Living with attention deficit hyperactivity disorder (ADHD) often means facing challenges that go beyond attention issues. Many people with ADHD struggle with what experts call executive dysfunction: impairments in the management system in the brain that helps us organize thoughts, prioritize tasks, and follow through on things we start.
The frustration of knowing what needs to be done but struggling to start or complete tasks isn’t a character flaw. It’s a neurological difference in how the ADHD brain processes information and organizes behavior. These invisible barriers can affect everything from your morning routine to your career goals.
Let’s explore the relationship between ADHD and executive function and what practical strategies can make a real difference in your daily life.
What Is Executive Function?
Executive functions1 are the mental skills that help you manage yourself and navigate complex situations. They include abilities like planning ahead, prioritizing, problem-solving, self-regulation, impulse control, and multitasking.
Everyone relies on these skills to handle daily responsibilities and work toward long-term goals. When executive functions are impacted by ADHD, even routine tasks can require a lot more mental effort than they might for others.
ADHD and Executive Dysfunction: The Connection
ADHD and executive dysfunction are closely linked. Most people with ADHD have trouble with executive function skills, though these challenges look different from person to person.
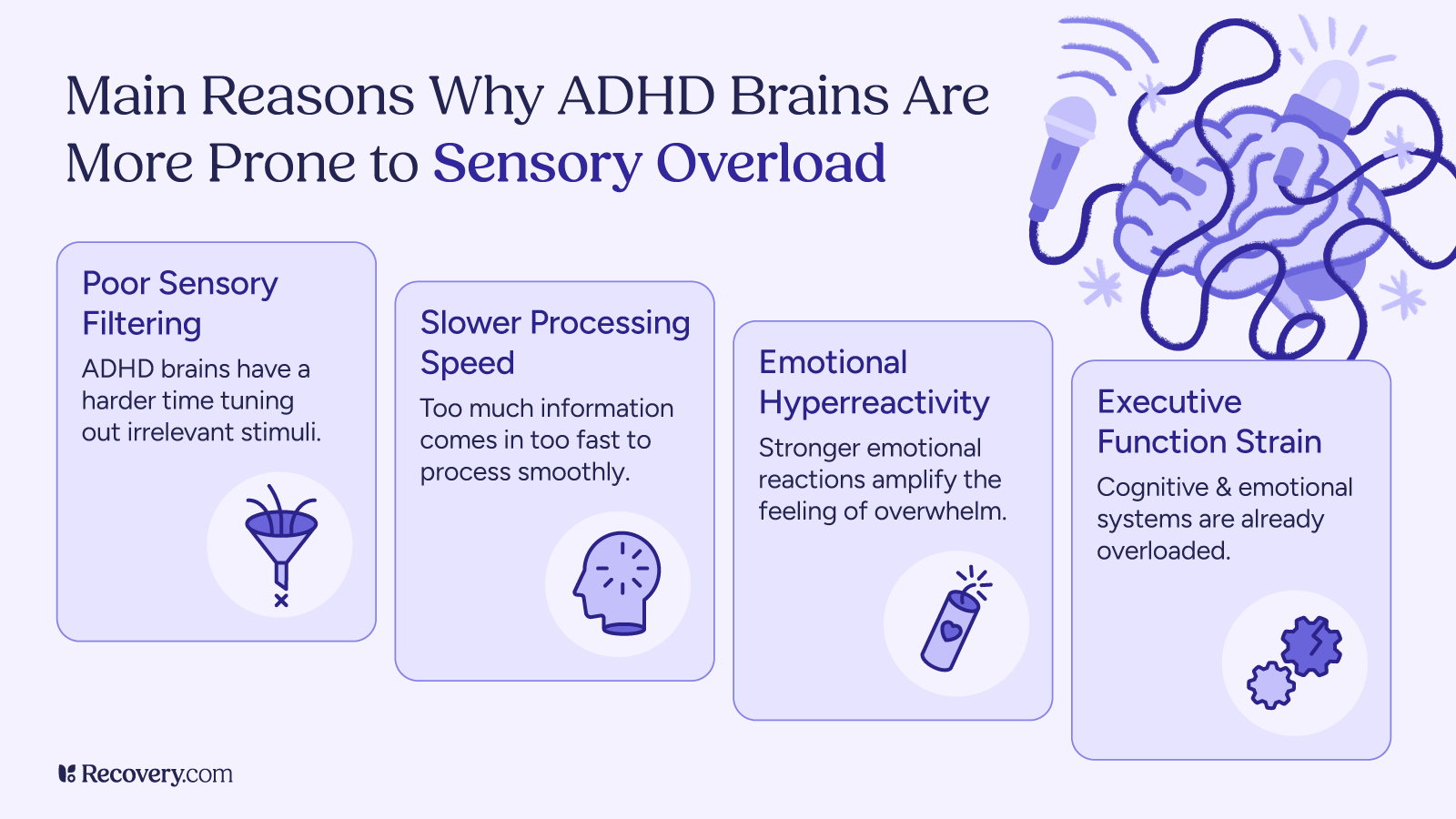
Neuroscience shows that ADHD affects how certain brain areas develop,2 especially parts that help us plan, focus, and control impulses. These brain regions may grow differently or work differently in people with ADHD.
