Seeing a loved one struggle with addiction can be extremely difficult. Addiction has a huge impact on the person experiencing it. It can also affect the mental health of loved ones, and put a strain on their entire community.
You want to help as best as you can. You may have already looked into rehabs near you, but found that your loved one resisted. This isn’t uncommon. Remember that they are in a delicate place. While they may be ready to accept some help, the idea of going through treatment can seem daunting. At the same time, their behaviors can impact your mental well-being. You deserve healing too.
If your loved one is reluctant to seek treatment, you might wonder if you can do anything to get them into rehab. And the short answer is yes: there are a number of ways you can help.
- How can you help someone who has an addiction problem?
- Can I force my loved one to go to rehab?
- How does a person qualify for mandatory rehab?
- In what states can you force someone into rehab?
- Will my loved one face legal consequences if they go to forced rehab?
Involuntary Rehab for Different Family Members
Efficacy Rates and the Treatment Experience
General Questions
How Can You Help Someone with an Addiction Problem?
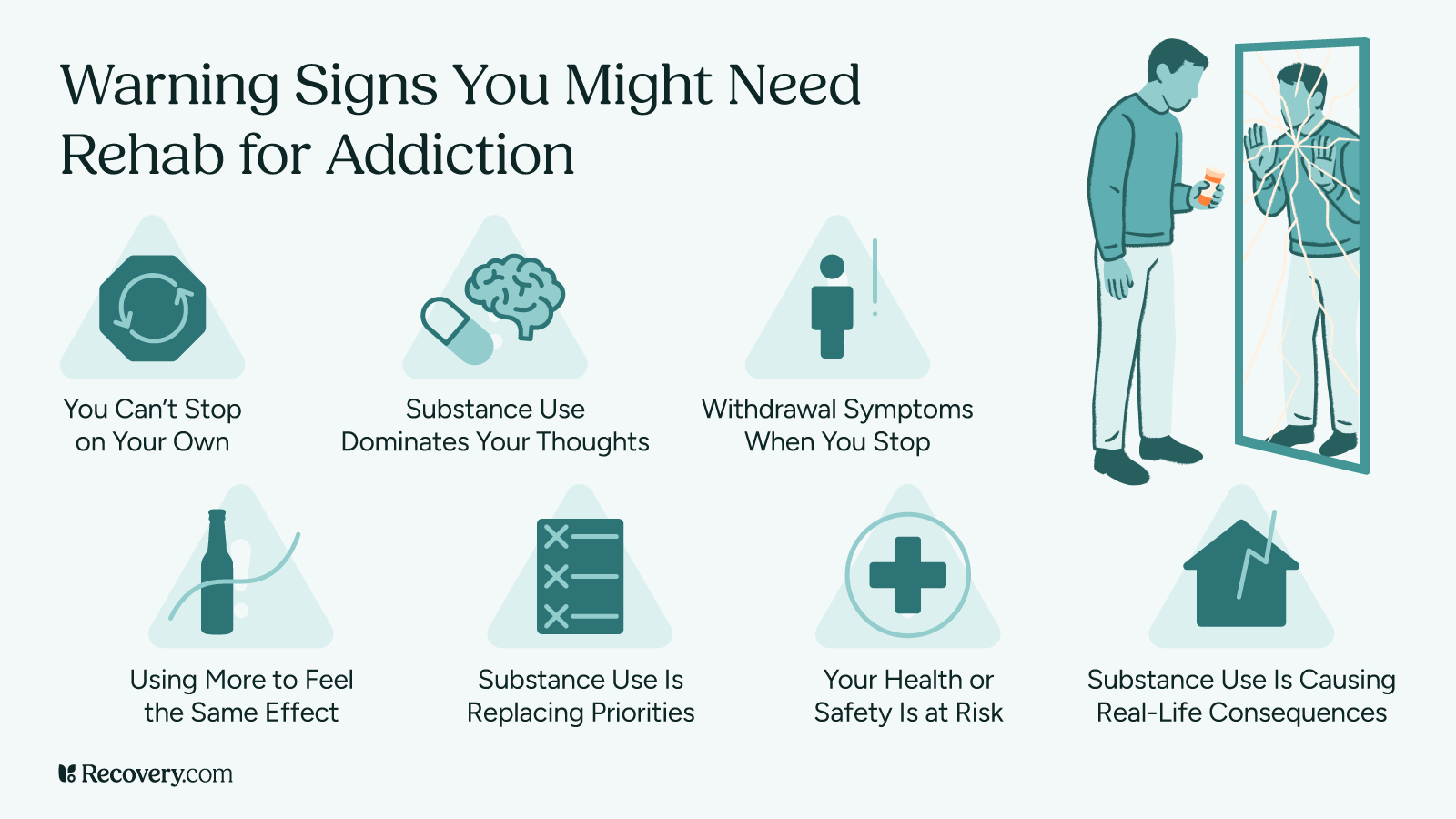
There are several ways to help someone struggling with addiction. But before you make a plan, there are some factors you should keep in mind. You can start by answering the following questions:
- How severe is their addiction?
