Eating disorders (EDs) are a serious mental health issue. And while they’re more common than you might think, it’s important to remember that eating disorders are treatable. People can and do recover from them.
Treatment for eating disorders comes in several forms: some people need, or prefer, to receive around-the-clock care from medical professionals and will opt for a residential rehab program. For those with a strong support network, an outpatient program may be a good fit. Eating disorders are complex, so one type of treatment isn’t necessarily better than the other. Here, we’ll guide you through the basics of eating disorders, along with different treatment options and common therapies:
- What’s an Eating Disorder?
- Signs and Symptoms
- Types of Eating Disorders: An Overview
- Common Causes of Eating Disorders
- Who Suffers from Eating Disorders?
- Where to Find Treatment
- Common Therapies for Eating Disorders
What’s an Eating Disorder?
The American Psychological Association defines eating disorders1 as any “abnormal eating habit that can threaten your health or even your life.” People who suffer from eating disorders may eat less or more than the recommended amount of food to be considered healthy. An estimated 30 million U.S. adults will have experienced some form of eating disorder2 at some point in their lives.
Eating disorders are serious mental health conditions that present both behavioral and physical symptoms.
Signs and Symptoms
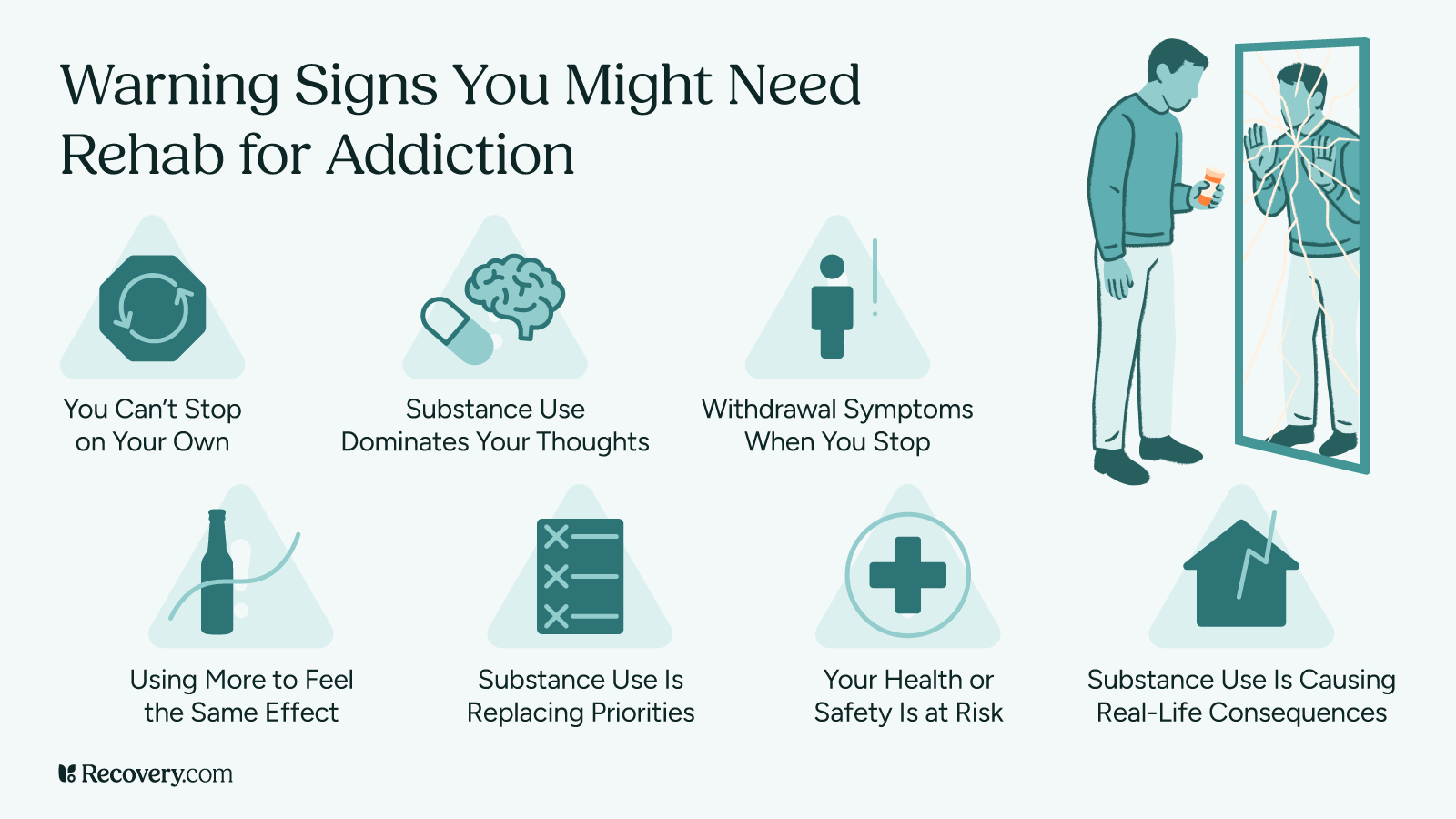
When you seek professional help for an eating disorder, your healthcare provider must give you a formal diagnosis before mapping out a treatment plan. They’ll look at your feeding and eating disorder symptoms3 as laid out in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). There are several different types of eating disorders defined in DSM-5, and each is distinct from the other. Some symptoms may apply to many of these disorders:
Behavioral Symptoms
- Excessively preoccupied with thoughts of food and body shape or image, making it difficult to focus on other areas of life
- Restricting calorie intake or refusing to eat certain foods like carbohydrates
- Engaging in compulsive eating habits like skipping meals, episodes of out-of-control eating, self-induced vomiting or over-exercising
- Anxious about eating around others
- Withdrawing from social contact and your usual hobbies
- Irritability or mood swings
- Hiding eating behaviors
Physical Symptoms:
- Noticeable weight fluctuations
- Dizziness or feeling lightheaded, commonly exacerbated by movement
- Digestive issues such as constipation, stomach cramps, bloating, and more
- Females may experience irregular periods or periods may stop completely