Experts are now acknowledging executive dysfunction as a core symptom of ADHD3 instead of a separate issue. Medication helps some people improve these skills, but most people still need extra strategies to manage daily tasks.
When you understand this connection, it makes sense why addressing only inattention doesn’t solve all ADHD problems. That’s because trouble with starting tasks, keeping track of time, and staying organized comes from the same brain differences that affect attention.
Signs of Executive Dysfunction in ADHD
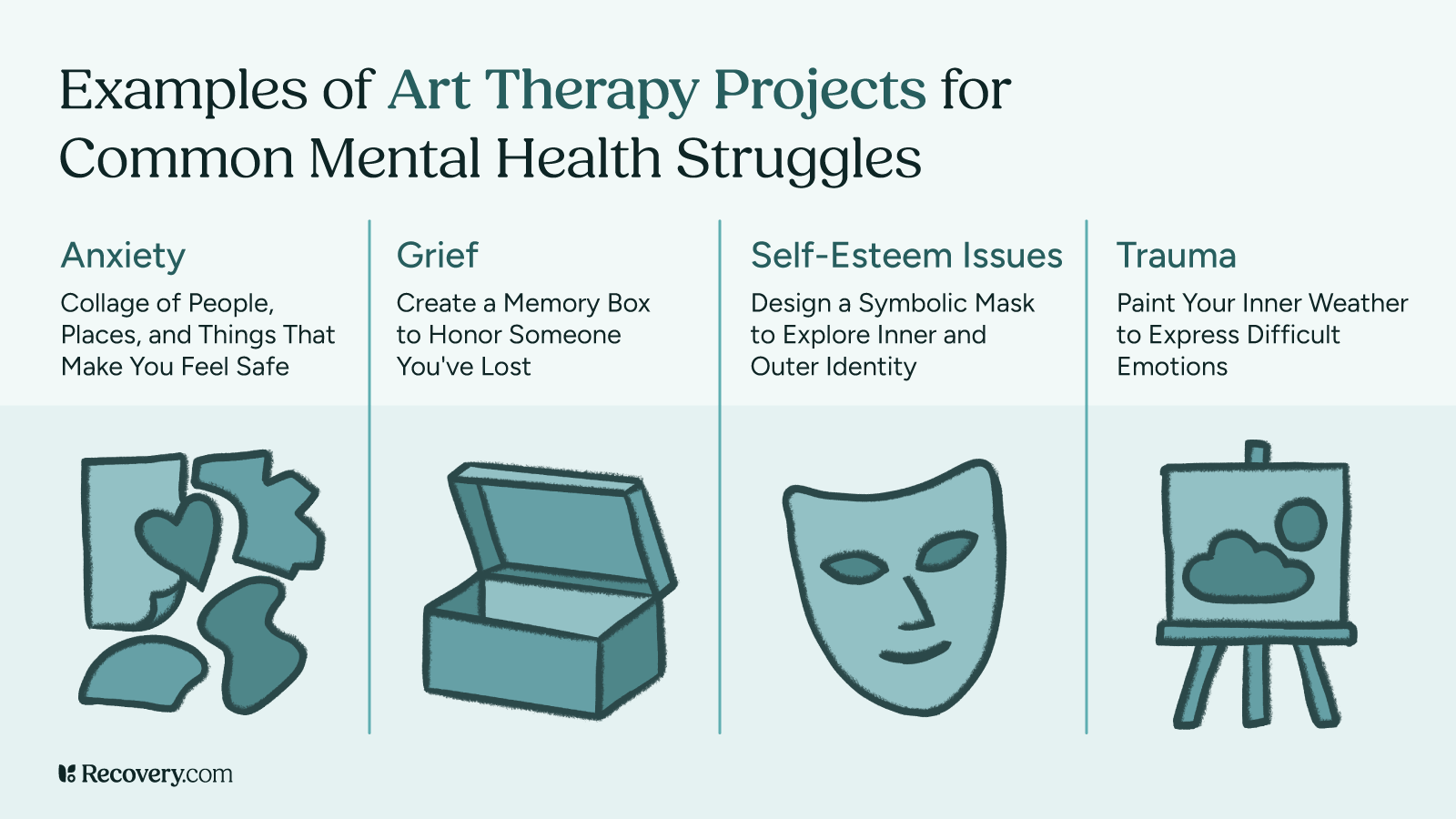
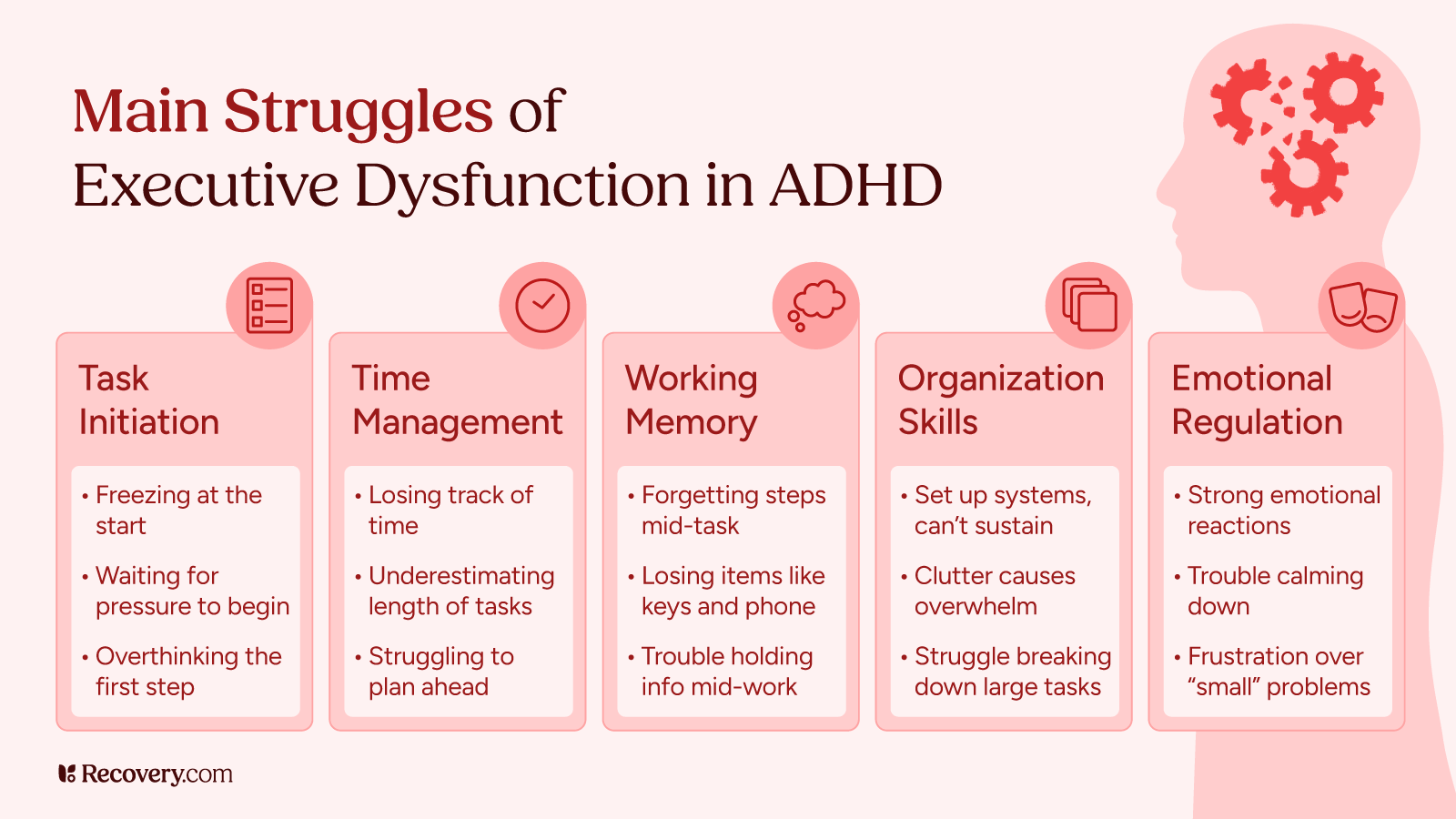
Executive function deficits show up in several ways. You might recognize difficulties in these areas in yourself or someone you care about:
Starting Tasks
- Procrastination: putting off important work until the last minute
- Freezing when you need to start big projects
- Needing extra pressure (like deadlines) to get started
Managing Time
- Always thinking tasks will take less time than they do
- Losing track of time while doing activities
- Finding it hard to plan ahead
Remembering Things
- Forgetting what you were doing in the middle of a task
