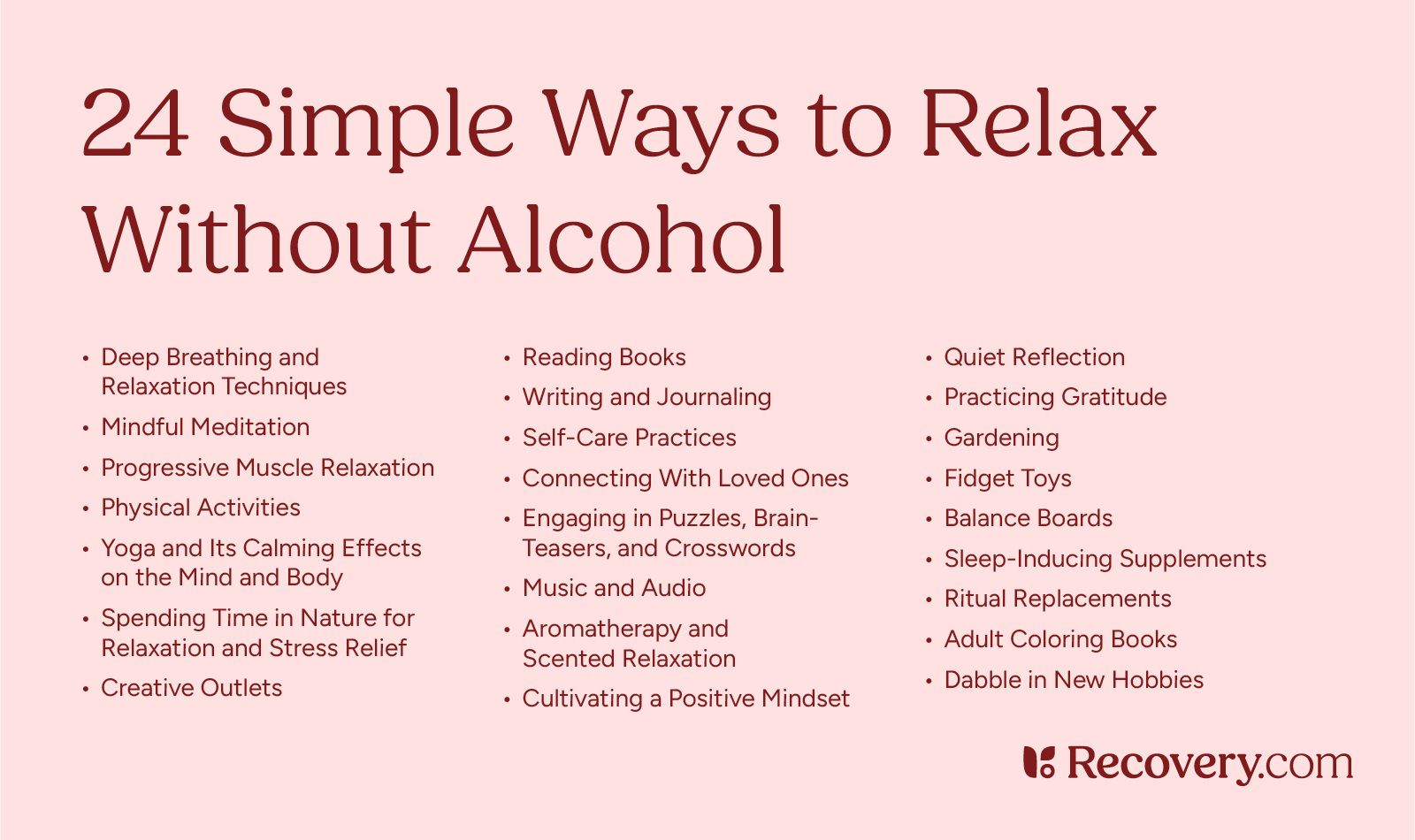
Relaxing without alcohol is entirely achievable by exploring healthier and more fulfilling alternatives. From engaging in physical activities like yoga and walking to practicing mindfulness through meditation or journaling, there are countless ways to unwind. Creative hobbies, such as painting or playing music, and social connections, like spending quality time with friends or joining a club, can also bring relaxation and joy. These alternatives not only reduce stress but also promote long-term well-being, proving that relaxation doesn’t have to come in a glass

1. Deep Breathing and Relaxation Techniques
In moments of stress, breathing is powerful. Data shows that breath control has huge benefits,1 both physically and psychologically.
Deep breathing techniques,2 in particular, can help your body relax. These practices stimulate your relaxation response, which has a direct effect on your physical health. Experts say deep breathing can stabilize your blood pressure, and may even improve immune system activity. Deep, diaphragmatic breathing3—or, belly breathing—can also reduce stress and negative emotions. It may even improve your attention span.
