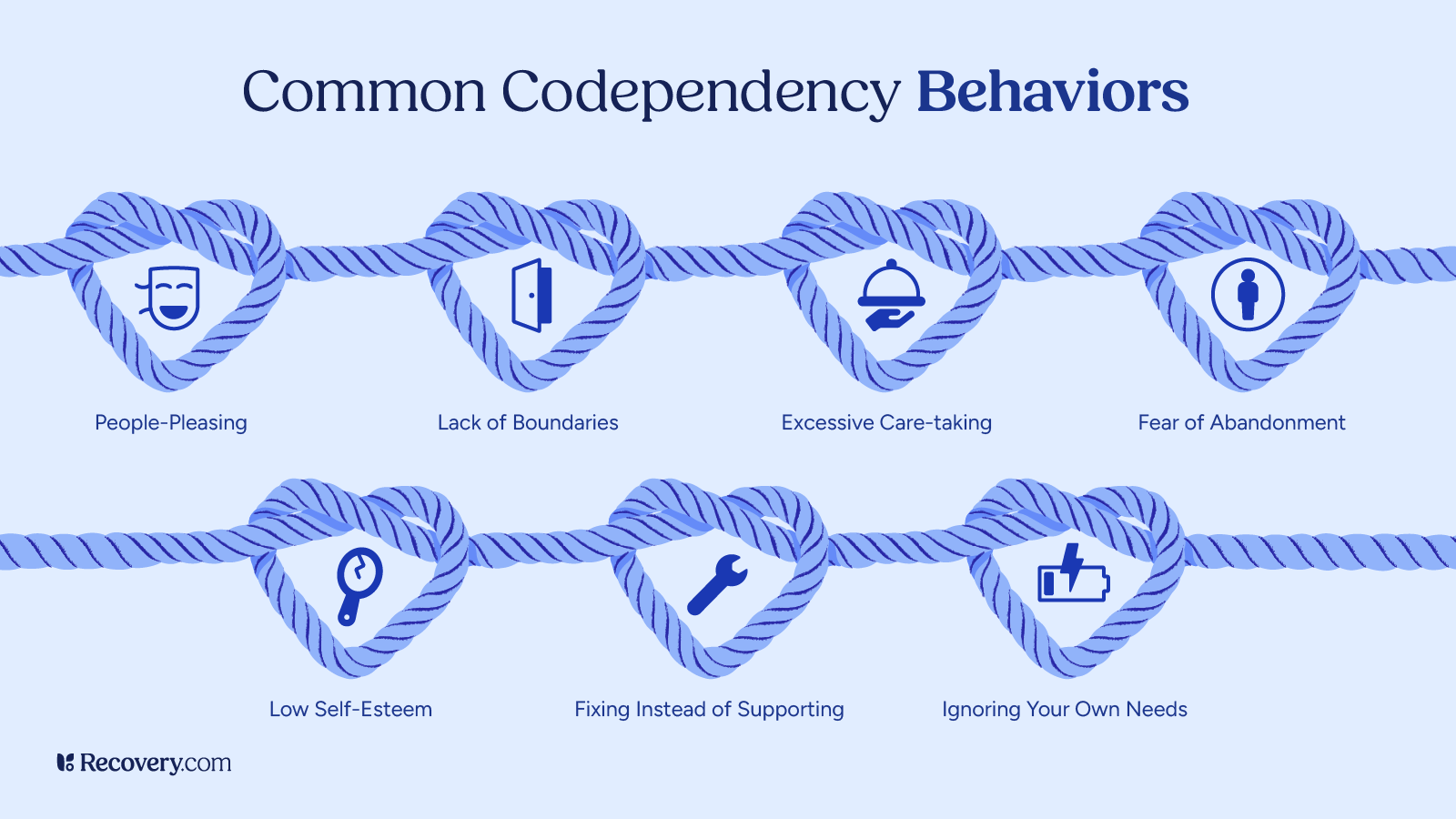
Signs of Codependency
Spotting codependent patterns6 in your life is the first big step toward making real change. Everyone’s experience with codependency looks a bit different, but here are some common signs you might recognize in yourself:
- Excessive caretaking: You almost always put other people’s needs ahead of your own, even when it hurts you. For example, you might stay up all night helping a friend with their project even though you have an important meeting tomorrow, cook fancy meals for your family while you just eat whatever’s left over, or say “yes” to additional tasks when you already feel overburdened.
- Difficulty setting boundaries: You find it really hard to say “no” when people ask you for favors or your time. You may cancel plans you were looking forward to because a coworker asked for help at the last minute, or you let family members call you during your workday for things that aren’t emergencies.
- People-pleasing tendencies: You make decisions based on what will make others happy, not what’s best for you. You might agree with someone’s opinion even when you actually think differently, just to avoid any conflict. Or you might take on extra tasks because you’re scared of letting someone down.
- Fear of abandonment: A codependent person will often work extra hard to keep relationships going because they’re scared people will leave them. This could mean putting up with someone treating you badly or staying in relationships that don’t make you happy because the idea of being alone feels too scary to face.
- Controlling behaviors: In an attempt to be helpful, you try to control situations or people out of anxiety. This can look like constantly offering unsolicited advice or getting frustrated when someone doesn’t follow your suggestions about how to handle their problems.
- Difficulty identifying your own feelings: You’re tuned into others’ emotions but disconnected from your own. You might be able to sense when your partner is upset before they even realize it but struggle to answer when someone asks how you’re feeling.
- Unhealthy attachment to drama or crisis: You feel most purposeful when solving problems and might even unconsciously create or seek out chaotic situations where you can play the rescuer. When times are crisis-free, you may feel anxious, uncertain, or uncomfortable.
5. Seek Support and Professional Help
Overcoming codependency is challenging work, and you don’t have to do it alone. Professional support can make a huge difference in your healing journey.
Therapy, especially with someone who specializes in codependency, family systems, or trauma, can help you understand the roots of your codependent patterns and develop strategies to change them. Cognitive-behavioral therapy (CBT) and dialectical behavior therapy (DBT) are particularly effective approaches for addressing codependency.
Support groups like Codependents Anonymous (CoDA)6 offer connection with others facing similar challenges. Spending time around others who share your experiences can reduce shame and provide insights for your recovery.
Self-help books about codependency, boundaries, and self-esteem can supplement other forms of support. Look for resources by recognized mental health professionals that offer practical exercises alongside information.
Pro tip: Codependent No More2 and its accompanying workbook by codependency expert Melody Beattie are classics on the topic, and a great place to start. There are also treatment resources available.
Life Beyond Codependency: Your Journey to Emotional Freedom
Breaking free from codependent patterns opens the door to relationships where you can truly be yourself. Working with a professional can accelerate your progress, giving you tools that fit your specific situation and background. Whether you choose one-on-one therapy or a structured program, having expert support gives you the guidance and follow-through that helps make real, lasting change possible.
FAQs
Q: Is it possible to stop being codependent?
A: Yes, codependency is a learned behavior that can be unlearned with self-awareness, therapy, and personal growth. According to Mental Health America, addressing underlying self-esteem issues, setting boundaries, and seeking support are key steps toward breaking free from codependency.
Q: How do you break the codependency cycle?
A: Breaking the cycle of codependency involves recognizing unhealthy relationship patterns, developing self-worth, and learning to set and maintain boundaries. Codependents Anonymous recommends a 12-step recovery process, while therapy and support groups can also be helpful in fostering independence and healthier relationships.
Q: What triggers codependency?
A: Codependency often stems from childhood experiences, such as growing up in an environment where emotional needs were not met or where a caregiver had addiction or mental health struggles. Other triggers include fear of abandonment, low self-esteem, and seeking validation through others.
Q: How do you heal codependent tendencies?
A: Healing from codependency involves building self-esteem, practicing self-care, and learning healthy communication. The National Center for Biotechnology Information suggests cognitive behavioral interventions can help individuals develop healthier thought patterns and coping strategies.
Q: How do you prevent a codependent relationship?