- Will they need help detoxing?
- Are they open to receiving treatment?
- What is your relationship with them like now? Even if you were close in the past, addiction can isolate people from their loved ones.
Just offering to help can be effective. People are more likely to recover from addiction ((Bartlett, R., Brown, L., Shattell, M., Wright, T., & Lewallen, L. (2013). Harm reduction: Compassionate care of persons with addictions. Medsurg Nursing : Official Journal of the Academy of Medical-Surgical Nurses, 22(6), 349–358. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4070513/)) with the support of a loved one.
Communication is the first step. But it can be difficult to know exactly what to say or how to say it. Talking to someone about getting treatment requires compassion, empathy, and honesty. This conversation might be a painful one, and that’s okay. Stay focused on your goal of getting them the help they need.
If your loved one is at risk of harming themselves, or they refuse to get help, it may be time to stage an intervention. Sometimes, this means using the Community Reinforcement and Family Training (CRAFT) intervention model. ((An underappreciated intervention. (n.d.). Https://Www.Apa.Org. Retrieved June 30, 2022, from https://www.apa.org/monitor/2017/12/underappreciated-intervention))
In the CRAFT model, a therapist teaches you how to encourage a person to enter treatment. You’ll learn to reward your loved one’s positive behaviors without reinforcing unhealthy ones. CRAFT can also teach you to care for yourself and regain control of your life.
If they agree to get help, they may or may not benefit from residential rehab. Data shows that some people with less severe addictions respond well to talk therapy. ((Bartlett, R., Brown, L., Shattell, M., Wright, T., & Lewallen, L. (2013). Harm reduction: Compassionate care of persons with addictions. Medsurg Nursing : Official Journal of the Academy of Medical-Surgical Nurses, 22(6), 349–358. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4070513/))
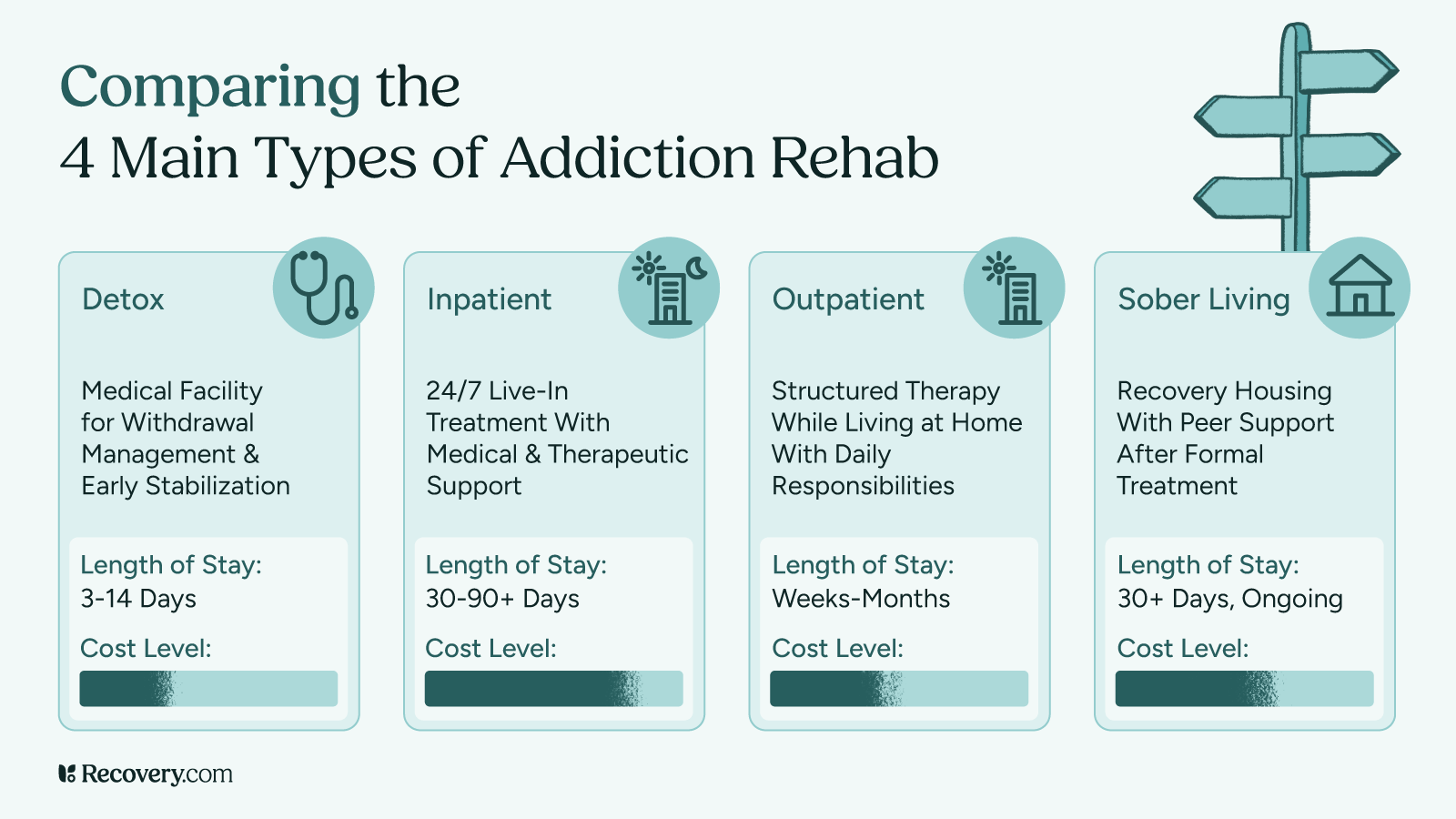
