When you’re living with an addiction, it can be hard to imagine recovery. Many people get lost in the negative, thinking about life without drugs or alcohol. But what about life with more time, energy, and emotional stability?
Addiction eats away at your resources. People lose money, relationships, their physical health—the list goes on and on. When you start healing, you’ll have so much more to work with. If you decide to attend a residential treatment center, experts can help you put those assets to use. And from there, you’ll start dreaming of—and planning for—a better future.
1. Your Mental Health Gets Better
Addiction affects both your physical and mental health. ((Addiction and health. National Institute on Drug Abuse. https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction/addiction-health)) And when you’re actively using drugs, the idea of withdrawal might sound even worse. That’s a valid fear. But it might not be a reality. With the right support, detox doesn’t have to be dangerous. Best of all, withdrawal and detox are temporary. And unlike continued substance use, they offer a lot to look forward to on the other side.
Focus More Easily
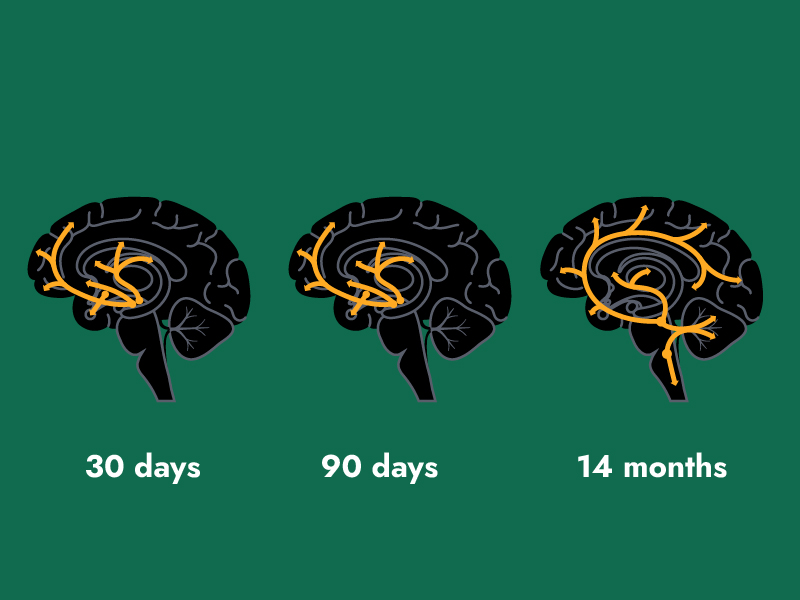
Addiction makes it hard to focus, ((Gould, T. J. (2010). Addiction and cognition. Addiction Science & Clinical Practice, 5(2), 4–14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3120118/)) reason, and learn new things. It can also interfere with your memory. This is because drugs quite literally change your brain. You might not even notice these issues at first, since they start so gradually. But shortly after getting sober, you can expect your mental state to improve. ((Module 10: Sobriety Sampling. (n.d.). Boston Center for Treatment Development and Training. https://www.mass.gov/doc/module-10-sobriety-sampling-0/download))
Manage Co-Occurring Symptoms
Studies show that 50% of people with addiction also have a mental health condition. ((Part 1: The connection between substance use disorders and mental illness. National Institute on Drug Abuse. https://nida.nih.gov/publications/research-reports/common-comorbidities-substance-use-disorders/part-1-connection-between-substance-use-disorders-mental-illness)) Because of this, many rehabs treat co-occurring disorders.
In these programs, you’ll learn how to manage your conditions in a healthy way. You may even find that just one type of treatment helps you heal from both addiction and another health issue. ((Pettinati, H. M., O’Brien, C. P., & Dundon, W. D. (2013). Current status of co-occurring mood and substance use disorders: A new therapeutic target. The American Journal of Psychiatry, 170(1), 23–30. https://doi.org/10.1176/appi.ajp.2012.12010112))
2. Your Physical Health Improves
Addiction takes a serious toll on your body, as well as your mind. And before treatment, you may not even be aware of all your physical symptoms. Most rehabs can treat these issues alongside your mental health. And during recovery, your health may start to improve in some unexpected ways.
- Recovery increases overall physical health. ((Laudet, A. (2013). Life in Recovery [Report on Survey Findings]. Faces and Voices of Recovery. https://facesandvoicesofrecovery.org/wp-content/uploads/2019/06/22Life-in-Recovery22-Report-on-the-Survey-Findings.pdf))
- Sexual function improves ((Ghadigaonkar, D. S., & Murthy, P. (2019). Sexual dysfunction in persons with substance use disorders. Journal of Psychosexual Health, 1(2), 117–121. https://doi.org/10.1177/2631831819849365)) when you stop using drugs.
- Liver damage stops as soon as you quit drinking ((Morgan, T. R. (2017). Treatment of alcoholic liver disease. Gastroenterology & Hepatology, 13(7), 425–427. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5572973/)) (but it can take months to see the full extent of healing).