A: Preventing codependency starts with self-awareness and setting clear boundaries. Maintaining individual interests, fostering self-worth, and communicating openly with partners or loved ones can help establish interdependent, rather than codependent, relationships.
Q: How does a codependent person feel?
A: A codependent person may feel anxious, responsible for others’ happiness, or emotionally drained. They often struggle with low self-esteem and fear abandonment, leading them to prioritize others’ needs over their own.
Q: Does your partner or loved one exhibit any signs of being codependent?
A: Signs of codependency in a loved one may include excessive caretaking, difficulty setting boundaries, fear of being alone, and reliance on others for self-worth. Mental Health America highlights that codependency can occur in romantic relationships, friendships, or family dynamics.
Q: Why did I develop codependent tendencies?
A: Codependent tendencies often develop from early childhood experiences, such as growing up in a family where emotional neglect, addiction, or controlling behaviors were present. Research indicates that past trauma and adverse childhood experiences significantly contribute to codependency.
Q: How do you overcome codependency?
A: Overcoming codependency requires self-awareness, boundary-setting, and shifting focus to personal well-being. Therapy, support groups, and mindfulness practices have been found to be effective in fostering emotional independence.
Q: What are narcissistic traits?
A: Narcissistic traits include a lack of empathy, an inflated sense of self-importance, manipulation, and a need for excessive admiration. Codependents often find themselves in relationships with narcissistic individuals due to their caretaking tendencies.
Q: What steps can I take to stop being codependent?
A: Steps to stop being codependent include recognizing unhealthy patterns, building self-esteem, practicing self-care, and seeking therapy or support groups. Developing hobbies and interests outside of relationships can also help foster independence.
Q: What are effective strategies to stop being codependent?
A: Effective strategies include therapy (such as cognitive-behavioral therapy), practicing mindfulness, learning assertiveness skills, and setting firm boundaries. Research suggests that increasing self-awareness and engaging in self-affirmation exercises can aid in breaking codependent habits.
Rewiring Your Brain From Addiction: 7 Things You Need To Know
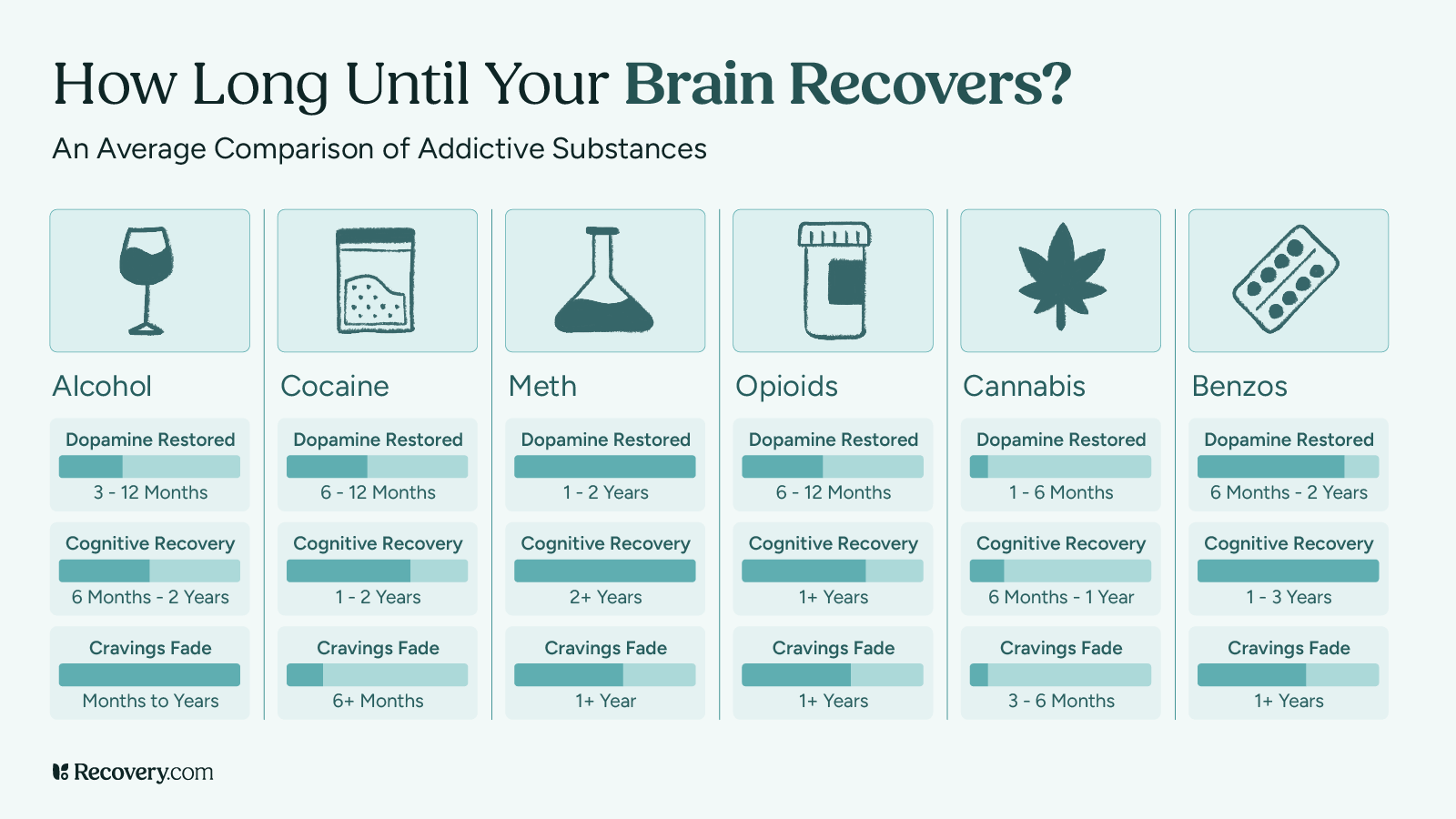
When you stop using drugs and alcohol, it takes time to rewire your brain. The exact timeframe depends on several factors. Certain drugs, for example, lengthen the brain rewiring process. Some practices can also help you recover faster.
Here’s what experts know about helping your brain rebuild after addiction:
1. Understanding How Addiction Changes Your Brain
Dopamine and the Brain’s Reward System
Your brain has a natural reward system1 that makes you feel good when you do things that help you survive and thrive. This system uses a neurotransmitter called dopamine, which creates feelings of pleasure and happiness. When you eat good food, exercise, or spend time with people you love, your brain releases small amounts of dopamine.
Alcohol and drug use release far more brain chemicals2 than natural activities do. This creates an unnaturally strong surge of pleasure signals in your brain. When this happens repeatedly, it can overwhelm your brain’s normal reward system.
Over time, your brain tries to adjust to these high levels of dopamine by becoming less sensitive to it. This means you need more and more of the substance to feel the same effects: a process we call tolerance.3 Regular stimuli that used to make you happy might not feel as good anymore, because your brain’s reward system isn’t working like it should.
Areas of the Brain Affected by Addiction
Addiction affects 3 main parts of your brain.4 Each plays a crucial role in helping you think, feel, and make decisions.
The basal ganglia is your brain’s pleasure center. It helps you feel good when you do healthy things like eating or exercising. With substance use disorders, this area becomes less sensitive to normal pleasures and more focused on substances.
The amygdala is your brain’s stress manager. When addiction develops, this area becomes more sensitive. This can make you feel anxious, irritable, or uncomfortable when you’re not using addictive substances.
The prefrontal cortex5 helps you make good decisions and control impulses. Addictive behaviors make this area weaker, which makes it harder to resist cravings or think about long-term consequences.
Rewiring your brain from addiction is real, and it works. Research suggests meaningful neural shifts can happen in weeks, but full recovery takes months or years of consistent effort involving identifying and replacing toxic thought patterns, creating new neural pathways, and reinforcing them with repetition, consistency, and community.