If your loved one’s struggle with addiction is more severe, you may consider a treatment program. The good news is, substance use disorder can be treated. ((Early intervention, treatment, and management of substance use disorders. US Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424859/)) And, recovery rates are higher at rehabs with comprehensive continuing care programs.
Can I Force My Loved One to Go to Rehab?
If your loved one needs treatment but has refused to get it, you may be wondering if you can force them into rehab. You can, but only in certain states.
Some form of involuntary treatment is allowed in 47 states and the District of Columbia. ((Fuller, D., & Pinals, D. (n.d.). Assisted Outpatient Treatment (AOT) Community-Based Civil Commitment. National Initiative to Improve the Court and Community Response to Mental Illness. Retrieved June 30, 2022, from https://www.ncsc.org/__data/assets/pdf_file/0026/16964/mhf2-assisted-outpatient-treatment-jan-2020.pdf)) Connecticut, Maryland and Massachusetts are currently the only states where you can’t commit a loved one to treatment. Make sure to check your area’s regulations before taking any action. The exact laws vary from state to state, and can change over time.
In many areas, a person needs to meet certain requirements to qualify for mandatory rehab. ((State Standards for Initiating Involuntary Treatment. (2020). Treatment Advocacy Center. https://www.treatmentadvocacycenter.org/storage/documents/state-standards/state-standards-for-initiating-involuntary-treatment.pdf)) These requirements also vary between U.S. states. Generally, you will need to prove that a person is in the middle of a crisis or is currently addicted to substances.
This process can also change depending on your loved one’s exact health concerns. Some states have different requirements for people with addictions and mental health issues. Others even distinguish between alcohol and drug addictions. And some even have one set of rules for current patients, and another for people who are new to treatment.
These policies can be hard to navigate. Before you start this process, make sure you know exactly which laws apply to your situation. Once you get the ball rolling, it can be hard to control what comes next. The more you plan, the more likely you are to get the best possible result.