- Heart function and blood pressure improve after one month of sobriety from alcohol. ((Thomes, P., Rasineni, K., Saraswathi, V., Kharbanda, K., Clemens D., Sweeney, S., Kubik, J., Donohue Jr., T., & Casey, C. (n.d.). Natural Recovery by the Liver and Other Organs After Chronic Alcohol Use. https://arcr.niaaa.nih.gov/volume/41/1/natural-recovery-liver-and-other-organs-after-chronic-alcohol-use))
- Addiction recovery lowers your risk of contracting infectious diseases ((Laudet, A. (2013). Life in Recovery [Report on Survey Findings]. Faces and Voices of Recovery. https://facesandvoicesofrecovery.org/wp-content/uploads/2019/06/22Life-in-Recovery22-Report-on-the-Survey-Findings.pdf)) like HIV/AIDS and hepatitis C.
3. You Kickstart a Healthy Lifestyle
There’s more to recovery than therapy. Even in rehab, you can engage in fun, fulfilling hobbies, like martial arts or cooking. These healthy coping tools can help you stay grounded after you complete treatment.
Sobriety can help you get your life on track in measurable, practical ways. Studies show that most people’s finances improve during addiction recovery. ((Laudet, A. (2013). Life in Recovery [Report on Survey Findings]. Faces and Voices of Recovery. https://facesandvoicesofrecovery.org/wp-content/uploads/2019/06/22Life-in-Recovery22-Report-on-the-Survey-Findings.pdf)) And that, in turn, can improve your mental and even physical health. Experts agree that financial stability decreases your chance of depression, ((Bialowolski, P., Weziak-Bialowolska, D., Lee, M. T., Chen, Y., VanderWeele, T. J., & McNeely, E. (2021). The role of financial conditions for physical and mental health. Evidence from a longitudinal survey and insurance claims data. Social Science & Medicine, 281, 114041. https://doi.org/10.1016/j.socscimed.2021.114041)) anxiety, and heart disease. This solid foundation can empower you to take healthy risks, like meeting new people.
4. You’ll Build a Sober Community
Sobriety can improve your relationships. ((Kemp, R. (2019). Addiction and addiction recovery: a qualitative research viewpoint. Journal of Psychological Therapies. 4. 167-179. https://www.researchgate.net/profile/Ryan-Kemp-3/publication/337410578_Addiction_and_addiction_recovery_a_qualitative_research_viewpoint/links/5e54e278299bf1bdb8395e12/Addiction-and-addiction-recovery-a-qualitative-research-viewpoint.pdf?_sg%5B0%5D=started_experiment_milestone&origin=journalDetail)) Many residential programs are built to support this. In rehab, you’re surrounded by people who support your healing goals. And once you start to repair your relationship with yourself and others, you’ll get to build a support network that has your back as you continue your journey.
This new community can be found through 12-Step meetings, non-12-Step support groups, sober living, or outpatient aftercare. Or, you could connect with people who share your interests. Whether you find a new hobby or pick up an old one, this can be a fun, low pressure way to find like-minded people.
If your previous social circle was built around drug use, this is your chance to form new, healthy relationships. And because forming social connections with other sober people can help prevent relapse, ((Study shows impact of social interactions on addictive behavior. (2018, October 15). National Institute on Drug Abuse. https://nida.nih.gov/news-events/news-releases/2018/10/study-shows-impact-of-social-interactions-on-addictive-behavior)) it’s an important part of your recovery.
5. You Have the Chance to Reconnect With Loved Ones
Addiction damages close relationships ((Lander, L., Howsare, J., & Byrne, M. (2013). The impact of substance use disorders on families and children: From theory to practice. Social Work in Public Health, 28(0), 194–205. https://doi.org/10.1080/19371918.2013.759005)) with both given and chosen family. But recovery empowers you to hone your interpersonal skills. And, in time, those skills might help you heal your family dynamic.
For Michael Waggoner, sobriety is an opportunity to reconnect with family. ((Michael waggoner. (2020, September 9). Faces & Voices of Recovery. https://facesandvoicesofrecovery.org/story/michael-waggoner/)) “I am rebuilding relationships with my family, I am rebuilding trust,” he says. “I am able to be a dad today and a positive influence in my son’s life.”
6. You Can Realize Your Higher Purpose
Experts say that “addiction is a response to boredom, loneliness, meaninglessness, and other existential struggles.” ((Thompson, G. R. (n.d.). Meaning Therapy for Addictions: A Case Study. https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.1026.5596&rep=rep1&type=pdf)) Sobriety can help you find your purpose, and go on to live a meaningful life. Instead of just coping with a series of problems, you can build confidence and start moving toward the future you want for yourself.
When he was addicted to alcohol, James Gibbon had “no hope for the future.” ((James gibbons. (2020, September 9). Faces & Voices of Recovery. https://facesandvoicesofrecovery.org/story/james-gibbons/)) He faced legal, financial, and relationship problems as a result. “I accepted the fact that I would never own a home, have a career, graduate from college, meet somebody special, and start a family,” he says. But after treatment:
“I began to see potential in myself. My confidence began to grow.”
The hard work of recovery can help you resolve past trauma, and teach you healthier coping strategies. With those skills, James achieved all the goals he thought were beyond him. And that isn’t unusual. When you stop using drugs and enter recovery, your potential for success only grows.
Sobriety Is Just the Beginning
It takes hard work to get and stay sober.
Healing isn’t just about stopping drug use. It’s about starting a new chapter.
And once you commit to recovery, you might be surprised by your own strength. That self-confidence is a powerful starting point.
Visit our directory of inpatient rehabs to learn more about their locations, services, pricing, and more.
Reviewed by Rajnandini Rathod