When researching treatment options, one of the first questions that comes up is how long rehab programs last. You’ll find programs ranging from 30 days to 6 months or longer, which can feel overwhelming when you’re trying to make decisions about care.
Treatment duration isn’t the same for everyone because specific needs vary significantly between individuals. Someone addressing a short-term mental health episode may have different timing requirements than someone working through a severe eating disorder. Co-occurring mental health conditions, previous treatment history, and the severity of addiction all influence how long treatment takes.
The most common program lengths are 30, 60, and 90 days, though some people benefit from shorter intensive programs while others need extended care lasting several months. Research suggests that longer treatment periods generally lead to better outcomes, but the optimal length depends on your specific circumstances and treatment goals.
This guide examines standard rehab durations and what makes each timeframe effective for different situations. You’ll learn about the factors that influence treatment length and how clinical teams determine appropriate program duration.
Understanding these elements can help you work with your healthcare provider to choose the treatment options that align with your needs, insurance coverage, and recovery goals. The right program length is one that provides an adequate length of time to build sustainable recovery skills.
Standard Rehab Program Lengths
The most common residential treatment durations1 each offer distinct advantages depending on your recovery needs and circumstances.
30-Day Programs
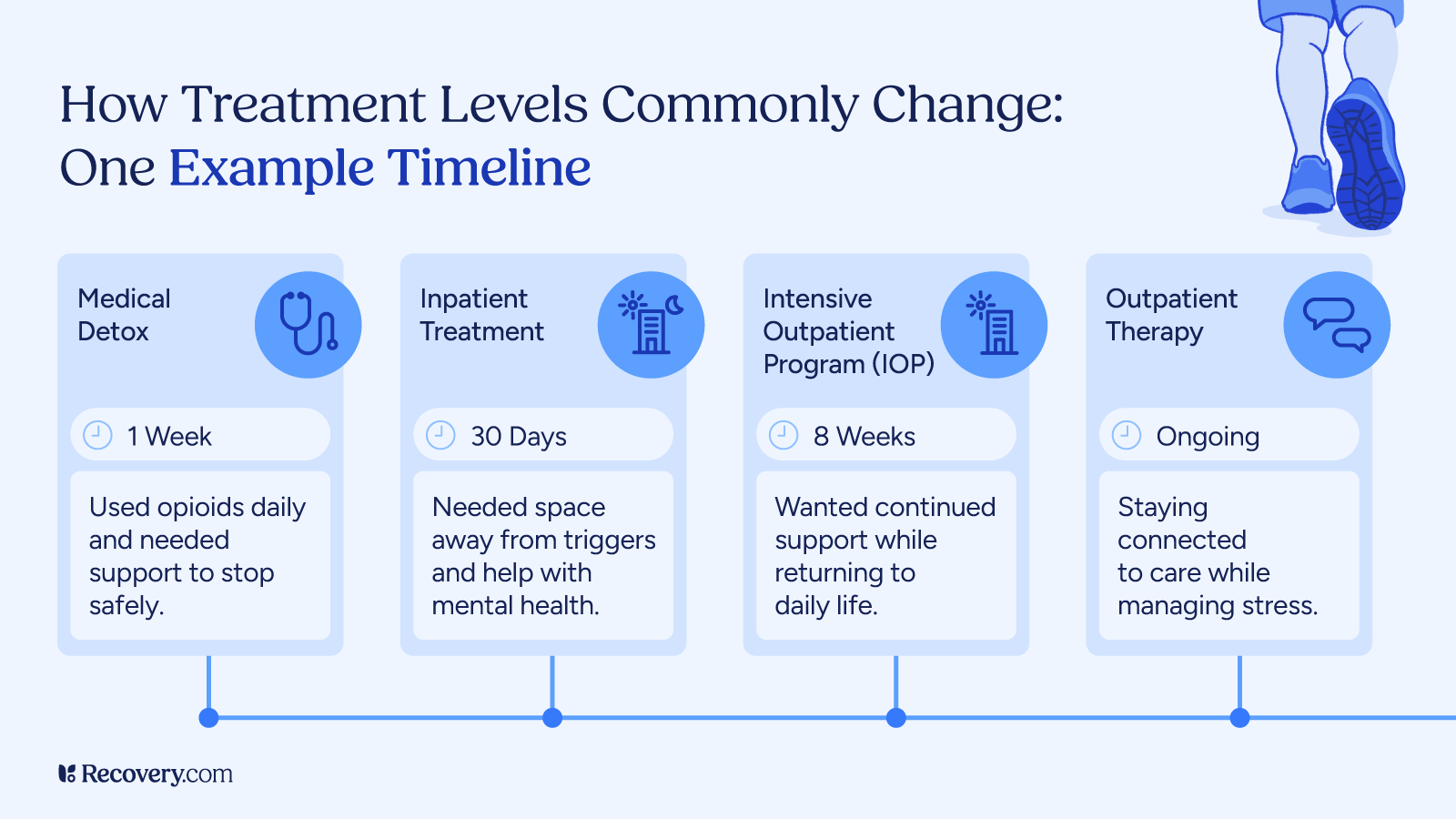
30-day programs are the standard length for many residential treatment centers. These programs focus on treating drug or alcohol addiction symptoms, addressing underlying mental health issues, and establishing the foundation for healthy lifestyle changes. If you need detox, they may refer you to a specialized detox center or offer it onsite.