– W. Lee Warren, M.D. | Brain Surgeon and Author
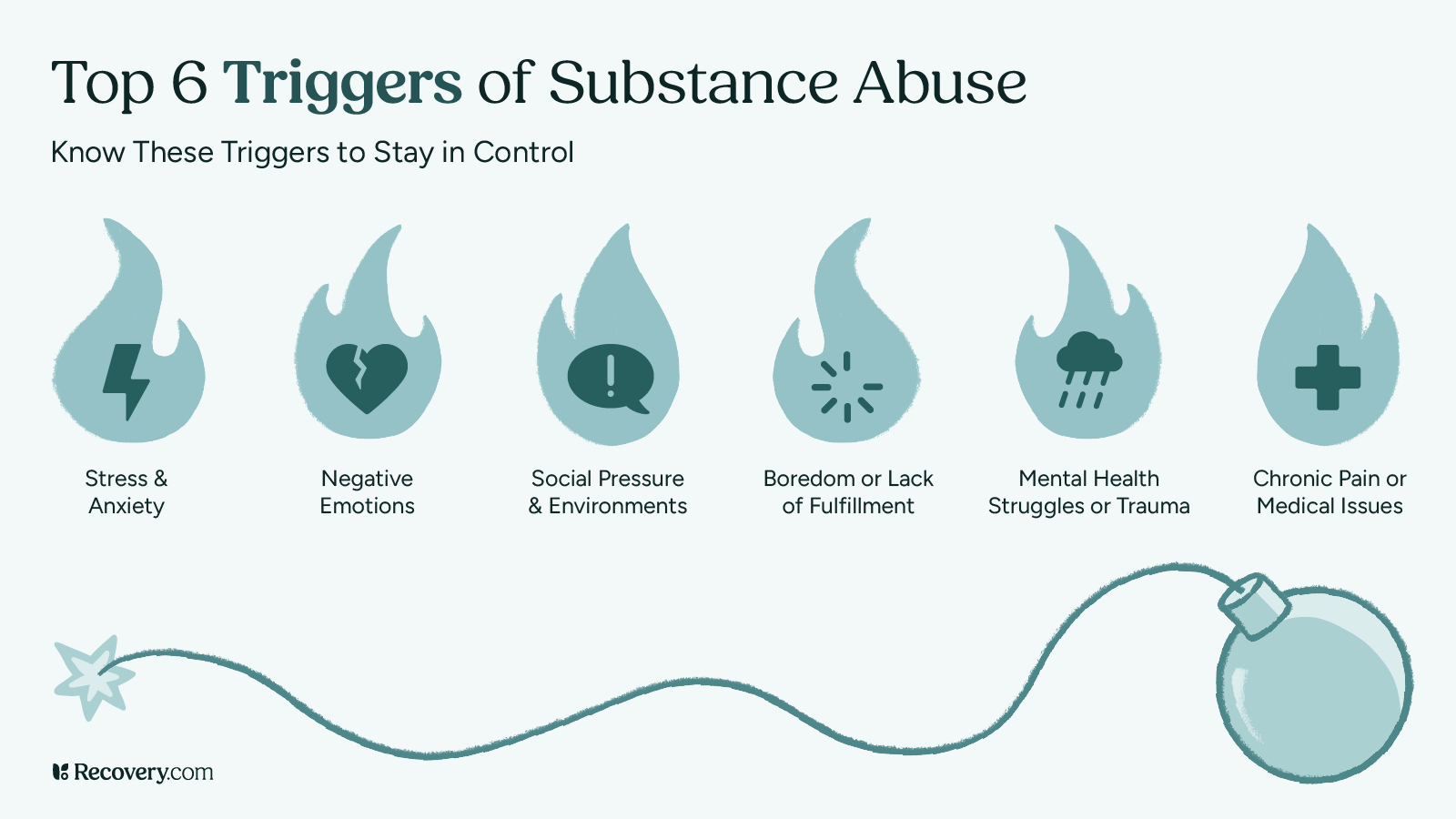
How Habits and Triggers Form
Your brain is designed to help you repeat behaviors that make you feel good. During addiction, your brain creates strong connections between certain situations (called triggers) and substance abuse. These connections form through repeated use over time.
Triggers can be places, people, feelings, or times of day that your brain associates with drug abuse. When you encounter these triggers, your brain automatically generates cravings. Learning to understand and manage your triggers (and their associated coping mechanisms) is an important part of recovery.
2. The Timeline of Brain Recovery
The recovery process happens in stages, and everyone’s path is different. While your brain health starts to improve as soon as you stop using substances, the full process takes time. Knowing what to expect during each stage can help you see the progress you’re making, which helps you stay motivated.
What to Expect in the First Month
The first month of recovery usually involves the biggest changes as your body adjusts to being substance-free. During the first week, you might experience withdrawal symptoms as your brain chemistry starts to reset. These symptoms can be uncomfortable, but they usually peak within a few days.
After the first week, many people notice their thinking becomes clearer and their sleep starts to improve. You might have mood swings or strong cravings during this time, which is normal. Your brain is working hard to restore its natural chemical balance.
Some people also notice changes in their appetite and energy levels during this first month. These changes are signs that your brain and body are beginning to heal.
Changes During Months 2-12
During these months, your brain continues to heal and rebuild healthy pathways. A lot of people in this stage find their mood becomes more stable and they start enjoying regular activities again. Your sleep quality and energy levels will continue to improve during this time.
Your brain’s ability to think clearly and make decisions also typically gets better during these months. But you might still experience occasional cravings—especially during stressful times. If this is the case for you, you’re not doing anything wrong! It’s totally normal and tends to happen less often as time goes on.
Your dopamine reward system will gradually become more responsive to natural pleasures like food, exercise, and social connections. This is a great sign that your brain is returning to its normal way of functioning.
Long-Term Recovery: One Year and Beyond
After a year, many people find their brain function has significantly improved. While some people still experience occasional cravings, these are usually less frequent and easier to manage. Your brain continues to heal and strengthen new, healthy patterns throughout your recovery journey.
Factors That Affect Your Recovery Timeline
Several things can influence how quickly your brain heals. These include the type of substances used, how long you used them, your overall health, and whether you have other mental health conditions. Having good support and treatment can help speed up the healing process.
When someone actively works to rewire their brain in recovery, they experience several key benefits: regaining self control, restoring emotional balance, breaking destructive patterns, improved stress response , enhanced cognitive function and a greater sense of purpose and joy. Rewiring the brain in recovery isn’t just about breaking free from addiction—it’s about reclaiming your life, restoring your mind, and creating a future built on strength and resilience.
– Dr. Zoe Shaw | Psychotherapist and Author
3. Stages of Brain Rewiring
Just like healing from a physical injury, your brain goes through different stages as it recovers from drug addiction. While everyone’s journey is unique, knowing what to expect at each stage can help you feel more confident about the path ahead. Let’s look at how your brain heals over time.
Stage 1: Getting Through Withdrawal
The first stage of recovery starts when you stop using substances, and it’s often the most challenging part of the journey. During this time, your brain works hard to adjust to life without substances. You might feel physically and emotionally uncomfortable, which is completely normal.
Most people experience withdrawal symptoms for about a week, though this can vary depending on the substance. It’s very important to get medical support during this time, as some types of withdrawal can be dangerous. Remember, these difficult feelings are temporary and are signs that your brain is beginning to heal.
Stage 2: Early Recovery Changes
After withdrawal, you’ll enter a period where your brain is actively rebuilding healthy patterns. While you might still have cravings, they’ll likely feel less intense than before. This is the perfect time to start learning new ways to handle stress and challenging emotions.
During this stage, many people find it helpful to work with counselors or join support groups. These supports can teach you practical tools for managing cravings and building a healthy lifestyle. Your brain is becoming more receptive to new experiences and ways of coping.
Stage 3: Long-Term Healing
As you move into long-term recovery, your brain continues to strengthen its healthy pathways. While the journey doesn’t end here, many people find that cravings become less frequent and easier to handle. Each day of recovery helps your brain build and maintain these positive changes.
