Life can throw unexpected curveballs, leaving us feeling lost, overwhelmed, and disconnected. For many, navigating the aftermath of trauma can feel like an insurmountable challenge, impacting not only their own well-being but also the lives of those around them. Yet, as one individual’s journey illustrates, seeking help can provide a pathway to profound transformation, even when circumstances remain largely the same.
1. Recognizing the Need for Help: The Unseen Struggle
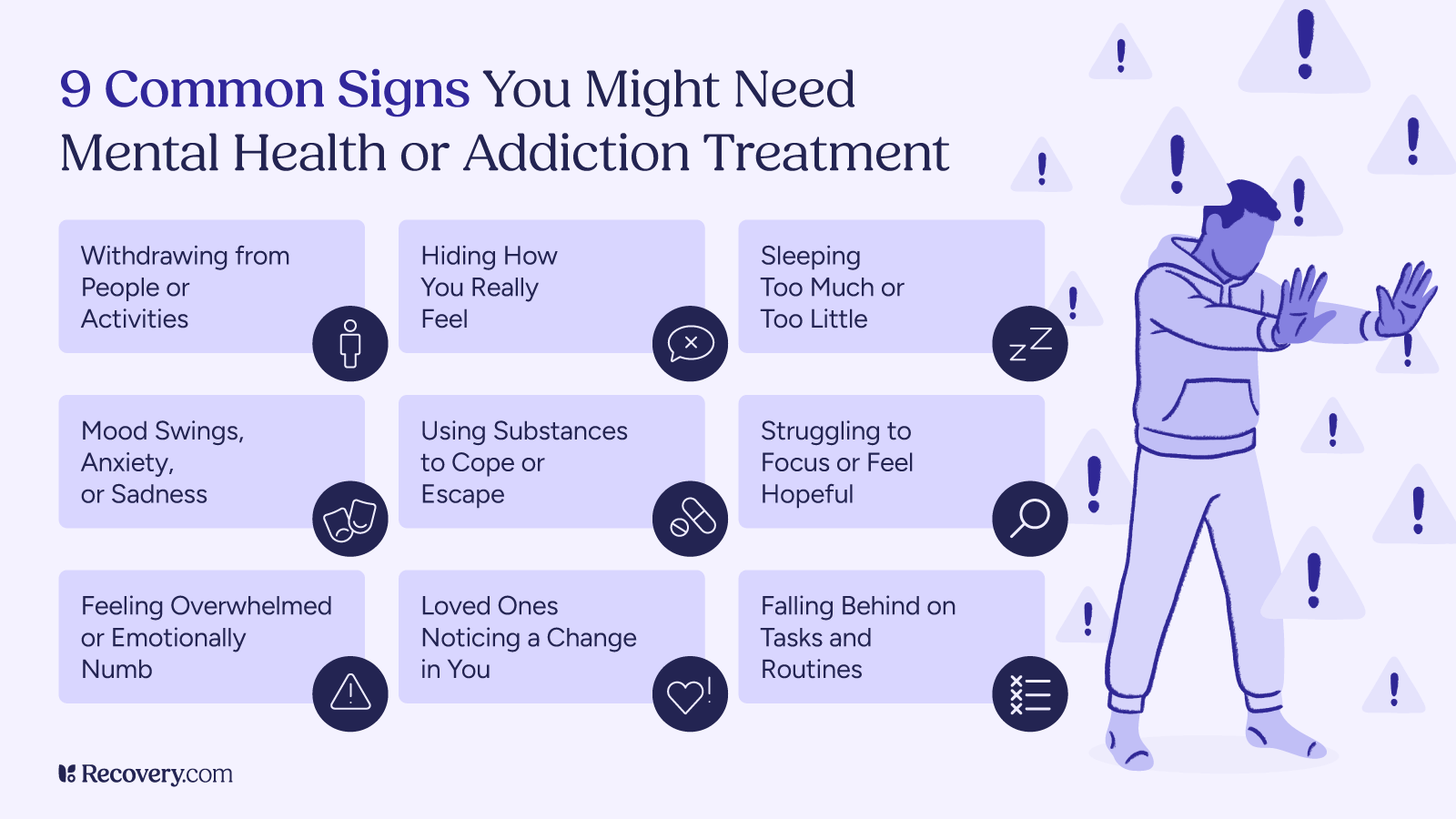
Often, the individuals most in need of support are the last to recognize the depth of their struggle. This was certainly the case for Jonas, who found himself in a chaotic and dark period of his life, grappling with an abusive relationship and the heartbreaking loss of contact with his children. Despite his internal turmoil, it was his sister who ultimately identified the severity of his situation and recommended trauma treatment at InHarmoni Rehab. As Jonas recounts, “I didn’t really understand in what kind of position I was in. Before she told me I needed to go, of course I realized that I was using sleeping pills in order to sleep, and things were going not in the right direction. I could see the signs, but I could not understand it myself.”