Here’s one technique you can try:
Rest your hand on your belly as you take slow, deep breaths in and out. Notice how it feels to breathe, both in your lungs and as your breath moves your hand. Continue this exercise for as long as you like. Try to observe your own experience without judgment.
2. Mindful Meditation
For many people, mindful meditation is an essential part of recovery4 from alcohol addiction. Meditating regularly can relieve depression and anxiety, help with cravings, and lower your risk of relapse.
Mindful meditation can take many forms. For instance, you can sit quietly with your eyes closed and focus on your breath. But that technique doesn’t work for everyone. You can also look around and take note of your environment, or pay attention to how your body feels while you go for a walk. Some people meditate in groups, sharing their experiences in daily or weekly sessions. Many people who are new to meditation find it helpful to use guided meditations or guided imagery. You can think of meditation as a therapeutic coping mechanism, a spiritual practice, or anything else that works for you.
3. Progressive Muscle Relaxation
You can use progressive muscle relaxation (PMR) for physical and emotional symptoms.5 This technique can treat many health issues, including anxiety, bipolar disorder, insomnia, headaches, and muscle pain. You can learn PMR from a trained healthcare provider, or try it on your own.
You’ll start by sitting or lying in a comfortable position. Then you’ll tense a single muscle or muscle group, bringing your attention to that area. It’s important to keep breathing, and not tense your muscles so much you injure yourself. Sometimes just a little tension is enough. Next, you’ll slowly release the tension and notice how it makes you feel, both physically and emotionally. You can repeat this process with muscles anywhere in your body. PMR sessions normally last 10-15 minutes.

4. Physical Activities
If you’re wondering how to take the edge off without alcohol, physical activities are a great place to start. Any type of aerobic exercise reduces alcohol cravings.6 Just moving your body and increasing heart rate can make a big difference right away.
Working out can also help over longer periods of time. Some data shows that the more you exercise, the less you’ll crave alcohol7 or drugs. That’s partly because exercise increases dopamine production.
Dopamine is a naturally occurring neurochemical that allows you to feel a sense of accomplishment. Addiction affects dopamine,8 and regulating this neurotransmitter is a very important part of healing. Regular exercise doesn’t only improve your physical health; it also helps your mind relax and recover.
Exercise isn’t accessible to everyone, but there are countless ways to engage your body. If you’re still recovering from the physical impact of addiction, you might need to move slowly at first. Talk to your doctor about which types of physical activity would be safe at each point in your healing process.
5. Yoga and Its Calming Effects on the Mind and Body
A growing body of research shows that yoga can help you commit to addiction recovery.9 This practice combines elements of exercise, mindful meditation, and spirituality. Many rehab centers offer yoga, and you can easily find classes in most areas or online.
Yoga promotes relaxation10 and improves your overall physical health. Experts believe that “yoga and meditation practices exert positive influence on addictive behaviors.”
6: Fidget Spinners
When energy builds up and demands an outlet, instead of drinking to subdue energy you can reach for something as simple as a fidget spinner, slime, or other fidget toy to release tension and free your mind. You can find a myriad of options on Amazon.
Keep a few fidget toys in your purse or pocket, and bring them to work to have on-hand at a moment’s notice. Some fidget toys provide sensory stimulation through pressure or texture, like bumpy rings or a thick dough you can knead to help yourself unwind and relax.
7: Balance Boards
Using something like an Indo Board requires your focus and attention, which can serve as an excellent way to destress by giving your brain and body a fun distraction. Balance boards command coordination and control, similar to surfing or riding a skateboard.
Incorporating balance boards into your daily routine, or taking it out each time you feel the urge to drink, can become an enjoyable part of your recovery journey.

8. Spending Time in Nature for Relaxation and Stress Relief
Just being in nature has numerous psychological benefits:11
- Reduces negative feelings
- Increases positive emotions
- Decreases impulsivity
- Improves physical health
- Lowers anxiety and depressive symptoms
- Reduces stress levels
- Alleviates drug and alcohol cravings
And when it comes to relaxing without alcohol consumption, this strategy is especially helpful. Data shows that spending time outdoors can help you recover from alcohol addiction.12 This is also a great way to connect with other people. For example, you could go camping with friends or join a local hiking group.
9. Creative Outlets
Artistic pursuits like painting, drawing, or crafting can be very therapeutic. What’s more, they offer an emotional outlet. This is extremely important during addiction recovery, when you might still be learning new coping skills.
Creativity reduces stress13 and anxiety and improves overall well-being. Data shows these activities can also benefit your physical health. Subjects in several studies reported reductions in chronic pain, fatigue, and sleep problems after working on creative projects.
10. Reading Books
While it might look passive from the outside, reading is an extremely creative activity. Think about what happens in your mind when you read. You might see images in your head, draw connections to your own life, or just imagine how it feels to be somewhere else.