4. Supporting Your Brain’s Recovery
Fortunately, there are plenty of ways you can support your brain’s natural healing process. Think of recovery like tending a garden: The more care and attention you give it, the better it grows. Simple daily choices can make a big difference in how quickly and effectively your brain recovers.
Regular Exercise and Physical Activity
Moving your body is one of the best gifts you can give your healing brain. Exercise naturally boosts your mood6 by releasing feel-good chemicals, similar to the ones your brain is learning to produce again on its own. Even a 15-minute walk can help!
You don’t need to live at the gym or start running marathons. Start with activities you enjoy, whether that’s dancing, swimming, or taking an easy walk around your neighborhood. As your energy improves, you’ll gradually be able to do more.
Sleep and Nutrition
Your brain does much of its repair work while you sleep, making good rest essential for recovery. Try to go to bed and wake up at the same time each day, even if you don’t feel tired at first. Your sleep patterns will naturally improve over time.
Eating nutritious foods gives your brain the building blocks it needs to heal. Instead of worrying about perfect eating habits, focus on adding healthy foods like fruits, vegetables, and proteins to your meals. Even small improvements in your diet can help your brain recover.
Stress Management
Finding healthy ways to handle stress is essential to your recovery journey. Deep breathing, taking short walks, listening to music, or talking with supportive friends all help calm your mind. Remember that it’s okay to start small—working in small moments of relaxation throughout your day can go a long way in calming your nervous system.
Building New Routines
Creating new daily routines helps your brain build healthy patterns. Start with one or 2 simple habits, like having breakfast at the same time every day or taking a walk after dinner. As these become comfortable, you can gradually add more supportive activities to your day.
5. Treatment Options That Help Rewire the Brain
Recovery isn’t a journey you need to take alone—there’s no shame in asking for help. Professional addiction treatment and support can have a huge impact on how quickly your brain heals. These interventions are like tools in your recovery toolkit: you can choose the ones that work best for you.
Therapy and Counseling
Working with a counselor or therapist gives you empowering tools for addiction recovery. These professionals understand how addiction affects the brain and can teach you practical ways to handle cravings and stress. Many people find cognitive behavioral therapy (CBT)7 especially helpful, as it teaches you how to change thought patterns that lead to substance abuse.
Your therapist can act as a guide on your recovery journey, helping you understand your triggers and develop strategies that work for your specific situation. It’s a great idea to find a therapist you like and start building a relationship with them, so help is there when you need it.
Support Groups
Meeting others who understand what you’re going through can be incredibly motivating. Support groups are safe spaces to share your experiences, learn from others, and build connections with people who support your recovery goals.
Lifestyle Changes
Small changes in your daily life can support your brain’s healing process. Focus on one change at a time, like improving your sleep schedule or adding healthy activities you enjoy.
When you rewire your brain, you stop being a passive passenger in your own life and start taking control. Old, destructive circuits weaken, and new, healthier ones take over. This means fewer cravings, better decision-making, and a stronger sense of purpose. It’s not just about avoiding addiction—it’s about building a brain that works for you, not against you. The result? A life where you’re free to think clearly, choose wisely, and move forward with confidence and hope.
– W. Lee Warren, M.D. | Brain Surgeon and Author
6. The Science of Hope and Healing
Understanding Brain Plasticity
Your brain has the ability to change and heal throughout your life. Scientists call this “plasticity,” which means your brain can create new neural pathways as it adapts to changes. This incredible ability is what makes recovery possible, no matter how long you’ve struggled with addiction.
Evidence of Recovery
Brain scanning studies show that people’s brains do heal during addiction recovery.8 While everyone’s timeline is different, many people see improvements in their cognitive functions, including memory, impulse control, decision-making, and emotional regulation. These positive changes only continue as you move forward in your recovery.
Setting Realistic Expectations
Recovery is more like a marathon than a sprint, and that’s okay. Some days will be easier than others, and healing happens gradually. Being patient with yourself and celebrating small victories along the way can help you stay on track.
7. Getting Help and Support
Finding Treatment
Taking the first step toward addiction treatment takes some courage, but the rewards of a life in recovery are well worth it. There are plenty of different treatment programs available to meet your specific needs, from detox to outpatient treatment to residential care. To learn more about choosing the right program, see our guide to finding a treatment center.
Building a Support System
Recovery is stronger when you have people in your corner. Loved ones, family, friends, counselors, support groups, and others in recovery can all be part of your support network. Don’t be afraid to let people know what you need.
If you’re ready to start recovery, a comprehensive rehab program can be a great starting point for your journey. This immersive experience gives you a chance to focus entirely on healing in a substance-free environment. Search for an addiction treatment center that matches your criteria and reach out to their team directly today.
FAQ
Q: How long does it take to rewire your brain from addiction?
A: The brain’s rewiring process varies by individual, but significant changes often occur within 12 to 18 months. Early improvements can be seen within weeks, while full recovery may take years, depending on factors such as substance type, duration of use, and lifestyle changes.
Q: Can dopamine levels return to normal after addiction?
A: Yes, dopamine levels can return to normal over time. The brain gradually restores its natural dopamine balance through healthy activities like exercise, proper nutrition, and stress management. However, this process can take several months to years.
Q: How long does it take to rewire your brain from a bad habit?
A: Breaking and rewiring a habit can take anywhere from 21 days to several months, depending on the habit’s intensity and duration. Consistently practicing new behaviors and avoiding triggers helps establish long-term changes.
Q: Can brains recover from addiction?
A: Yes, the brain has the ability to heal itself through neuroplasticity. While addiction alters brain structure and function, recovery is possible with time, therapy, and healthy habits that support brain repair.
Q: How long does recovery from addiction take?
A: Recovery is an ongoing process that unfolds in stages. While withdrawal symptoms may last days to weeks, brain healing continues for months or even years. Long-term recovery depends on individual factors and continued support.
Q: How long does it take to rewire the brain from addiction?
A: The timeline varies, but research suggests that noticeable improvements occur within 3 to 12 months, with continued healing over several years. Factors like substance type, overall health, and treatment interventions influence recovery speed.
Q: What are the benefits of rewiring the brain from addiction?
A: Rewiring the brain from addiction improves mental clarity, emotional stability, impulse control, and overall well-being. It also restores natural pleasure responses, strengthens decision-making skills, and enhances quality of life.
Q: What are the benefits of brain rewiring?
A: Brain rewiring helps create healthier thought patterns, reduces cravings, improves emotional regulation, and supports better decision-making. It also aids in forming positive habits and strengthening coping mechanisms.
Q: What is brain rewiring in addiction recovery?
A: Brain rewiring in addiction recovery refers to the process of forming new neural pathways to replace substance-related behaviors with healthier alternatives. This involves breaking old habits, reducing cravings, and restoring normal brain function.
Q: How can you increase dopamine in your brain?
A: You can naturally increase dopamine through regular exercise, a healthy diet rich in protein and antioxidants, sufficient sleep, mindfulness practices, social interactions, and engaging in enjoyable activities.
Q: Are there any ways to speed up this process or aid in the brain’s recovery from addiction?
A: Yes, brain recovery can be supported through consistent sleep, regular exercise, balanced nutrition, therapy, mindfulness, and positive social connections. Professional treatment, such as cognitive behavioral therapy (CBT), can also accelerate healing.
Q: What is the timeline for brain recovery from addiction?
A: Brain recovery follows a general timeline:
- First month: Initial withdrawal symptoms, mood swings, and sleep disturbances.
- Months 2-12: Improved cognitive function, emotional stability, and reduced cravings.
- One year and beyond: Strengthened neural pathways, increased natural pleasure responses, and long-term behavioral changes.
Q: What factors influence the time it takes to rewire the brain from addiction?
A: Several factors impact the brain’s recovery timeline, including the substance used, length of addiction, overall health, mental health conditions, treatment interventions, and the presence of a supportive environment.
Q: How long does it take for the brain to heal after quitting an addiction?
A: The brain begins healing immediately after quitting, with significant improvements seen within the first year. However, full recovery, including emotional regulation and cognitive function, can take multiple years, depending on individual circumstances.