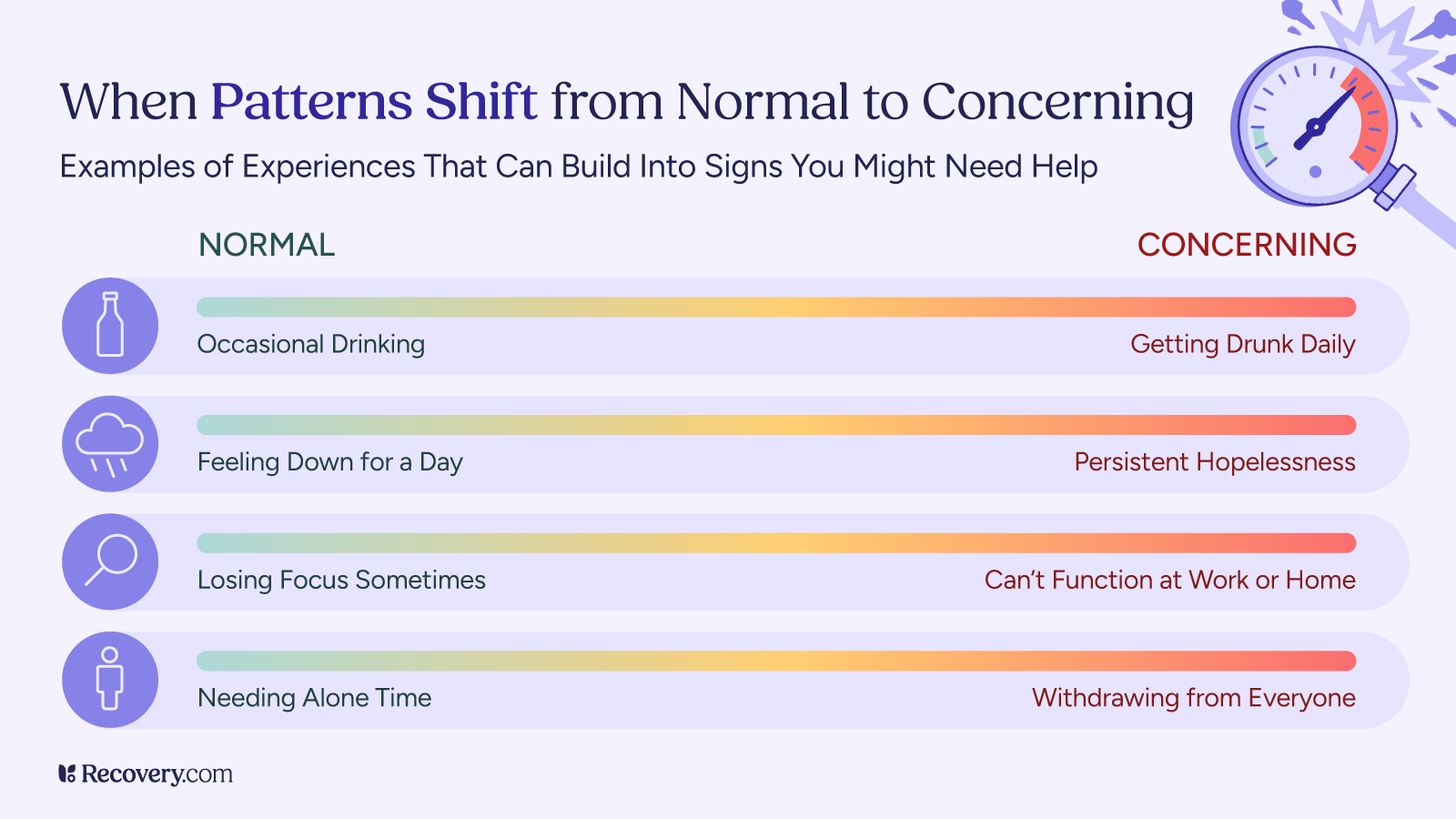
This sentiment underscores a critical aspect of mental health: self-awareness can be a significant barrier when deeply entrenched in emotional pain. External perspectives from loved ones can be invaluable in these moments, offering a lifeline when an individual is unable to objectively assess their own needs. The signs—such as relying on substances like sleeping pills to cope—were present, yet the emotional toll prevented Jonas from fully grasping the extent of his struggles. This often happens because trauma can impair our ability to regulate emotions and make sound judgments, leading to a distorted view of reality and a reluctance to seek help.
2. Overcoming Skepticism: A Leap of Faith Towards Healing
The decision to enter treatment is rarely an easy one, often accompanied by a healthy dose of skepticism and apprehension. Jonas admits, “My expectations going into treatment was quite on the skeptical side. I didn’t think I could do much about changing my behavior and my mood because of the state and my life situation. So I would say that I was quite skeptical.” This initial doubt is a common hurdle for many