- Having trouble keeping information in mind while working
- Often misplacing your phone, keys, or wallet
Staying Organized
- Creating systems but struggling to stick with them
- Feeling overwhelmed by messiness or too much information
- Finding it hard to break big projects into smaller steps
Handling Emotions
- Feeling emotions more intensely than others
- Having trouble calming down or regaining self-control when you’re upset
- Getting very frustrated by small problems
The 30% rule for ADHD4 helps explain these challenges. This idea suggests that people with ADHD develop executive skills about 30% more slowly than others. For example, a 30-year-old with ADHD could have executive function abilities similar to a 21-year-old without ADHD. This isn’t about how smart they are—it’s about how certain areas of the brain develop.
How Executive Dysfunction Impacts Daily Life
When executive function skills don’t work well,5 everyday tasks are much harder. This can show up as challenges in several areas of your life:
At Work or School
- Missing deadlines even when you know the work is important
- Trouble following multi-step instructions
- Difficulty switching between different tasks
- Struggling to stay focused in meetings or classes
At Home
- Leaving piles of unfinished projects around the house
- Paying bills late, even when you have the money
- Forgetting things when you shop without a list
- Feeling overwhelmed by household chores
- Forgetting important dates or commitments
- Being late to social events
- Interrupting others in conversation
- Seeming uninterested when your mind wanders
Personal Health
- Forgetting to take medications
- Putting off medical appointments
- Trouble with sleep hygiene
- Finding it hard to stick with exercise routines
These daily challenges can make you feel frustrated or bad about yourself. Many people with ADHD or executive function disorder blame themselves, thinking they’re just lazy or unmotivated. But the reality is that their brains are working differently, which makes these tasks genuinely harder.
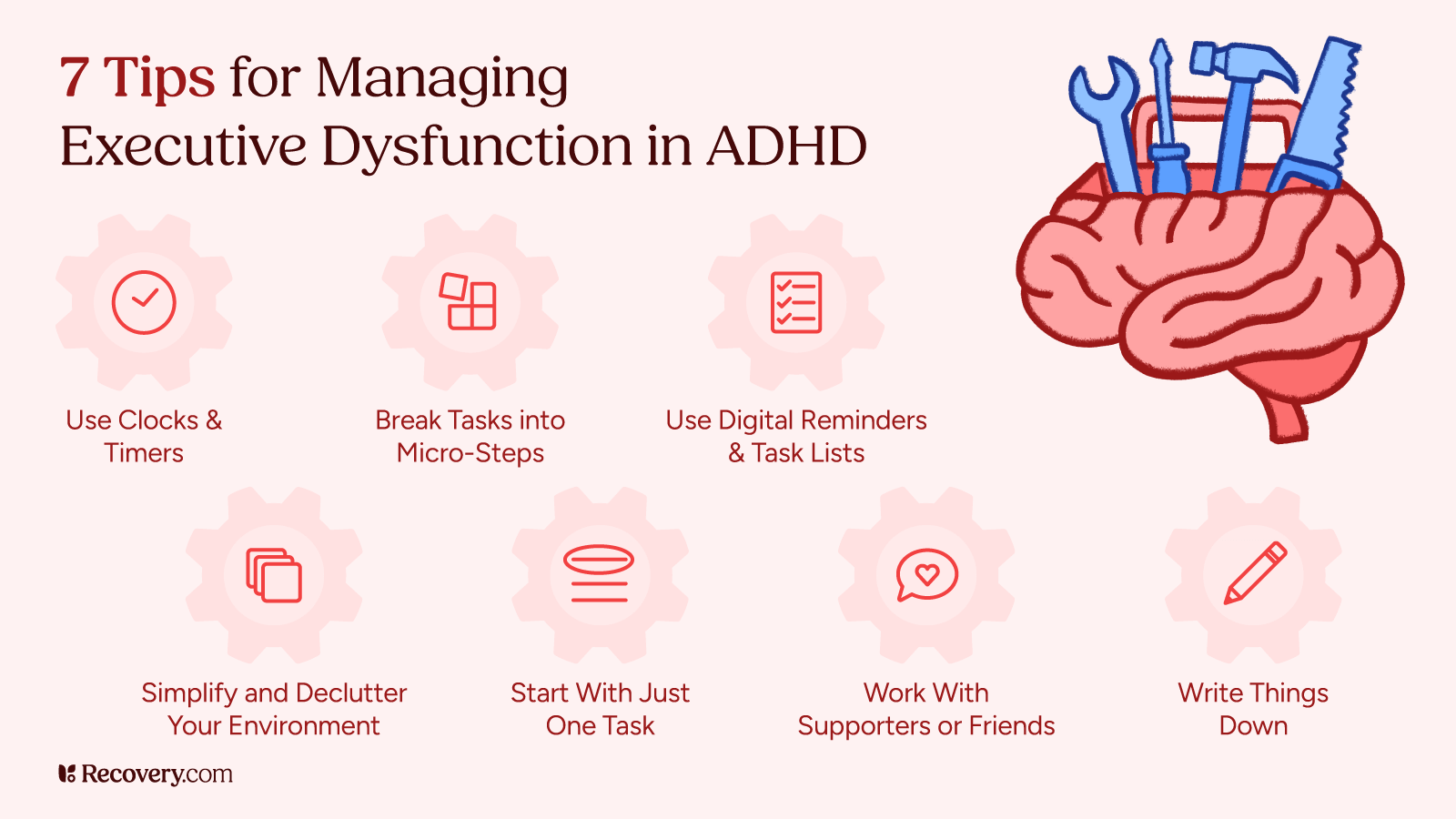
5 Strategies to Improve Executive Function When You Have ADHD
Living well with executive dysfunction means finding strategies that work for your unique brain. Here are some approaches that ADHDers find helpful:
1. Create External Structure
Making time visible can be a game-changer for ADHD brains.6 Try setting a 25-minute timer for focused work sessions. Visual reminders placed where you’ll definitely see them, like sticky notes on the bathroom mirror, can prevent forgotten tasks. Creating simple routines for regular activities, like always putting your keys in the same spot, reduces daily decision fatigue. Breaking tasks into very small steps also helps overcome paralysis—instead of tackling “clean kitchen,” try just “clear counters” as a starting point.
Takeaways:
- Set timers
- Use visual reminders
- Always put things in the same place
- Create simple routines
- Breaking tasks into small steps
2. Use Technology to Your Advantage
Technology can serve as your external brain. Setting multiple alarms for important events ensures backup when your time awareness falters. Apps designed specifically for ADHD7 can break complex tasks into manageable steps and provide helpful reminders. Calendar alerts with specific, detailed reminders work better than vague notes, and digital task managers that send notifications can keep important items from falling through the cracks.