Sober Living: 7 Ways It Supports Long-Term Addiction Recovery
Sober living environments (SLEs)1 provide group housing for individuals recovering from substance use disorders.
These living spaces, also known as sober living homes, halfway houses, or recovery residences, create a structured and supportive atmosphere that helps residents’ transition back into everyday life after completing rehabilitation programs.
Sober living homes are designed to help individuals maintain sobriety by addressing the people, places, and things in their environment. These homes provide a structured setting1 that promotes accountability, peer support, and essential life skills. Below are seven key features that make sober living effective:

1. Substance-Free Environment
Residents must remain abstinent from drugs and alcohol while living in a sober home. This rule allows individuals to recover in a safe space free from triggers. Eliminating access to substances makes relapse more difficult, giving residents the opportunity to focus on their sobriety and coping strategies. Oftentimes, depending on the type of sober living, drug testing may be a part of accountability and maintaining a drug-free environment.
2. House Rules and Accountability
A lack of accountability is a common trait in addiction. Sober living homes enforce specific house rules, such as curfews, mandatory house meetings, and assigned chores, to instill discipline and responsibility. House managers oversee rule enforcement, ensuring everyone stays on track and remains accountable to themselves and their housemates. This can also include monitoring of activities and schedules, support systems, and even testing for drug use.
3. Support System and Peer Encouragement
Residents benefit from a built-in community of individuals2 who are also in recovery. Living with peers who share similar struggles fosters mutual support, encouragement, and accountability. This social reinforcement helps combat feelings of isolation and strengthens one’s commitment to sobriety. Some sober living homes require 12-step meetings or other types of peer support or social support.
How does sober living support long-term, sustained recovery?
Recovery housing can solidify someone’s journey in their recovery either post-treatment or while someone is attending treatment in an outpatient setting. Recovery housing ideally provides support, structure, community, accountability, and responsibility. Although many people choose not to go into recovery housing and can maintain successful recovery, the relationships and foundation that recovery housing can provide can be invaluable as a contribution to long-term success.
Tanya Kraege LCSW, CSAC, CCAR RC, WI CPS | Ventus Rex
4. Structured Daily Routine
Sober living environments3 emphasize the importance of structure. Residents follow daily routines that may include attending therapy sessions, support groups, exercising, and completing household chores. Establishing a consistent schedule helps individuals develop positive habits and reduce the time spent thinking about substance use. One of the main benefits of sober living is having structure as a next step after more formalized treatment or recovery programs.
5. Transition Assistance and Life Skills Training
Sober living homes often provide life skills training to help residents reintegrate into society. Programs may include budgeting, job searching, cooking, and relationship-building skills. These resources equip individuals with the tools needed to maintain independence and sustain long-term recovery. Depending on the level of care provided in the home, there may be additional options available for life skills or other educational opportunities.
6. Connection to Recovery Resources
Many sober living homes offer access to additional support services, such as therapy, job placement programs, and educational opportunities. These resources help residents continue their recovery journey beyond the sober living environment, ensuring they have the tools to maintain sobriety in everyday life.
7. Affordable Housing Options
Sober living costs vary depending on location, services, and amenities. Monthly expenses typically range from $300 to $2,000. Many homes operate on a sliding scale or offer financial assistance for those in need, making sober living an accessible option for individuals from different financial backgrounds. Some homes are credentialed and some operate like the Oxford House4 model.
Optimizing the Recovery Experience
Addiction impacts all aspects of a person’s life, requiring a holistic approach to recovery. For individuals with severe substance use disorders or co-occurring mental health conditions, sober living can provide a stable and supportive environment while they continue treatment. Programs such as cognitive behavioral therapy (CBT) and dialectical behavioral therapy (DBT) can help address both addiction and underlying mental health issues, improving overall well-being.
Here are some additional types of recovery support services along a path to sobriety and wellness.
How does sober living differ from traditional rehab?
Sober living offers a structured, substance-free environment where individuals can gradually transition back into daily life, often with fewer restrictions than traditional rehab. Traditional rehab, on the other hand, is typically more intensive with structured treatment programs, licensed therapy, other behavioral services, and medical supervision.
Andrew J. Schreier, ICS, CSAC, LPC, ICGC-II, BACC
Treatment Programs: A Path to Sobriety
Addiction treatment programs provide structured support to help individuals achieve long-term recovery. These programs vary in intensity and approach but generally include the following components:
- Assessment and Evaluation: Before beginning treatment, individuals undergo a comprehensive assessment to determine the severity of their addiction, identify co-occurring mental health disorders, and develop a personalized treatment plan.
- Detoxification: Detox is a critical first step in recovery. Medically supervised detox programs help individuals safely withdraw from substances while managing withdrawal symptoms. This step is especially important for individuals detoxing from opioids, benzodiazepines, or alcohol, as withdrawal can be life-threatening.
- Inpatient Treatment: Inpatient programs provide 24/7 care in a structured environment. Treatment typically includes individual therapy, group counseling, behavioral therapy, and holistic approaches. This immersive setting allows individuals to focus entirely on their recovery.
- Outpatient Treatment: Outpatient programs offer flexibility for individuals who can maintain independent living while attending scheduled therapy and support sessions. This option is ideal for those with a stable home environment and strong support system.
- Aftercare Planning: Long-term recovery requires ongoing effort. Aftercare planning includes continued therapy, support groups, and recovery resources to help individuals transition back into daily life while maintaining sobriety.
- Support Groups: Participation in 12-step programs, such as Alcoholics Anonymous (AA) or Narcotics Anonymous (NA), provides peer support, accountability, and encouragement from others who understand the challenges of addiction.
Bridging the Gap: Integrating Sober Living with Treatment
Sober living homes serve as a vital link between inpatient treatment and full independence. By combining structured treatment with sober living, individuals receive comprehensive support that enhances their recovery journey. This approach fosters long-term sobriety, equipping individuals with the tools and resources needed to reintegrate successfully into society.
If you or a loved one are seeking the best sober living environment, consider researching reputable options to find the right fit for your recovery needs.
If you or a loved one are seeking the best sober living environment, please consider one of the following that come highly recommended:
If you or a loved one are seeking the best sober living environment, consider ARC Stone Lodge in Louisa, Kentucky, which provides a structured, supportive setting for recovery. The Southeast Addiction Center, with locations in Georgia and Tennessee, offers comprehensive addiction treatment alongside sober living options. The Pennsylvania Recovery Center in Phoenixville, Pennsylvania, is another highly regarded facility for those in need of a supportive transition.
For young men seeking specialized sober living, Sandstone Care Young Men’s Sober Living in Maryland provides tailored support. The Massachusetts Center for Addiction in Weymouth, Massachusetts, also offers structured sober living programs designed for long-term recovery. Additionally, Lantana Recovery Connecticut in New Milford provides a supportive recovery-focused community for individuals seeking a sober lifestyle.
For a broader list of recommended sober living homes that match individual recovery needs, check out the comprehensive sober living directory for more options.
This version integrates the recommended facilities smoothly within the text while keeping it natural and informative. Let me know if you need any further tweaks!
Frequently Asked Questions
Q: What is the meaning of sober living?
A: Sober living refers to a structured, substance-free environment that supports individuals in recovery from addiction. It provides a safe space where residents can rebuild their lives and develop the skills needed for long-term sobriety.
Q: What do you do in sober living?
A: In a sober living home, residents follow house rules, attend recovery meetings, engage in therapy or counseling, complete household chores, and develop essential life skills to maintain independence and sobriety.
Q: How long do most people stay in sober living?
A: The length of stay varies based on individual needs, but most residents stay between 90 days and a year. Some may stay longer if they require extended support before transitioning to independent living.
Q: What does it mean to live a sober life?
A: Living a sober life means abstaining from drugs and alcohol while actively engaging in healthy behaviors, relationships, and coping strategies. It involves maintaining mental, physical, and emotional well-being without substance use.