- Dental issues including cavities, sensitive teeth, and enamel erosion
- Muscle weakness
Types of Eating Disorders: An Overview
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) lists several different types of eating disorders:
- Anorexia nervosa
- Bulimia nervosa
- Binge eating disorder
- Avoidant/restrictive intake disorder
- Pica
- Rumination disorder
- Other specified feeding and eating disorders (OSFED) including:
-
- Muscle dysmorphia
- Orthorexia nervosa (ON) proposed criteria
People most commonly seek treatment for anorexia nervosa, bulimia nervosa, and binge-eating disorder.
Anorexia Nervosa
If you suffer from anorexia nervosa, you may experience intense feelings of self-consciousness and body image distortion, causing you to withhold food from yourself. People with anorexia often engage in extreme eating habits to lose weight. If you notice signs of anorexia, don’t take it lightly. Anorexia is one of the most fatal mental health issues4 in the U.S., with an estimated mortality rate of 10%.
Bulimia Nervosa
Bulimia nervosa is characterized by episodes of binge-eating followed by attempts to “purge” the food over the fear of gaining weight. People may attempt to “purge” through vomiting, laxatives, or over-exercising, all of which are harmful to the body.
Binge-Eating Disorder
Those with a binge-eating disorder experience recurring, vicious cycles of uncontrollable overeating. People often cite a loss of control during binge-eating episodes5. While everyone’s trigger for binge eating is different, it’s usually associated with high stress.
Common Causes of Eating Disorders
The exact cause of eating disorders is still inconclusive. However, there are several speculated risk factors that contribute to the development of eating disorders6.
Biological Factors
A significant number of medical studies suggest an association between genetics and eating disorders. A 2004 report detailing the genetics of eating disorders published in Psychiatry (Egmond) found “greater than 50% of the variance in liability to eating disorders and disordered eating behaviors can be accounted for by additive genetic effects.”7 More recently in 2013, the Annals of Neurosciences reported an “undeniable link between genetic factors and eating disorders.”8
Environmental Factors
A unique combination of environmental factors can contribute to body dissatisfaction. These might include societal pressure and other environmental influences like bullying in school, criticism from family members, and the idolization of certain body types. Teens and young adults are especially impressionable: body dissatisfaction among American teens9 reached new highs in the wake of the Covid-19 pandemic.