Takeaways:
- Set multiple alarms for important events
- Use ADHD apps and digital task managers
- Use calendar alerts with specific notes
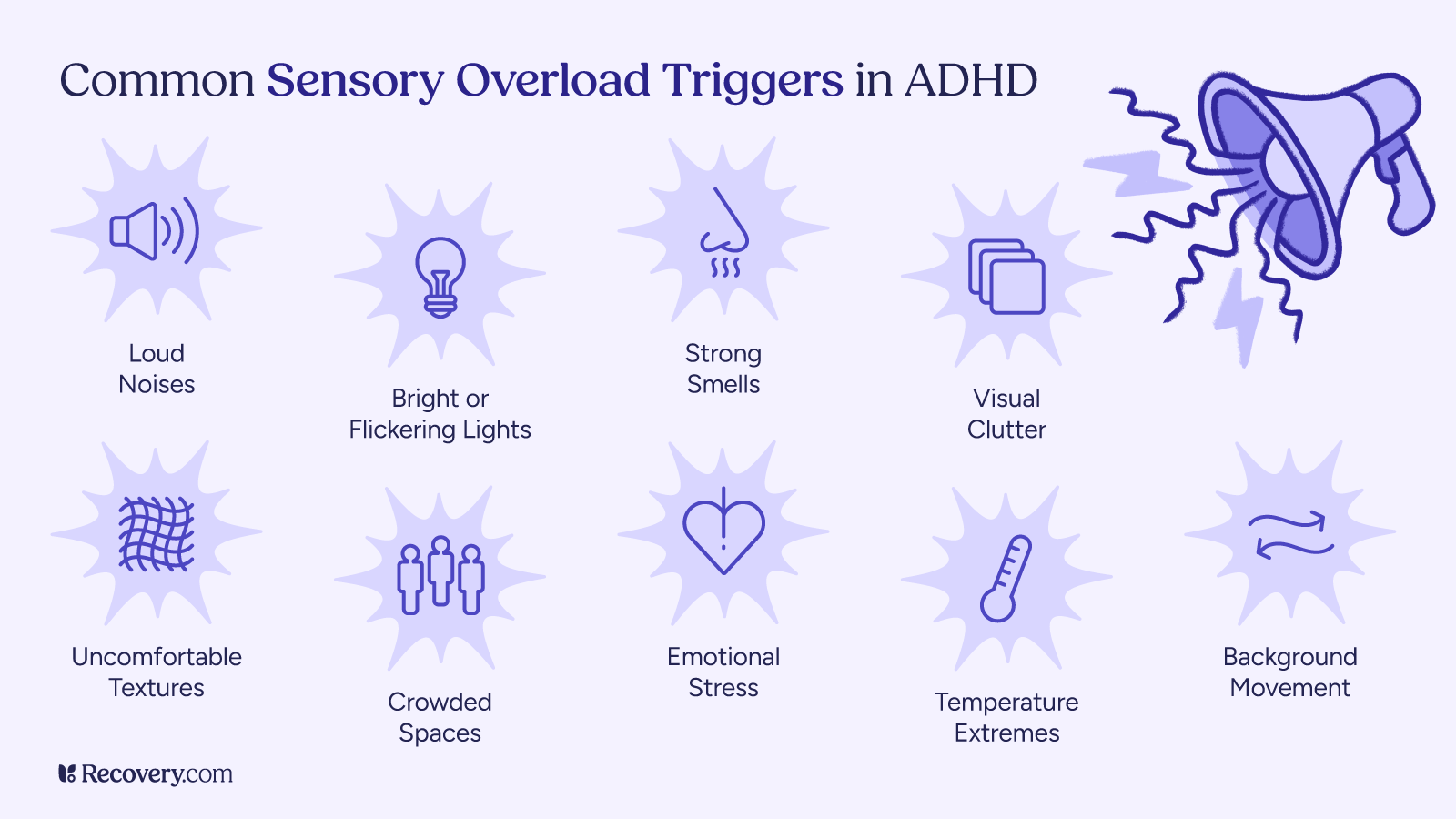
3. Adjust Your Environment
Your surroundings have a major impact on your executive function.8 Reducing distractions in your workspace removes hurdles for your attention. Noise-canceling headphones can help if sounds easily pull your focus away. Consider organizing items by how you use them rather than by category, making functional sense for your daily needs. Making important items more visible through clear containers or open shelving prevents the “out of sight, out of mind” problem.