seeking help for trauma. The weight of past experiences and the belief that one’s situation is unchangeable can create a powerful barrier to embracing the possibility of recovery.
However, moving past this skepticism is often the first and most crucial step towards healing. It requires a willingness to suspend disbelief and take a leap of faith, even when the path ahead seems uncertain. This initial acceptance, even if hesitant, opens the door to new perspectives and strategies for coping. For those contemplating treatment, it’s important to acknowledge these fears and recognize that they are a normal part of the process. Trusting in the therapeutic process, even when doubts linger, can unlock profound personal growth.
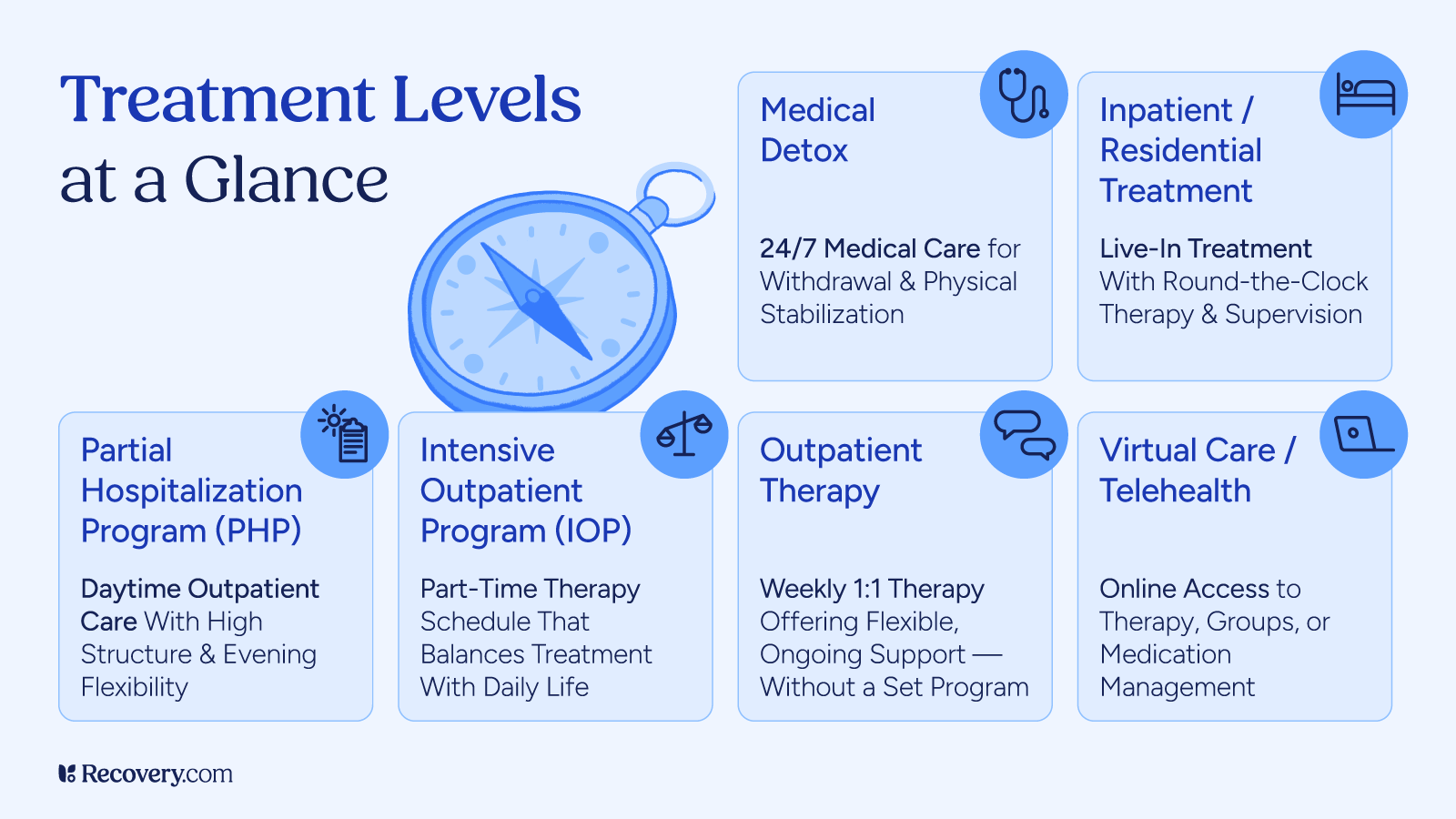
Explore trauma treatment options.
3. The Ripple Effect of Healing: A New Perspective on Connection
One of the most profound realizations Jonas experienced in rehab was the interconnectedness of his well-being with those around him. He discovered that his emotional state and behaviors had a significant impact on his friends, family, and ultimately, his children, even in their absence. “Well, I would say that rehab gave me a brand new perspective on life. I realized that it’s not only me that matters because the way I feel and behave affects everybody around me. And if I don’t feel well, My friends, my family, and everybody will be affected.”
This shift in perspective is a cornerstone of trauma recovery. It moves beyond individual suffering to encompass the broader relational context. When individuals heal from trauma, the positive effects radiate outwards, improving the quality of their relationships and creating a more positive environment for everyone involved. This understanding also empowered Jonas to maintain his strength for his children, recognizing that even without direct contact, his improved well-being could indirectly impact them. This concept aligns with attachment theory, which posits that our emotional well-being and relational patterns are deeply intertwined. A research article in Psychological Science in the Public Interest highlights the lasting impact of early attachment experiences on adult relationships and mental health, underscoring the importance of healing individual trauma for the benefit of broader relational systems.