Q: What is a sober living home?
A: A sober living home is a residential facility that provides a drug- and alcohol-free environment for individuals in recovery. It offers structure, accountability, and peer support to help residents transition from rehab to independent living.
Q: What are sober living house rules?
A: Sober living homes enforce house rules such as maintaining sobriety, attending meetings, adhering to curfews, completing assigned chores, and participating in house meetings. These rules help create a structured and supportive environment.
Q: What is a halfway house?
A: A halfway house is a transitional residence for individuals recovering from addiction or leaving incarceration. It provides temporary housing with structured programs, support services, and supervision to help residents reintegrate into society.
Q: Are you covered for addiction treatment?
A: Insurance coverage for addiction treatment, including sober living, varies by provider and policy. It’s essential to check with your insurance company to determine coverage for treatment, therapy, or transitional housing programs.
Q: Does the sober living home you are considering provide access to mental health resources and community support?
A: Many sober living homes offer access to therapy, counseling, peer support groups, job assistance, and other mental health resources. It’s important to research a home’s available services to ensure they align with your recovery needs.
Q: What are halfway house rules?
A: Halfway houses typically have structured rules, including mandatory sobriety, curfews, participation in treatment programs, job search requirements, and adherence to behavioral guidelines. These rules help residents transition back into society successfully.
Q: How does sober living support recovery from addiction?
A: Sober living homes provide a stable, substance-free environment where residents receive peer support, structure, and access to recovery resources. This setting helps individuals build coping skills, accountability, and a strong foundation for lasting sobriety.
Q: How does sober living differ from traditional rehab?
A: Unlike inpatient rehab, which offers intensive treatment in a clinical setting, sober living provides a less restrictive, transitional environment where residents can practice independent living while still receiving recovery support.
Q: How does sober living help in addiction recovery?
A: Sober living homes foster long-term recovery by reinforcing healthy routines, peer support, and access to therapy and life skills training. They help individuals build resilience, stability, and self-sufficiency after rehab.
What Is Harm Reduction For People Who Use Drugs?
Harm reduction is a practical and compassionate approach to helping people who use drugs. It focuses on reducing the negative effects of substance use, rather than demanding total abstinence. For people with substance use disorder, harm reduction meets them where they are at and supports them in staying safer, healthier, and more informed. Instead of judging or punishing people for their choices, harm reduction provides resources and care to improve their well-being.
What Does Harm Reduction Mean?
Harm reduction recognizes that not everyone is ready or able to stop using drugs right away. Instead of pushing for immediate change, it focuses on smaller, realistic steps to make substance use less risky. These steps aim to:
- Prevent overdoses.
- Reduce the spread of diseases, like HIV or hepatitis.
- Improve physical and mental health.
- Connect people to support and services.
Harm reduction doesn’t mean encouraging drug use—it’s about reducing harm while treating people with dignity and respect.
Why Is Harm Reduction Important?
Substance use disorder is a complex issue, and people often face barriers to quitting, like stigma, mental health challenges, or lack of resources. Harm reduction provides help without judgment, which makes it more likely that people will seek support. Here’s why it matters:
- Saves Lives: Programs like naloxone distribution (to reverse overdoses) and supervised consumption sites prevent deaths caused by drug use.
- Builds Trust: Offering nonjudgmental help encourages people to engage with health services and seek more support when they’re ready.
- Reduces Costs: Preventing overdoses and diseases lowers healthcare expenses for communities.
- Empowers Individuals: Harm reduction respects personal choice while offering tools to stay safe.
Examples of Harm Reduction Strategies
Harm reduction can take many forms. Here are some common strategies:
1. Naloxone Distribution
- Naloxone is a medication that reverses opioid overdoses. Harm reduction programs provide it to individuals and families, teaching them how to use it in emergencies.
2. Syringe Exchange Programs
- These programs give people access to clean needles and syringes, reducing the spread of infections like HIV or hepatitis. They also offer a safe way to dispose of used needles.
3. Safe Consumption Sites
- These are supervised places where people can use drugs in a safer environment. Medical staff are available to prevent overdoses and provide care if needed.
4. Education on Safer Use
- Harm reduction programs teach people about safer drug use, like not sharing needles or using test strips to check for fentanyl contamination.
5. Access to Healthcare
- Many harm reduction programs connect people to doctors, mental health support, and social services, improving overall well-being.
Harm Reduction and Recovery
Harm reduction doesn’t conflict with recovery—it supports it. For many people, harm reduction is the first step toward recovery. By reducing risks and building trust, these programs create opportunities for people to seek help when they’re ready.
For example:
- Someone who accesses a syringe exchange program might later decide to enter treatment.
- A person using naloxone to prevent overdoses may feel motivated to explore recovery options after connecting with a harm reduction worker.
Recovery looks different for everyone, and harm reduction provides the foundation for change.
Breaking Stigma with Harm Reduction
One of the biggest barriers people with substance use disorder face is stigma—judgment or negative attitudes from others. Harm reduction helps fight this stigma by treating people with respect and compassion, no matter where they are in their journey. It sends a powerful message: everyone deserves care and dignity.
Harm Reduction Saves Lives
Harm reduction is about more than just safety—it’s about meeting people where they are at and helping them move forward, one step at a time. It saves lives, protects communities, and provides hope for a better future. By focusing on reducing harm, we can support people with substance use disorder in ways that are practical, respectful, and life-changing.
Understanding the 6 Stages of Change in Substance Use Disorder
Recovering from substance use disorder is a journey, and like any journey, it happens in stages. People don’t usually wake up one day and decide to change their lives overnight. Instead, recovery is a process that happens step by step. Experts call this process the stages of change, and understanding these stages can help people recognize where they are and how to move forward.
What Are the Stages of Change?
The stages of change describe how people work through their decision to change behavior. These stages are part of a model called the Transtheoretical Model, created by psychologists to explain how people overcome challenges like addiction. There are six main stages:
- Precontemplation
- Contemplation
- Preparation
- Action
- Maintenance
- Relapse (or Lapse)
Let’s break down each stage.
1. Precontemplation: “I Don’t Have a Problem.”
In this stage, people don’t think they have an issue with substance use, or they aren’t ready to consider changing. They might:
- Deny their substance use is a problem.
- Blame others for their situation.
- Avoid talking about their behavior.
During this stage, family and friends often notice the problem before the person does. It’s a time of denial and avoidance.
2. Contemplation: “Maybe I Should Change.”
In the contemplation stage, people start thinking about their behavior and whether they should change. They might:
- Recognize the negative effects of substance use.
- Feel conflicted about quitting.
- Start weighing the pros and cons of changing.
This stage is about becoming aware, but the person may not be ready to act yet. It’s the first step toward making a decision.
3. Preparation: “I’m Ready to Do Something.”
When someone reaches the preparation stage, they’ve decided to make a change. They start planning how to take the first steps toward recovery. This might include:
- Researching treatment options.
- Talking to a doctor, counselor, or recovery coach.
- Setting goals for quitting or cutting back.
Preparation builds momentum, making the person feel more confident and ready to move forward.
4. Action: “I’m Making Changes.”
The action stage is when people take real steps toward recovery. This could mean:
- Starting treatment or attending support groups.
- Making lifestyle changes, like avoiding triggers.
- Practicing healthier coping strategies.
During this stage, individuals work hard to stick to their goals. It’s challenging, but it’s also empowering as they start to see progress.
5. Maintenance: “I’m Staying On Track.”
Maintenance is all about keeping the changes going over time. In this stage, people:
- Develop routines that support their substance use goals.
- Continue attending therapy or support groups.
- Handle cravings and challenges without relapsing.
The goal of this stage is to build a stable, fulfilling life in recovery. It takes ongoing effort, but with time, the new habits become part of everyday life.
6. Relapse: “I Slipped, but I Can Try Again.”
Relapse, or a return to substance use, is a common part of recovery. It doesn’t mean failure; it’s a chance to learn and grow. People in this stage might:
- Identify triggers or challenges that led to the relapse.