Trauma
The flood of emotions that follow a traumatic event can trigger an eating disorder, and it’s rather common for eating disorder patients to cite traumatic experiences. According to a study published in Eating Disorders The Journal of Treatment & Prevention, researchers found that “the prevalence of traumatic events in ED patients10 has ranged from 37% to 100%.”
Co-occurring Disorders
Eating disorders are a mental health issue that commonly co-occurs with other mental disorders. The National Association of Anorexia Nervosa and Associated Disorders reports that between 33% up to 50% of individuals with anorexia have co-occurring mood disorders11, like anxiety and depression.
Who Suffers from Eating Disorders?
Eating disorders can affect anyone regardless of gender, ethnicity, and age.
The American Psychological Association estimates that in the U.S., 20 million women and 10 million men will experience some form of eating disorder1 in their lives. While women are more likely to receive a diagnosis than men, the number of men who suffer from an eating disorder may be under-reported12. That may be because men aren’t as likely to seek treatment.
Eating disorders are more common among teenagers and young adult populations. According to the National Institute of Mental Health13, people normally start developing bulimia and anorexia at the age of 18, and 21 for binge eating. But eating disorders can still affect the elderly. Unfortunately, this is sometimes overlooked. A 2012 study published in the International Journal of Eating Disorders found that 13% of women in the U.S. aged 50 and older have eating disorder symptoms14.
Where to Find Treatment
If you think you or a loved one has an eating disorder, the earlier you find help the better. Untreated eating disorders can have serious and harmful effects on the body. In severe cases, eating disorders can be fatal. For example, the mortality rate for people who suffer from anorexia is 18 times higher15 than for individuals who don’t have eating disorders.
Many people start their recovery journey by talking to their primary care physician. They’ll begin by checking your medical history and vital signs to ensure you don’t need more serious care, like medication or hospitalization. If your case doesn’t require hospitalization, your physician may be able to point you towards local resources for treating eating disorders, like a dietician, therapist, or outpatient program.
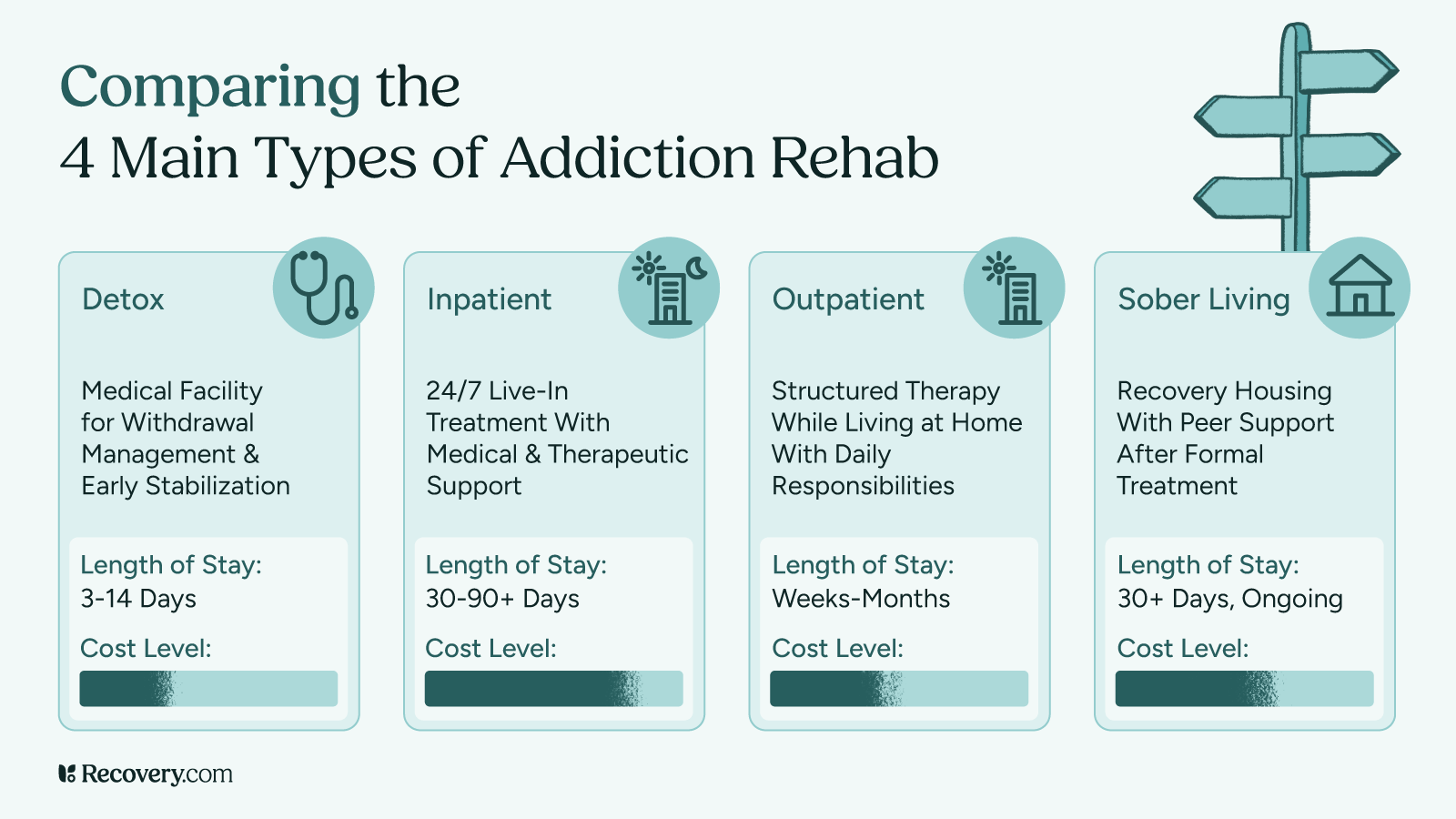