During this timeframe, you’ll participate in intensive group and individual therapy, learn coping strategies, and work on identifying triggers and relapse prevention techniques. A lot of patients find 30-day programs highly effective. But some people choose to extend their stay if they feel they need more time to build stability and confidence before returning to their daily environment.
60-Day Programs
60-day programs allow for deeper therapeutic work. This extended timeframe provides more opportunities to practice new coping skills, work through unresolved trauma or other mental health issues, and strengthen sobriety skills. Many people find that the second month of treatment is when significant breakthroughs occur in therapy.
These programs often include more comprehensive family involvement and begin preparing for the transition back to daily life. The additional time allows for gradual skill-building and can help you identify potential triggers or challenges you might face after leaving treatment. This duration strikes a balance between intensive care and practical time constraints.
90-Day Programs
90-day programs are often considered the gold standard in drug addiction treatment. Some research indicates that longer treatment programs are associated with better long-term outcomes and lower relapse rates.2 This timeframe allows for complete stabilization, thorough exploration of underlying issues, and more extensive practice of recovery skills.
During the third month, many programs focus on real-world application of skills learned in treatment. You’ll have time to work through multiple challenges and setbacks within a supportive environment. Extended programs also provide more opportunities for family therapy and rebuilding relationships damaged by addiction.
Factors That Determine Rehab Length
1. Severity of Addiction
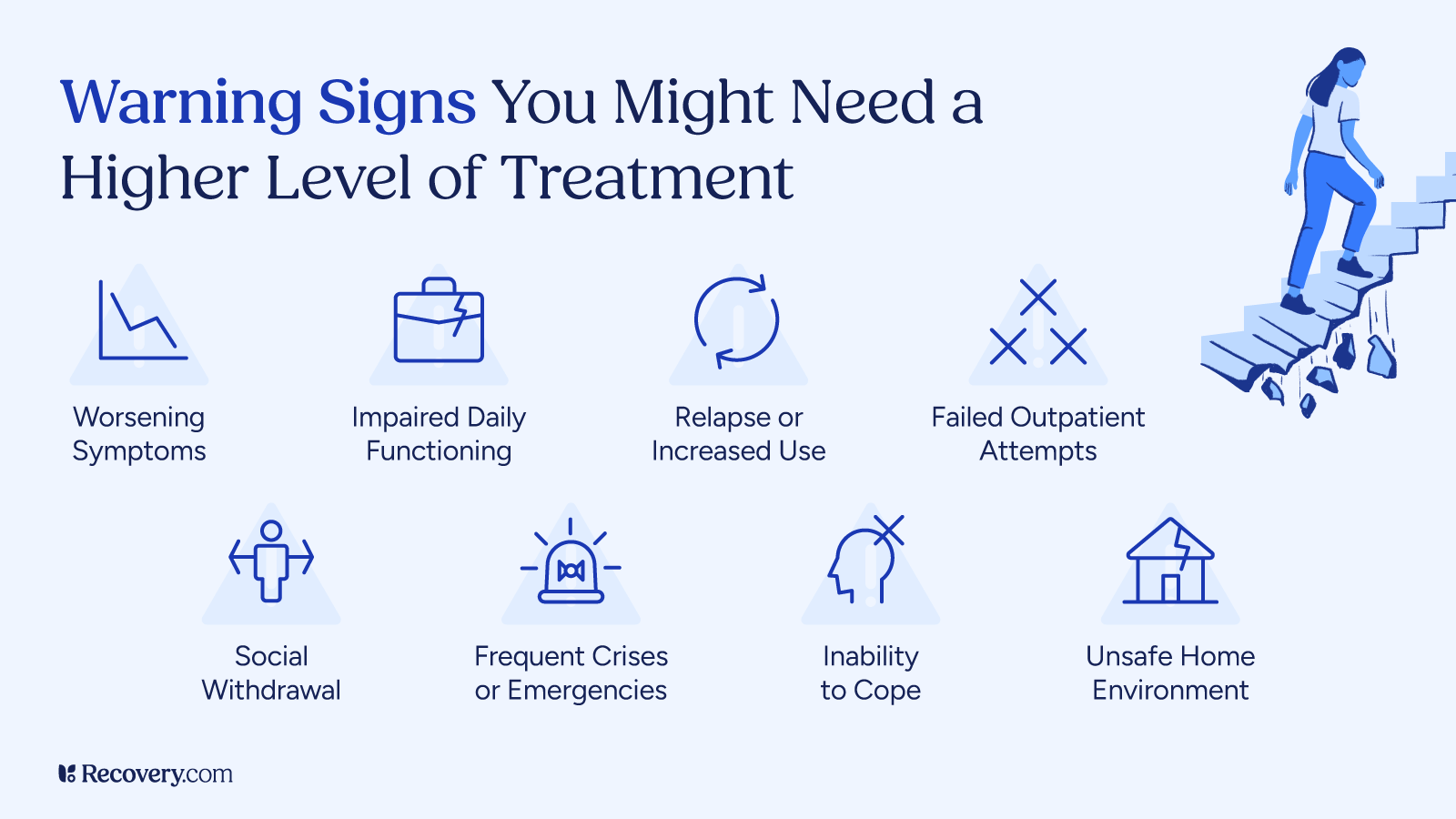
The complexity and severity of your addiction significantly influences how long substance abuse treatment takes.3 People with long-term substance use patterns or multiple addictions typically need more time for stabilization and recovery skill development.
Research shows that more severe addiction patterns often require longer initial treatment4 and extended continuing care. Greater severity is also associated with more intense withdrawal symptoms and higher risk for medical complications, which can extend the stabilization phase before therapeutic work begins effectively.