- Revisit their goals and recovery plan.
- Seek extra support to get back on track.
Many people go through this stage several times before reaching long-term recovery. What matters most is staying committed and not giving up.
Recovery Is a Journey, Not a Straight Line
The stages of change show that recovery is not always a smooth path. People might move forward, stay in one stage for a while, or even slip back to an earlier stage. What’s important is that change is possible at every step. With patience, support, and determination, people can overcome substance use disorder and build a healthier future.
If you or someone you know is working through these stages, remember: each step is progress, and it’s never too late to seek help. Recovery is possible, one stage at a time.
The Pros and Cons of Moderation Management for Alcohol Use: Wes Arnett
When someone struggles with drinking, they often have to decide how to make a change. Many people choose to quit drinking entirely, but others look into a different option called moderation management. This approach focuses on drinking less instead of stopping completely.
Moderation management can be helpful for some people, especially if they don’t feel their drinking is out of control. However, it’s not the best choice for everyone. Let’s take a closer look at what moderation management is, the good things about it, and the challenges it might bring.
What Is Moderation Management?
Moderation management is a way to cut back on alcohol without quitting completely. It’s meant for people who:
- Want to drink less but don’t want to stop entirely.
- Don’t have a severe problem with alcohol.
- Are willing to set rules for themselves about how much they drink.
The goal of moderation management is to help people create healthier habits and reduce the harm alcohol can cause.
Pros of Moderation Management
1. Flexibility
- You don’t have to stop drinking altogether, which makes this option feel more manageable for some people.
2. Personalized Goals
- You set your own limits, like how many drinks you’ll have in a week or avoiding drinking in risky situations.
3. Increases Awareness
- Moderation management encourages people to track their drinking, which helps them notice patterns and triggers.
4. Keeps Social Connections
- For people who worry that quitting drinking might make them feel left out in social situations, moderation management allows them to still join in while drinking less.
5. Easy to Start
- Some people may feel uncomfortable with labels like “alcoholic.” Moderation management can feel like a more approachable way to begin making changes.
Cons of Moderation Management
1. Not for Severe Alcohol Problems
- Moderation management isn’t recommended for people with severe alcohol use disorder. For these individuals, even small amounts of alcohol can quickly lead to bigger problems.
2. Requires Self-Control
- You have to stick to the limits you set. If you’ve struggled with self-control before, MM might not work as well.
3. Slippery Slope
- Drinking in moderation can make it harder to notice when you’re slipping back into unhealthy patterns.
4. Limited Support
- Moderation management doesn’t have the same kind of built-in support system that other support group programs or professional treatment programs offer.
5. Success Rates Vary
- While some people are able to successfully cut back, others find it hard to stick with moderation long-term.
Who Might Benefit from Moderation Management?
Moderation management can work well for people who:
- Have mild or moderate drinking issues, but not severe alcohol use disorder.
- Are committed to tracking their drinking and sticking to limits.
- Feel confident they can stay in control.
- Want to try cutting back before deciding if they need to quit entirely.
When Is Abstinence a Better Choice?
For some people, quitting alcohol completely is the safest and most effective option. This might be the case if you:
- Have been diagnosed with severe alcohol use disorder.
- Have tried to drink in moderation before but couldn’t stick to it.
- Experience withdrawal symptoms when you stop drinking.
- Have mental health challenges that alcohol makes worse.
Final Thoughts
Moderation management can be a good starting point for people who want to cut back on drinking without stopping completely. It offers flexibility and control, but it also takes effort and self-discipline. For additional information visit Moderation.org. For people with more serious drinking problems, abstinence or professional treatment might be a better fit.
The most important thing is to choose the option that works best for you and helps you live a healthier, happier life. Whether it’s moderation, quitting alcohol entirely, or a mix of both, taking steps toward change is something to be proud of.
Recovery Coaches 101: Inspiring Hope for People with Substance Use Disorder: Wes Arnett
Having a substance use disorder can feel overwhelming. For many people, it’s a struggle that comes with feelings of shame, loneliness, and hopelessness. But there’s good news: help is available, and recovery is possible. One of the most inspiring forms of support comes from recovery coaches. These dedicated individuals play a crucial role in helping people on their journey to overcoming addiction. Let’s explore how recovery coaches inspire hope and make a difference.
What Is a Recovery Coach?
A recovery coach is someone who provides guidance, encouragement, and support to people working to overcome substance use disorder. They are not doctors, counselors, or therapists. Instead, recovery coaches are mentors and allies who walk alongside people in recovery. Many recovery coaches have personal experience with addiction, which allows them to connect with others on a deep and understanding level.
The Power of Sharing Stories
One of the most powerful ways recovery coaches inspire hope is by sharing their own stories. Hearing from someone who has been through similar struggles and come out stronger can be incredibly motivating. It shows that recovery is possible, even when it feels out of reach. Coaches often share how they overcame challenges, rebuilt their lives, and found joy in sobriety. These stories remind people in recovery that they’re not alone and that a brighter future is within their grasp.
Providing Practical Support
Recovery coaches also help with the practical side of recovery. This might include:
- Setting Goals: Recovery coaches help individuals set realistic goals, such as finding a job, reconnecting with family, or improving physical health.
- Navigating Resources: Coaches connect people with treatment programs, support groups, housing, or job training.
- Building Skills: They teach coping strategies to handle cravings, stress, and setbacks.
By helping individuals take small, manageable steps toward their goals, recovery coaches make the process of rebuilding a life in recovery feel achievable.
Being a Source of Encouragement
Recovery isn’t a straight line—it has ups and downs. Recovery coaches are there to provide encouragement, especially during tough times. They celebrate victories, no matter how small, and remind people of their progress. This support helps people stay motivated and keeps them from feeling defeated by setbacks.
Creating a Judgment-Free Zone
One of the biggest challenges for people with substance use disorder is the stigma they often face. Recovery coaches create a safe, judgment-free space where individuals can open up about their struggles without fear of criticism. This compassionate approach helps people feel understood and valued, which is essential for building self-esteem and trust.
Inspiring Hope Every Step of the Way
At the heart of their work, recovery coaches inspire hope. They show that recovery isn’t just about quitting substances—it’s about rediscovering a meaningful life. By offering guidance, support, and a belief in the possibility of change, recovery coaches help individuals see the potential within themselves.
Substance use disorder can be isolating, but recovery doesn’t have to be. With the help of a recovery coach, people can find the strength, confidence, and hope they need to move forward. Their message is clear: You’re not alone, and recovery is possible.
Do All Recovery Coaches Have Lived Experience with Substance Use?
Not all recovery coaches have personal experience with substance use. While many do, it’s not something every recovery coach has. Having personal experience with addiction and recovery can be very helpful for a recovery coach. It allows them to connect with others on a deeper level and offer empathy, understanding, and insight into the struggles and successes of recovery. However, it’s important to know that personal experience isn’t the only thing that makes a good recovery coach. Some excellent coaches are trained and certified but don’t have personal experience with substance use, and the people they help don’t see this as a problem.
In the end, the most important thing is to find a recovery coach you feel comfortable with, and who can support you in reaching your recovery goals. If working with a recovery coach who has lived experience with substance use disorder is important to you, definitely ask this question when you are interviewing a potential coach to work with.
10 Things a Recovery Coach Can Help You With
As you work through your recovery journey, having a recovery coach can be a big help. A certified recovery coach is a trained professional who offers support, encouragement, and guidance to people recovering from substance use disorder. Here are ten things a recovery coach can work with you on:
- Setting Recovery Goals
Help you identify and define realistic short-term and long-term goals for your recovery journey. - Developing a Personalized Recovery Plan
Create a customized plan that addresses your specific needs, challenges, and strengths. - Exploring Recovery Pathways
Introduce you to various recovery pathways, such as 12-step programs, harm reduction approaches, or many other methods, and support the path that works best for you. - Identifying Triggers and Coping Strategies
Work with you to recognize triggers for substance use and develop healthy coping mechanisms to manage cravings and stress. - Building a Support Network
Help you connect with recovery groups, support networks, and community resources to strengthen your support system. - Improving Life Skills
Assist in developing essential skills like time management, budgeting, communication, and problem-solving to support a stable recovery. - Navigating Resources
Guide you in accessing treatment programs, housing assistance, healthcare, employment opportunities, and other community resources. - Enhancing Accountability
Provide regular check-ins and encouragement to help you stay on track with your recovery goals. - Learning Stress Management Techniques
Teach strategies for managing stress, such as mindfulness, meditation, exercise, and other self-care practices. - Building Healthy Relationships
Support you in creating and maintaining positive relationships that foster recovery and reduce exposure to toxic influences.