There are several levels of care for treating eating disorders. Each varies in intensity and is delivered in different settings.
Inpatient Programs (Residential Rehab)
In an inpatient program, you receive 24/7 clinical care on-site at a treatment center. This is the most intensive level of care and is usually recommended if patients exhibit worrying medical signs:
-
-
- laboratory findings that are abnormal or indicate critical health risks
- unstable vital signs including cardiac disturbances, hypothermia, hypotension, and more
- coexisting medical conditions that may result in further complications
-
You don’t need to have severe medical issues to enroll in an inpatient program. For some people, a change of scenery and stepping away from potential triggers is exactly what they need to successfully work towards long-term recovery.
Partial Hospitalization Program (PHP)
A PHP, also referred to as a “day hospital,” is less intensive than an inpatient program but more intensive than an IOP. In a PHP, you receive treatment at a clinic for around 3 to 5 days each week, 4 to 8 hours a day. You’ll go home each day after treatment.
Intensive Outpatient Program (IOP)
While outpatient programs still follow an intensive therapeutic schedule, you can go home each day after treatment rather than receive 24-hour medical monitoring. You can expect to go in for treatment 3 to 5 hours a day, around 2 to 3 days each week.
This option can work for people who have their symptoms under control enough to complete daily tasks. It’s also usually more cost-effective than inpatient programs. IOPs may be a good fit for people who have a strong support network at home.
Support Groups
Eating disorder support groups offer a network of peers who share similar experiences to yours and some provide educational information that could aid your recovery. There are two main types of support groups: self-help support groups and professionally operated support groups.
Self-help groups, also called “fellowships” or “peer support groups,” are organized by members of the group itself. The sense of comradery this creates can be important for many people in their recovery journey.
Professionally operated support groups are facilitated by professionals like a licensed therapist or a social worker. On top of offering a strong support network of peers, group discussions are led by staff with professional experience in the field of eating disorder treatment. These groups are often operated by hospitals, clinics, or treatment centers and may require a fee to attend.