Behavioral addictions like gambling, gaming, or compulsive shopping can be equally complex and may require extended treatment to address underlying triggers and develop healthy coping mechanisms. Eating disorders also require specialized care5 and often need longer treatment durations due to their complex medical and psychological components.
2. Mental Health Considerations
Co-occurring mental health disorders (also known as dual diagnosis) often require additional treatment time. Conditions like depression, anxiety, PTSD, or bipolar disorder need integrated care alongside addiction treatment. Childhood trauma, recent traumatic events, or other trauma histories may necessitate specialized therapies6 that extend program duration.
3. Chronic Relapse
Previous treatment attempts also influence length recommendations. People who have experienced multiple relapses may benefit from longer drug rehab programs7 to identify what didn’t work previously and develop more robust prevention strategies.
The good news is, each treatment episode provides valuable information about what approaches are most effective for your specific situation.
If you’ve experienced multiple treatment attempts, learn more about specialized approaches in our guide to breaking the cycle of chronic relapse.
4. Personal Circumstances
Your support system at home determines a lot about your recovery. Strong family support and stable housing may allow for shorter residential stays with transition to outpatient rehab. On the other hand, chaotic home environments or relationships that enable addictive behaviors may require longer residential treatment and careful discharge planning.
Work and financial considerations can affect which program you select, though many employers offer leave protections and insurance providers typically cover medically necessary treatment. Legal requirements, such as court-ordered treatment, may mandate specific program lengths. These factors should be balanced with your treatment team’s recommendations for optimal outcomes.
5. Your Treatment Response and Progress
Individual healing timelines vary significantly, even among people with similar presentations. Some people achieve stability quickly and gain strong recovery skills early in treatment. Others need more time to engage with the recovery process or work through their resistance to change in the early stages of sobriety.