Working with a recovery coach can have many benefits and make a positive difference in your journey toward lasting recovery and well-being. If any of the above ways a coach can help spark your interest, consider exploring the option of working with a coach during your recovery journey.
Choosing the Right Recovery Coach: A Partner on Your Path
Choosing a recovery coach is an important decision that can make a big difference in your recovery journey. To find the right coach for your needs, keep these aspects in mind.
Qualifications and Experience
Look for a coach who has formal training in recovery coaching or peer support, and holds a current certification. Don’t hesitate to ask about their training and certifications—it’s completely okay to do so. While qualifications matter, it’s also important to think about their experience helping people with challenges similar to yours.
Share the challenges you’re facing and ask the coach if they have experience working with those things. For some people, it might not matter if the coach has personal experience with the same substance they’re struggling with, but for others, that connection can be very important.
Recovery Pathway Approach
Choose a coach whose approach feels right for you. Some coaches focus on specific recovery pathways, like the 12-Step program used by Alcoholics Anonymous or Narcotics Anonymous. If that’s what you’re looking for, that’s great! But if you’re not interested in the 12-Step approach, working with a coach who focuses on it might not be the best fit for you.
If you’re open to exploring other recovery pathways, be sure to ask the coach about their experience with and knowledge of other pathways. It’s important to find someone who matches your needs and can help you build the skills and strategies to succeed.
Personal Connection
Having a strong connection with your coach is very important. Look for someone who is empathetic, kind, and non-judgmental. A good coach should make you feel safe and supported while building trust with you. Communication is key, so choose someone who listens well and speaks clearly. It’s often said that a good coach should listen more than 90% of the time and talk less than 10%.
During your conversation with a potential coach, pay attention to whether they truly listen to you. Also, remember that it’s okay to switch to a different coach if you don’t feel the connection you need. Finding the right fit is what matters most.
Tips Having a Successful Relationship with Your Recovery Coach
Having a successful relationship with your recovery coach can greatly improve long-term recovery success. Building a strong, trusting, and supportive relationship can take time but is well worth the effort. Here are some tips that can help nurture that relationship:
1. Open and Honest Communication:
- Share openly: Be honest and transparent about your struggles, successes, and challenges.
- Ask questions: Don’t hesitate to ask questions, no matter how small or silly they may seem.
- Provide feedback: Share your thoughts and feelings about the coaching sessions and your time together.
2. Active Participation:
- Set goals: Work with your coach to set realistic and achievable goals.
- Take initiative: Be proactive in your recovery by taking steps to improve your well-being.
- Follow through: Commit to your recovery plan and follow through on your commitments.
3. Trust and Respect:
- Build trust: Be reliable and consistent in your communication and actions.
- Respect boundaries: Understand and respect your coach’s boundaries and professional limitations.
- Value their expertise: Recognize your coach’s knowledge and experience, then tap into these so you gain benefits.
4. Self-Awareness:
- Reflect on your progress: Regularly assess your progress and be willing to identify areas for improvement.
- Be honest with yourself: Acknowledge your strengths and weaknesses.
- Practice self-compassion: Be kind to yourself and avoid self-criticism. Giving yourself some grace goes a long way when a roadblock is encountered.
5. Positive Attitude:
- Maintain hope: Believe in your ability to recover and live a fulfilling life.
- Embrace challenges: View challenges as opportunities for growth and learning.
- Celebrate successes: Acknowledge your accomplishments, no matter how small, and celebrate them.
What Does it Mean to “Meet Someone Where They Are At” When Talking About Recovery Coaching?
“Meeting someone where they are” in recovery coaching and peer support means customizing the support to fit the person’s current stage of recovery and their specific needs. It’s about understanding their situation, feelings, and challenges without judging them or pushing them too hard.
Here are some key aspects of this approach:
- Empathy and Understanding: This involves actively listening to the person’s experiences and feelings without judgment.
- Non-Judgmental Attitude: Creating a safe and supportive space where the individual feels comfortable sharing their thoughts and feelings.
- Individualized Approach: Recognizing that each person’s recovery journey is unique and customizing support accordingly.
- Setting Realistic Goals: Setting achievable goals that are aligned with the person’s current situation, capabilities, and motivation.
- Flexibility: Being adaptable and willing to adjust the approach as needs change.
By meeting people where they are, recovery coaches and peer supporters can build trust, inspire hope, and encourage individuals to take the steps needed for long-term recovery.
The Difference Between a Recovery Coach and a Sponsor
The journey to recovery from substance use disorder is filled with challenges and victories. Along the way, individuals often rely on various support systems to guide them, including recovery coaches and sponsors. While both offer valuable support, their roles and approaches are different, each serving unique purposes.
Imagine recovery as a ship navigating the stormy seas of addiction. In this analogy, the recovery coach is the captain, and the sponsor is the sailor. The recovery coach, like a captain, takes charge of steering the ship to safety. They use their training and experience to navigate the unpredictable waves, storms, and obstacles, ensuring the ship stays on course. The sponsor, like a sailor, works alongside others on the ship. They use their personal experience with past storms to guide and encourage, focusing on specific tools and methods that helped them succeed. Both roles are distinct, but both are essential for a successful voyage.
Recovery Coaches: The Captain of the Journey
Recovery coaches are trained professionals who guide individuals through their recovery process. They help create personalized recovery plans, connect people with essential resources, and build life skills. Recovery coaches support many different recovery pathways and empower individuals to choose the one that works best for them.
One of their main roles is to provide ongoing encouragement and show that recovery is achievable. They focus on individuals’ strengths, help set goals, and offer various levels of accountability based on what the individual prefers. Recovery coaches also help individuals develop strategies to manage stress, cravings, and other challenges. They may accompany individuals to support group meetings, healthcare appointments, or legal meetings, offering practical and emotional support.
Additionally, recovery coaches assist with basic needs like housing, employment, and healthcare by connecting individuals with appropriate resources. These practical supports help individuals stabilize their lives so they can focus on their recovery. Sponsors, in contrast, generally do not assist with these needs.
Sponsors: A Fellow Sailor on the Journey
Sponsors are typically individuals in recovery who volunteer to support others. They share their personal experiences, provide guidance, and offer limited accountability. The sponsor-sponsee relationship is often rooted in 12-step programs like Alcoholics Anonymous or Narcotics Anonymous, where the sponsor helps the sponsee work through the 12 steps.
Unlike recovery coaches, sponsors tend to focus on one recovery pathway—the one they’ve personally followed. They provide empathy, encouragement, and practical advice for staying sober. By sharing their own struggles and successes, sponsors inspire and motivate others to keep going.
Sponsors and sponsees usually have check-ins, either in person, over the phone, or by text. These check-ins are generally less frequent than those with a recovery coach but still provide opportunities to monitor progress, address challenges, and offer support. Sponsors often encourage regular attendance at 12-step meetings and participation in recovery activities.
The Best of Both Worlds
Understanding the differences between a recovery coach and a sponsor can help you decide which type of support might be right for you—or if working with both is the best choice. While there are similarities in their roles, their differences mean they often complement each other well. Many people find that having both a recovery coach and a sponsor creates a more comprehensive support system, combining the professional guidance of a coach with the shared experience and empathy of a sponsor.
Both roles are vital in their own way, and together, they can provide the tools, encouragement, and support needed for a successful and lasting recovery journey.