How Does a Person Qualify for Mandatory Rehab?
A person must meet specific criteria to qualify for involuntary treatment. ((State Standards for Initiating Involuntary Treatment. (2020). Treatment Advocacy Center. https://www.treatmentadvocacycenter.org/storage/documents/state-standards/state-standards-for-initiating-involuntary-treatment.pdf)) These criteria vary by state.
Most states require proof that a person is actively using drugs or alcohol. They may also need evidence from a psychology expert that the person is a danger to themselves or others. ((Saya, A., Brugnoli, C., Piazzi, G., Liberato, D., Di Ciaccia, G., Niolu, C., & Siracusano, A. (2019). Criteria, procedures, and future prospects of involuntary treatment in psychiatry around the world: A narrative review. Frontiers in Psychiatry, 10, 271. https://doi.org/10.3389/fpsyt.2019.00271)) Additionally, many states have separate processes for evaluating those in a mental health crisis and current patients.
Usually, anyone can ask for another person to get evaluated for involuntary care. But that isn’t always the case. In California and Florida, the request needs to come from a designated professional. This might mean the member of a crisis team, a physician, or a social worker.
The first step is filing a petition for evaluation. Next, a qualified expert will perform the assessment. In some states, that expert must be associated with a treatment center. Others allow psychologists, psychiatrists, and addiction counselors to facilitate this process.
Which States Let You Send Someone to Involuntary Treatment?
Most U.S. states allow for 3 forms of involuntary rehab: ((Fuller, D., & Pinals, D. (n.d.). Assisted Outpatient Treatment (AOT) Community-Based Civil Commitment. National Initiative to Improve the Court and Community Response to Mental Illness. Retrieved June 30, 2022, from https://www.ncsc.org/__data/assets/pdf_file/0026/16964/mhf2-assisted-outpatient-treatment-jan-2020.pdf))
- In an emergency evaluation, or psychiatric hold, someone is admitted to a hospital in crisis. In most states, they can be held for a maximum of 72 hours. During that time they’ll undergo a thorough evaluation.
- Inpatient civil commitment is a legal intervention. This occurs after a person meets their state’s criteria for civil commitment. Then, a judge can order them to undergo inpatient treatment. Even if they do meet all local criteria, this decision is in the judge’s hands.
- Outpatient civil commitment is also known as assisted outpatient treatment, or AOT. This is court-ordered outpatient treatment for qualifying people with mental health issues. Criteria to qualify for AOT civil commitment ((State Standards for Initiating Involuntary Treatment. (2020). Treatment Advocacy Center. https://www.treatmentadvocacycenter.org/storage/documents/state-standards/state-standards-for-initiating-involuntary-treatment.pdf)) vary by state.
If you or someone you know is suffering a mental health crisis and may be a danger to themselves or others, you should call 911.
If you call 911, you can request a Crisis Intervention Trained (CIT) officer with special training in mental health emergencies. A CIT officer may or may not be available to help, but you can always ask.
Will My Loved One Face Legal Consequences?
It depends, but it’s possible.
In some cases, court-ordered rehab is available as an alternative to jail time. This is only available in certain states, and the case has to meet specific criteria:
- The charges are non-violent.
- The defendant is eligible for parole.
- The charge is no more serious than a 3rd-degree felony.
- The defendant has no history of violence.
- The defendant has no history of sexual assault.
If your loved one is in possession of certain drugs—like cannabis, in certain states—they won’t face charges. But the possession of other substances can have serious consequences. As more municipalities decriminalize drug possession, ((Oregon’s drug decriminalization may spread, despite unclear results. (n.d.). Retrieved June 30, 2022, from https://pew.org/3pYDLxY)) these rules may change rapidly.
Court-ordered rehab doesn’t necessarily protect them from criminal charges. For instance, if they fail to complete court-ordered treatment, they may face fines or even jail time.
Legal consequences can be a barrier to some kinds of treatment. But this shouldn’t stop you from asking for help. If you’re concerned about what will happen if you send a person to involuntary drug rehab, reach out to a lawyer. They’ll be able to walk you through your state’s options and advise you on what to do next.
Getting Treatment for a Family Member
Can I Send My Teen to Rehab?