Experts at the National Alliance on Mental Illness (NAMI) explain that reading is “a healthy escape.”14 It lets you take a break from the stress of daily life without the negative effects of alcohol. Reading can also enrich your inner world, exposing you to new ideas and perspectives. By practicing this coping strategy, you can learn new ones at the same time.
11. Writing and Journaling
Writing—and especially journaling about your life—is a great way to process your thoughts and feelings. Studies show that writing can support recovery from alcohol addiction.15 Specifically, it can boost your self-confidence and stimulate new brain activity. If you join a writing group, it can also help you connect with other people.
Writing is an extremely accessible creative outlet. Unlike painting or crafting, you don’t need to invest in any specialized supplies. It’s also easy to keep your work private, even if you write in public places. This is a great way to explore your deepest feelings in a protected space. And if you ever want to, there are also plenty of ways to share your writing with the world.
Pouring a glass was my pause button, and then I’d have a huge spike in anxiety after heavy drinking that negates all of the benefits. Reframing how you relax is essential; you need a new off button, and there are alternatives without the hangover effect
-Amanda U.
12. Self-Care Practices
Self-care might sound like a passing trend, but there’s a reason everyone’s doing it. These small rituals can improve your relationship with yourself. You are more than the roles you play in other people’s lives. You could be the best employee, boss, parent, friend, or hiking buddy anyone has ever had—but who are you to yourself?
Simple activities, like taking a relaxing Epsom salt bath or painting your nails, can make a big difference. These practices let you give and receive love at the same time. They can also be relaxing, satisfying, and just plain fun.
There’s much more to self-care than pampering yourself. You can also think of going to therapy or eating well as forms of self-care. For many people in recovery, these activities are non-negotiable. Once you find the strategies that work best for you, look for ways to build them into your daily routine.
13. Connecting With Loved Ones
Spending quality time with your friends and family is hugely important during addiction recovery. Data shows that positive relationships are “crucial for reaching long-term abstinence16 or stable recovery from substance use.”
Friends and family can provide emotional support and hold you accountable in every phase of your healing journey. You can also ask them to invite you out to try new sober activities. If your loved ones enjoy a certain hobby, you might just like it too.
Any addiction, but especially high-functioning alcohol addiction, can interfere with your relationships. Maybe you isolated yourself to hide your addiction from your loved ones. Or maybe your close friends encourage you to keep drinking. In any case, you might have to rebuild your community during recovery. Consider joining a support group or attending a local meet-up to connect with people who share your values.
14. Engaging in Puzzles, Brain-Teasers, and Crosswords
In any stage of addiction, intellectual stimulation might lower your risk of addiction.17 One study suggests that solving puzzles and similar activities can rewire the brain, making you less interested in alcohol or drug use.
Puzzles and brain-teasers are easy to find. You can play sudoku online, download an app like Tetris, or do a new crossword puzzle every morning. These games keep your mind engaged, helping you relax while you enjoy a simple challenge.

15. Music and Audio
Music is a powerful tool for regulating your feelings. Studies show that listening to music activates the limbic system,18 which is the part of your brain that controls emotion and memory. Different types of music have different emotional impacts, depending on the tempo, volume, and genre. You might also associate certain pieces of music with different times in your life.
When you’re first learning how to relax without alcohol, you can explore different types of music to see what works for you. Instrumental pieces or nature sounds might help you unwind. In addition to music, you might try listening to podcasts or audiobooks.
16. Aromatherapy and Scented Relaxation
It’s no secret that alcohol can be addictive. That’s partly because drinking affects all of your senses, including your emotional responses. While that may be enjoyable in the short term, alcohol abuse just isn’t sustainable.
Relaxing without alcohol can also be a full-body experience. Engaging your sense of smell can help you create a soothing environment. You could take a bath with essential oils, light a scented candle, or put a diffuser on your desk at work. Various scents also have unique emotional effects. For example, studies show that lavender decreases anxiety.19
17. Cultivating a Positive Mindset
Positive thinking can help you heal from alcohol20 abuse. But there’s a fine line between cultivating optimism and invalidating your feelings. With the right support, you can learn to strike a balance.
When you first enter treatment, it might take effort to look on the bright side. But as you continue to heal, your confidence will likely go up. You can also learn how to interrupt negative thought patterns in therapy. This becomes a positive feedback loop. As you make more progress, it often gets easier to maintain your recovery.
18. Quiet Reflection
This coping strategy is a lot like meditation, but it can be more accessible. For example, meditation can be triggering for some trauma survivors.21 And even if you love to meditate, you might not be able to use this skill while you’re driving a car.
Quietly reflecting on your own life helps you put recent events in perspective. Consider how far you’ve come in your recovery journey. What coping strategies are currently working for you, and what could use an update?