Takeaways:
- Minimize distractions in your space
- Use noise-canceling headphones
- Organize items by how you use them
- Make sure important items are easily visible
4. Use Body-Based Techniques
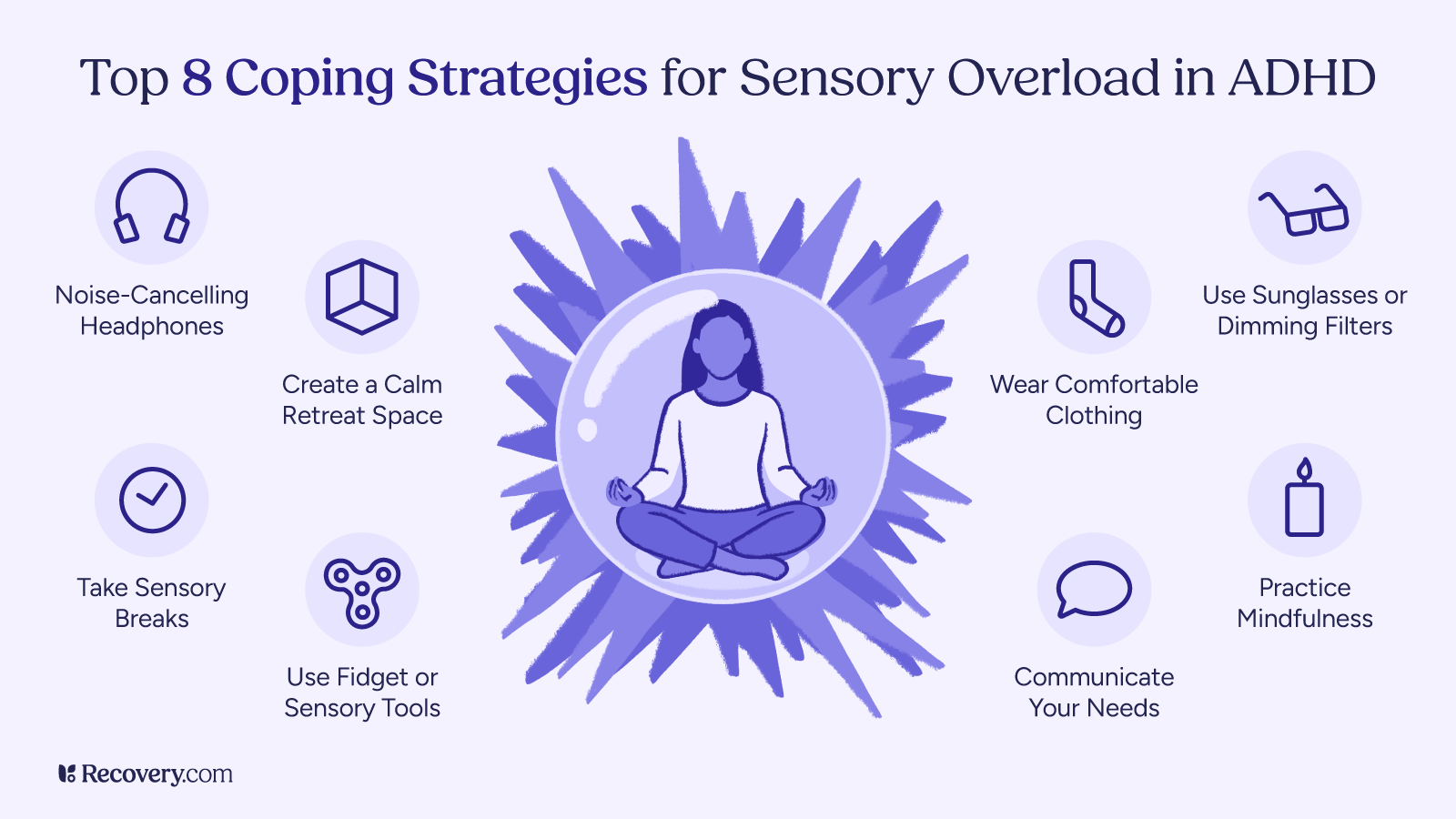
Physical strategies can also help. Regular exercise improves focus and cognitive function9 for many people with ADHD. Proper sleep improves your decision-making and makes a dramatic difference in your ability to manage symptoms of executive dysfunction. Some people find that fidget toys help them stay more focused during meetings or conversations. And short breaks for movement can reset your attention when you feel your focus drifting.
Takeaways:
- Aim to get regular sleep and exercise
- Use fidget toys in situations where you have to sit still
- Take mini movement breaks
5. Ask for Social Support
Let your loved ones know how they can communicate most helpfully with you. If verbal directions tend to evaporate from your memory, ask for written instructions. If you struggle with focus while working, try working alongside someone who quietly works near you. Share your goals with a friend and have regular check-ins to increase your accountability.
For even more structured support, an ADHD coach or accountability partner can provide consistent guidance that’s tailored to your specific challenges.
Takeaways:
- Ask for written instructions
- Work next to someone who’s working quietly
- Enlist an accountabilabbuddy to help you stay on track
- Hire an ADHD coach for structured support
You may need to experiment with different approaches until you find what helps you function best. The most effective strategies are the ones that address your specific challenges, and that you will actually consistently use.
Treatment Options for Executive Dysfunction
Self-help strategies can help you manage executive dysfunction, but they’re even more powerful when combined with professional treatment. These options are commonly used to treat ADHD executive dysfunction:
Psychiatry (Medication)
Medication is often the first line of treatment for ADHD, and many people find it helps with issues related to executive function. Stimulant medications like Adderall, Ritalin, and Vyvanse show positive results for about 70-80% of people with ADHD,10 as they help with focus, task initiation, and working memory. There are also non-stimulant options like Strattera for those who don’t respond well to stimulants or have unwanted side effects.