You may be able to send your child to rehab depending on your location and their age.
Different states have different legal requirements for minor consent to involuntary rehab. ((Kerwin, M. E., Kirby, K. C., Speziali, D., Duggan, M., Mellitz, C., Versek, B., & McNamara, A. (2015). What can parents do? A review of state laws regarding decision making for adolescent drug abuse and mental health treatment. Journal of Child & Adolescent Substance Abuse, 24(3), 166–176. https://doi.org/10.1080/1067828X.2013.777380)) In Washington state, for example, parents can initiate treatment for teens at a behavioral health treatment facility without the minor’s consent. ((Age of consent for behavioral health treatment in Washington. (2018). Washington State Health Care Authority. https://www.hca.wa.gov/assets/program/fact-sheet-age-consent-behavioral-health-treatment.pdf)) A minor in Washington is considered someone who is 13 to 17 years old.
The consent laws for teens vary from state to state, much as they do for adults. But it might be easier to send your teen to rehab for mental health issues than for addiction. And more states give parents authority over inpatient treatment compared to outpatient care.
In some states, parents need to prove they’ve exhausted all other treatment options before sending a teen to rehab against their will. And in most areas, parents need to prove their teen is a danger to themselves or others if they don’t get treatment.
Can I Send My Spouse to Rehab?
You can send your spouse to rehab in certain states.
Some states allow any interested persons, including a spouse, to petition for inpatient or outpatient commitment of a loved one. For example, this is the case in Mississippi, South Carolina, and Louisiana. Because specifics still vary widely depending on your location, it’s best to check your state’s regulations on involuntary commitment. ((State Standards for Initiating Involuntary Treatment. (2020). Treatment Advocacy Center. https://www.treatmentadvocacycenter.org/storage/documents/state-standards/state-standards-for-initiating-involuntary-treatment.pdf))
Some states let anyone, including a spouse, petition for someone else to get involuntary treatment. For example, this is the case in Mississippi, South Carolina, and Louisiana. However, the specific regulations vary widely depending on your location. Learn more about the local mental health treatment regulations ((State Standards for Initiating Involuntary Treatment. (2020). Treatment Advocacy Center. https://www.treatmentadvocacycenter.org/storage/documents/state-standards/state-standards-for-initiating-involuntary-treatment.pdf)) before you take action.
In some situations, you won’t have the time to do research. And by the time you’re thinking about mandatory rehab, you might already be in crisis. In many areas, anyone can request an emergency psychological evaluation for someone else. You can usually do this in response to a mental health crisis, including a crisis caused by substance use.
If you or someone you know is a danger to themselves or others, get yourself to safety and call 911.
If your spouse is putting you in physical danger, get yourself to safety FIRST. You can contact the National Domestic Violence Hotline at 1.800.799.SAFE (7233) if you need help.
Efficacy Rates and the Treatment Experience
Do Interventions Work?
Interventions may work with the help of a professional interventionist.
There aren’t many studies on the effectiveness of interventions. But limited data suggests that interventions can be successful when led by professionals. ((Nededog, J. (n.d.). Here’s why reality show “Intervention” has a higher success rate than most rehab programs. Business Insider. Retrieved June 30, 2022, from https://www.businessinsider.com/ae-intervention-success-rate-data-2015-8))
Professional interventionists often have an educational background in psychology or social work. Exact education requirements vary by state. But for the most part, these experts are trained to teach you about addiction, rehab, and recovery. Many interventionists are in recovery themselves. This gives them a unique level of empathy for both your and your loved one’s experience.
If you hire a professional to help you stage an intervention, they’ll help you prepare for days or weeks in advance. These events usually include a group of people close to the person with addiction. When you’re ready, you’ll all sit down together to discuss the impact of your loved one’s substance use. Usually, the goal is to encourage the person to seek treatment.
A strong community can impact someone’s decision to seek treatment. In a 2019 study of soldiers who decided to seek addiction treatment, ((Black, K., Britt, T., Zinzow, H., Pury, C., Cheung, J. (2019). The Role of Social Support in Treatment Seeking Among Soldiers. Occupational Health Science. 3. 10.1007/s41542-019-00044-2. Retrieved June 30, 2022, from https://www.researchgate.net/publication/334269504_The_Role_of_Social_Support_in_Treatment_Seeking_Among_Soldiers)) social support was “rated as most influential to that decision.”