Searching for Treatment Online
Most people turn to the internet to find eating disorder treatment programs. For the most part, quality treatment centers have their patients’ best interests at heart and help many find recovery each year. But some centers engage in ethically questionable practices. It’s important to be wary of these exploitative practices to protect yourself from rehab scams, which unfortunately do exist.
You can take extra precautionary steps to protect yourself from potential illegitimate rehabs when searching for eating disorder treatment online:
-
-
- Be wary of free helplines. Some websites may present information that appears unbiased, but require you to call a hotline. In some cases, these hotlines connect you with an agent who receives a referral fee for placing someone in a specific treatment center or program.
- Get your questions answered. During your call with any treatment provider, make sure their admissions team can answer specific questions you may have about their center and program. Be cautious if their answers seem vague, or they can’t specify details about their program.
- Ask about referral fees. If your primary care provider recommends a treatment facility, you can be upfront with them and politely ask if they received any compensation for making the recommendation.
-
Common Therapies for Eating Disorders
Since each individual’s experience with eating disorders is unique, there’s no universal approach to healing. Treatment usually involves steps to get back to a healthy weight and normalize bodily functioning, as well as psychotherapy to address the mental issues that eating disorders can stem from.
Nutritional Counseling
Dietitians or nutritionists who specialize in eating disorders work to understand the nutritional needs and challenges of their patients. From there, they’ll design a plan to help them safely meet those needs. One of their goals is to restore weight to a healthy level. According to The American Dietetic Association, “Medical Nutrition Therapy provided by a registered dietitian trained in the area of eating disorders16 plays a significant role in the treatment and management of eating disorders.”
Psychotherapy
There are several different kinds of psychotherapy (also known as “talk therapy”) used to treat eating disorders. Some common ones include cognitive behavioral therapy (CBT), dialectical behavioral therapy (DBT), and family therapy.
Cognitive Behavioral Therapy (CBT)
CBT teaches you how to change your thought process and beliefs using methodical, repeatable strategies. You can learn to spot when your thoughts around weight and appearance are distorted from reality and attempt to change them. Studies show that the ability to separate the sense of self from an eating disorder17 like anorexia is crucial to recover from it. The effectiveness of CBT is widely noted in the medical community. The Psychiatric Clinics of North America reports, “CBT is the treatment of choice for bulimia nervosa18 and there is evidence that it is as effective with cases of “eating disorder not otherwise specified” (eating disorder NOS), the most common eating disorder diagnosis.”
Dialectical Behavioral Therapy (DBT)
DBT is designed to help you develop practical skills that lead to healthier eating choices. This approach focuses on behavior changes and taking action to bolster your mental health. The skills you learn in DBT include emotional regulation, mindfulness, how to build stronger interpersonal relationships, and distress tolerance. You’re taught to accept your emotions mindfully, and that you are not your emotions. Volatile emotions can exacerbate eating disorder issues, and this type of therapy can help people learn how to regulate them.
Family-Based Therapy (FBT)
Eating disorders can impact the entire family system. FBT opens the door to more effective communication between patients and their family members. It teaches family members that while they may not be responsible for someone’s eating disorder, they can be an important figure in the therapeutic process. It also allows patients to recover with a support system, which can lead to more effective outcomes from therapy. A study conducted by the Stanford University School of Medicine, Lucile Packard Children’s Hospital, and the University of Chicago found that family-based therapy for anorexia is more effective than individual therapy.19
Recovery from Eating Disorders
Struggling, or watching a loved one struggle, with an eating disorder can be anguishing. But it’s important to keep in mind that eating disorders are treatable. With a treatment program fitted to your needs, it’s possible to see significant improvements, and the numbers are promising. A study published in the International Journal of Eating Disorders found that 3 in 4 patients with anorexia nervosa will see levels of improvement following treatment20.
If you’ve determined the need to seek eating disorder treatment, the positive news is there’s a wide variety of plans and programs to choose from. View our directory of rehabs for eating disorders to compare different treatment providers with information like program overviews, pricing, reviews and more.
Reviewed by Rajnandini Rathod