The effects of medication vary from person to person. Finding the right ADHD medication and dosage usually means working closely with your prescribing doctor to find what works best for you.
Helpful Therapies for Strengthening Your ADHD Executive Skills
Several therapy approaches can help build executive function skills.
- Cognitive behavioral therapy (CBT) teaches practical ways to manage ADHD challenges through changing thought patterns and developing concrete strategies.
- ADHD coaching focuses on real-world applications, helping you create systems that work with your natural brain function to accomplish goals and manage daily responsibilities.
- Occupational therapy offers specialized help with organization and time management skills through hands-on techniques.
- Mindfulness practices, including meditation and simple breathing exercises, can improve your focus and make it easier to control impulses.
- Working memory training programs: Special games and exercises can strengthen your ability to hold information in mind while working on tasks.
- Psychoeducation: Learning about how ADHD affects your brain helps you understand your challenges and find strategies that actually work for you.
When to Seek Professional Help
Professional help becomes essential when executive dysfunction significantly impacts your quality of life, affecting your work, relationships, or emotional well-being. If you’re diligently trying strategies on your own but still struggling to manage day-to-day tasks, expert guidance can make a big difference.
It’s especially important to reach out if your feelings of frustration or sadness about ADHD become overwhelming or start causing anxiety or depression. A mental health professional can help if you feel lost among all the possible approaches, steering you toward the right combination of interventions for your needs.
Many people find they benefit most from a combination of medication, therapy, and self-help strategies.
How to Be an Ally: Supporting Someone With Executive Dysfunction
It’s all of our job to educate ourselves on mental health conditions to create safer spaces for those around us. If someone you love has ADHD and executive dysfunction, your support can make a big difference.
Understanding Helps
Learning about ADHD and executive function helps you recognize these challenges as real neurological differences, not excuses. Understanding grows patience when you realize tasks that seem simple to you might be genuinely difficult for someone with executive dysfunction.
Practical Support
Offer clear, written instructions for complex tasks and help break down projects into smaller steps. Create organizational systems together rather than imposing your own. Gently reminding your ADHD friend without criticism can provide the external cue their brain needs.
Emotional Support
Celebrate small wins and avoid comparing your loved one to people without an attention deficit disorder. Be patient during tough moments and focus on their strengths, not just the challenges.
Workplace Support
Advocate for accommodations like written instructions and distraction-free workspace options to support your neurodivergent coworkers.11 When we learn to recognize the unique perspectives that often come with adult ADHD and other forms of neurodiversity (such as autism/autism spectrum disorder) as valuable assets, everyone thrives.
Get Help to Build a Life That Works With Your ADHD Brain
Executive dysfunction in ADHD presents some real challenges, but with understanding and the right strategies, these obstacles can become manageable. It may take some time and patience to find what works for your unique brain.
Instead of forcing yourself to fit into systems designed for neurotypical brains, success often comes from creating approaches that work with your natural strengths. Professional support can help you create a life that accommodates your executive function differences while still achieving your goals.
Use our search tool to find ADHD treatment programs that match your needs and connect directly with a specialist today.
FAQs
Q: How do you know if you have executive dysfunction?
A: Signs include trouble starting tasks, poor time management, difficulty organizing, problems with working memory, and emotional regulation challenges. If these issues significantly impact your daily life, consider talking to a healthcare provider about assessment.
Q: Does ADHD always cause executive dysfunction?
A: Most people with ADHD experience some degree of executive function challenges, though they vary in type and severity. Executive dysfunction is considered a core feature of ADHD, not a separate condition.
Q: What is the 30% rule for ADHD?
A: The 30% rule suggests that people with ADHD develop executive skills about 30% more slowly than their peers. This helps explain why adults with ADHD might struggle with skills that others their age have mastered.
Q: Can therapy help with executive dysfunction in ADHD?
A: Yes, several therapy approaches can help, including cognitive behavioral therapy (CBT), ADHD coaching, and occupational therapy. These treatments teach practical skills and strategies to manage executive function challenges.
Q: How can someone with ADHD improve their executive function?
A: Improvement comes through a combination of understanding your challenges, creating supportive environments, using tools and technology, establishing routines, and possibly taking medication. Professional support often helps this process.