Try letting your mind wander for a set period of time—like 10 minutes, or for however long it takes you to wash the dishes. Take notes on any revelations so you can share them with your therapist. Then, bring yourself back to the present moment. This practice can offer valuable insight, but it’s important not to get lost in thinking about your past.

19. Practicing Gratitude
In certain stages of recovery, gratitude can help you sustain abstinence.22 Data shows that engaging in a regular practice of gratitude improves levels of satisfaction, optimism, and hope. It also improves sleep and reduces depressive symptoms. At first glance, the benefits seem endless.
There’s one caveat here. Researchers note that if you’re still actively abusing alcohol, a gratitude practice may not help you recover. In fact, it can have the opposite effect. According to one study, “if the client does not want to change or is ambivalent about change, a gratitude practice might affirm what is good in life while currently drinking.”
Once you start treatment, writing about gratitude23 can be extremely helpful. This practice helps you focus on positive experiences, putting more energy into the things that bring you joy. It might also help you connect with other people, especially if you decide to share your writing.
20. Gardening
Gardening improves mental health,24 reducing symptoms of depression and anxiety. It also helps people cope with stressful situations and everyday fatigue. And because stress can increase your risk of alcohol relapse,25 this is extremely important for people in recovery.
Caring for plants can also give you a sense of accomplishment. There’s nothing like eating a meal with vegetables you grew yourself. And if you join a community garden, you can use this hobby to build strong relationships.
21: Sleep-Inducing Supplements
Though alcohol can make you feel sleepy for a bit, it actually prevents you from getting good sleep. Healthier alternatives, like sleep supplements, can improve how much you sleep and the quality of it.
Supplements for sleep include melatonin, ashwagandha, valerian root, and magnesium, plus many others. Check with your doctor to ensure any of these supplements won’t interact poorly with other medications, or impact pre-existing conditions you may have.
These natural ways to relax typically aren’t addictive or harmful, meaning you can take them as long as you need.
 Good Day Chocolate
Good Day Chocolate
22: Ritual Replacements
Preparing and drinking an alcoholic drink at night can bring the same comfort as the ritual of a morning coffee. Losing this part of your life can be hard. But you can keep the ritual and all its comforts by replacing alcohol with a non-alcoholic drink.
If you live with someone else, see if they might want to join your new ritual too. This can function simultaneously as check-in time with a loved one.
These are just some of the options you can try, adapting flavors and recipes to your preferences:
- Sparkling waters—try add-ins like fruit, herbs, or liquid water enhancers.
- Tea, especially relaxing blends with chamomile.
- Hot chocolate.
- Kombucha.
- Tart fruit juices, like cranberry or pomegranate juice, can replace the flavors of wine.
- Non-caffeinated sodas.
- Mocktails that include the ingredients of an alcoholic drink, but without the alcohol. You can also buy pre-made mocktails or 0-proof liquors.
 Affirmation Coloring Book for Adults
Affirmation Coloring Book for Adults
23: Adult Coloring Books
Coloring books aren’t just for kids anymore. People of all ages can benefit from the relaxing, de-stressing qualities of coloring. Adult coloring books vary from children’s in that they’re a little more complex in their designs, and with shapes and scenes adults would find more appealing. When you’re done you can even frame the piece.
Coloring in shapes requires no artistic abilities to shade or mix colors. Simply buy a pack of markers or crayons and start filling in the lines.
24: Dabble in New Hobbies
Try as many new hobbies as you can to give yourself a collection of calming activities to alter between. Some may be more relaxing, like knitting, or require more focus and attention, like building Legos or model airplane sets. Switching between hobbies and having multiple to choose from can alleviate both boredom and stress.
Here are a few hobbies you could try to relax and wind down:
- Crocheting blankets, washcloths, or making stuffed animals.
- Deep cleaning.
- Pottery–make yourself plates, mugs, bowls, and decorations.
- Jewelry making.
- Metal detecting (this also helps you spend more time in nature).
- Upcycling thrifted clothes.
- Embroidery.
- Arranging and pressing flowers.
There are countless ways to relax without drinking. The important thing is to choose activities that resonate with you. When you genuinely enjoy what you’re doing, it becomes easier to stay present, instead of trying to escape through addiction.
Learn more about treatment at alcohol rehab centers to get the support you need in any stage of recovery.
Frequently Asked Questions About How to Relax Without Alcohol
How can I relax without alcohol?
It’s entirely possible to relax without alcohol through various methods, such as deep breathing, mindful meditation, progressive muscle relaxation, physical activities, yoga, spending time in nature, and creative outlets like art and writing.
How does engaging in creative activities help in relaxing without alcohol?
Engaging in creative activities like painting, drawing, crafting, reading, and writing offers a therapeutic outlet for emotions and stress relief. These activities help you stay positive, improve your overall well-being, and support addiction recovery by promoting self-expression and diverting your focus from alcohol.