4. Embracing Practical Skills: Tools for Lasting Change
Beyond theoretical insights, trauma treatment provides invaluable practical skills that empower individuals to navigate daily challenges and foster lasting change. For Jonas, two key practices stood out: morning meditation and a conscious effort to change his communication patterns. He notes, “And of course there was a lot of practical skills that I’m using every morning, especially the meditation and especially the way I communicate. I’m trying to change my communication patterns because I realized that that was one of the reasons why I ended up in the situation I was in.”
Meditation offers a powerful tool for mindfulness, allowing individuals to observe their thoughts and feelings without judgment and cultivate a sense of calm amidst chaos. It can help regulate the nervous system, which is often dysregulated in individuals with trauma.
Communication skills are equally crucial, especially for those whose past trauma may have impacted their ability to express themselves effectively or set healthy boundaries. Learning to communicate assertively, actively listen, and understand non-verbal cues can transform relationships and prevent recurring patterns of conflict. These skills are often taught in various forms of therapy, such as Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT), which are frequently used in trauma treatment.
5. Redefining “Better”: Thriving Amidst Unchanged Circumstances
Perhaps one of the most remarkable aspects of Jonas’s journey is his ability to thrive even when his external circumstances remained largely the same. He clarifies, “actually I would say that my life today is not much different. I’m not in a completely different situation. The situation is actually the same, although the way I feel in this situation is what has have changed. I can now handle the situation. I can now understand what I’m feeling, and I also understand that things will be as good as you make them.”
This powerful realization highlights that healing isn’t always about dramatically altering external circumstances, but rather about transforming one’s internal landscape. It’s about developing resilience, emotional regulation, and a proactive mindset to navigate life’s challenges. Before treatment, Jonas was “feeling worse and worse,” but now, even with similar external pressures, he’s “feeling better and better.” This shift in perspective and internal strength is a testament to the profound impact of trauma treatment. It demonstrates that true well-being stems from our ability to adapt, cope, and find inner peace regardless of external variables. This internal locus of control is a key factor in long-term recovery and resilience, as detailed by research on psychological well-being.
6. The Investment in Yourself: An Insurance for the Future
For those hesitating to seek treatment due to concerns about cost or efficacy, Jonas offers a compelling perspective: it’s an investment, an insurance for the future. He urges individuals to consider the broader implications of their well-being, emphasizing that the positive impact extends beyond themselves. “I would say that this is a really, really small investment compared to what it’s gonna cost you if you don’t make the investment. So I would see it as a, as an insurance. It’s an insurance for the future. You can change everything for the better. By taking this step, I wish you the best of luck.”
This powerful analogy underscores the long-term benefits of addressing trauma. The emotional, physical, and relational costs of untreated trauma can be immense, leading to chronic stress, strained relationships, and diminished quality of life. Investing in treatment is not just about alleviating immediate suffering; it’s about building a foundation for a healthier, more fulfilling future. It’s an investment in personal growth, improved relationships, and overall well-being. Thinking about the cost-benefit analysis of treatment can be a powerful motivator for many.
7. Taking the First Step: Embracing the Unknown
The journey to healing can feel daunting, filled with questions and uncertainties about the process, the environment, and the people involved. Jonas acknowledges these common fears: “maybe you are a little bit in the doubt about going, maybe you’re a little bit scared about, you know, how it’s gonna be like, maybe you’re thinking about what kind of people are you gonna meet? How is the premises gonna be? How is the food gonna be? How is, how is this gonna change me anyway? How can, how can a treatment change anything?”
His advice is simple yet profound: “I would say that the only thing you can do to find out is to take the step because you know where you’re at, you know what problems you have, and if you want to try to solve them, try to find a solution. I would say that this is a really good first step.”
This sentiment encapsulates the essence of taking control of one’s narrative. While uncertainties may linger, the potential for positive change far outweighs the fear of the unknown. Recognizing one’s current struggles and actively seeking solutions is the courageous first stride towards a brighter future. Embarking on a healing journey requires courage, self-compassion, and a willingness to embrace the transformative power of support.