Is Forced Rehab Effective?
Experts have diverse opinions on the effectiveness of forced rehab. ((Werb, D., Kamarulzaman, A., Meacham, M. C., Rafful, C., Fischer, B., Strathdee, S. A., & Wood, E. (2016). The effectiveness of compulsory drug treatment: A systematic review. The International Journal on Drug Policy, 28, 1–9. https://doi.org/10.1016/j.drugpo.2015.12.005)) Some argue that it doesn’t help people recover. Others state that forced treatment is just as effective ((Is legally mandated treatment effective? National Institute on Drug Abuse. https://nida.nih.gov/publications/principles-drug-abuse-treatment-criminal-justice-populations-research-based-guide/legally-mandated-treatment-effective)) as voluntary treatment.
According to a 2016 analysis, nearly 75% of studies find no improvement in mandatory rehab. ((Werb, D., Kamarulzaman, A., Meacham, M. C., Rafful, C., Fischer, B., Strathdee, S. A., & Wood, E. (2016). The effectiveness of compulsory drug treatment: A systematic review. The International Journal on Drug Policy, 28, 1–9. https://doi.org/10.1016/j.drugpo.2015.12.005)) But this research has some limitations. Because states have such different laws, the definition of “mandatory” is far from universal.
In states where court-ordered rehab is an alternative to jail time, some rehabs resemble detention centers. Many of these programs don’t offer evidence-based treatment. They also often lack proper detox facilities for those who may need it. In these areas, experts say we should focus on removing barriers to care. This would be a more effective solution than mandatory treatment. ((Poser, R. (n.d.). Does forced rehab work? Mother Jones. Retrieved June 30, 2022, from https://www.motherjones.com/politics/2018/06/does-forced-rehab-work/))
There are some cases of successful recovery following forced addiction treatment. According to the National Institute on Drug Abuse, outcomes for people who attend court-ordered rehab ((Is legally mandated treatment effective? National Institute on Drug Abuse. https://nida.nih.gov/publications/principles-drug-abuse-treatment-criminal-justice-populations-research-based-guide/legally-mandated-treatment-effective)) are just as effective as they are for people who seek treatment voluntarily.
How Long Does Mandatory Rehab Last?
This depends on a few factors, including your location and your loved one’s mental health status.
If someone is in the midst of a mental health crisis, they may be held for up to 72 hours during an emergency evaluation. This is also called an involuntary hold. Each state has their own set of guidelines regarding the length of an involuntary hold. ((Know the laws in your state—Treatment advocacy center. (n.d.). Retrieved June 30, 2022, from https://www.treatmentadvocacycenter.org/component/content/article/183-in-a-crisis/1596-know-the-laws-in-your-state))
During this time, an expert evaluates the person to see if they need further treatment. If so, they may be held for up to 2 weeks in most states. If they need further treatment after that time, they may attend inpatient rehab.
My Loved One Won’t Go to Rehab: How Can I Help?
Involuntary rehab is often the last resort for families who have tried all other avenues. If your loved one refuses to get help, it’s your job to care for yourself. You may need to set boundaries, or focus on your own mental health. Remember that you also deserve to heal.
There are many mutual support groups for people impacted by addiction. Most of these groups are free, open to anyone with a commitment to healing. You can find in-person groups in most areas, and online meetings are accessible from anywhere. These of the best-known groups for loved ones:
- Al-Anon is for adults who love someone with an addiction.
- Alateen is like Al-Anon, but for teens.
- Codependents Anonymous, or CoDA is for anyone with codependency, whether or not you have a loved one with addiction.
These groups follow the 12-Step model of recovery. They are peer-led, with a focus on fellowship and mutual support. If 12-Step groups aren’t right for you, you can look for other support groups in your area. And whether or not you join a group, you might benefit from seeing a 1:1 talk therapist.
If your loved one does agree to attend rehab, finding a program can be daunting – not just for them, but for your whole family. Visit our directory of addiction rehab centers to learn about treatment options, including detox services, pricing, and family therapy programs.
Reviewed by Rajnandini Rathod