Your clinical team should thoroughly assess you when you arrive at rehab and, throughout treatment, help determine how ready you are to transition between care levels. Factors like medication stabilization, therapy engagement, family involvement, and developing recovery skills all influence these decisions. The goal is to ensure you have adequate tools and support before stepping down to less intensive care.
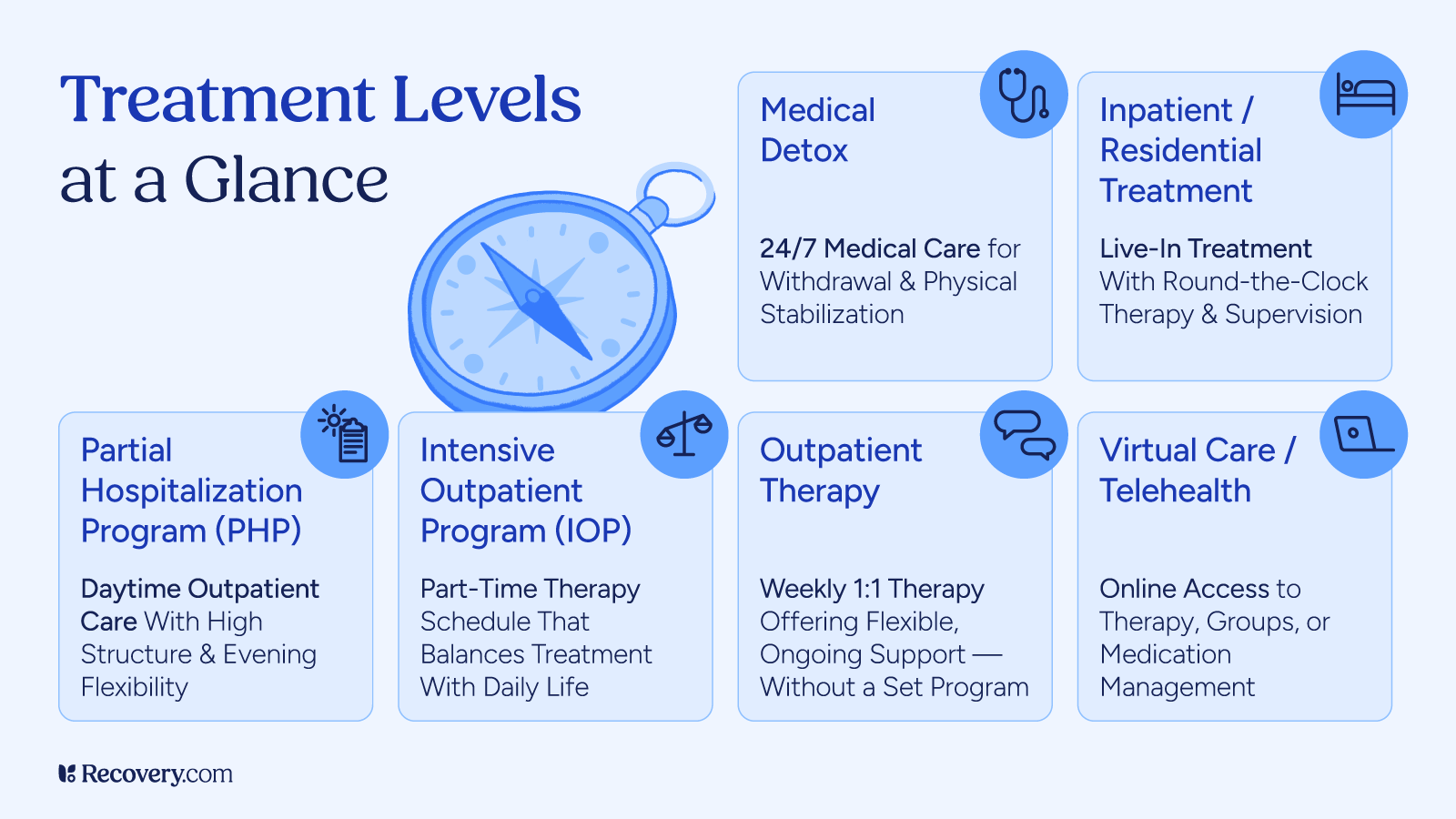
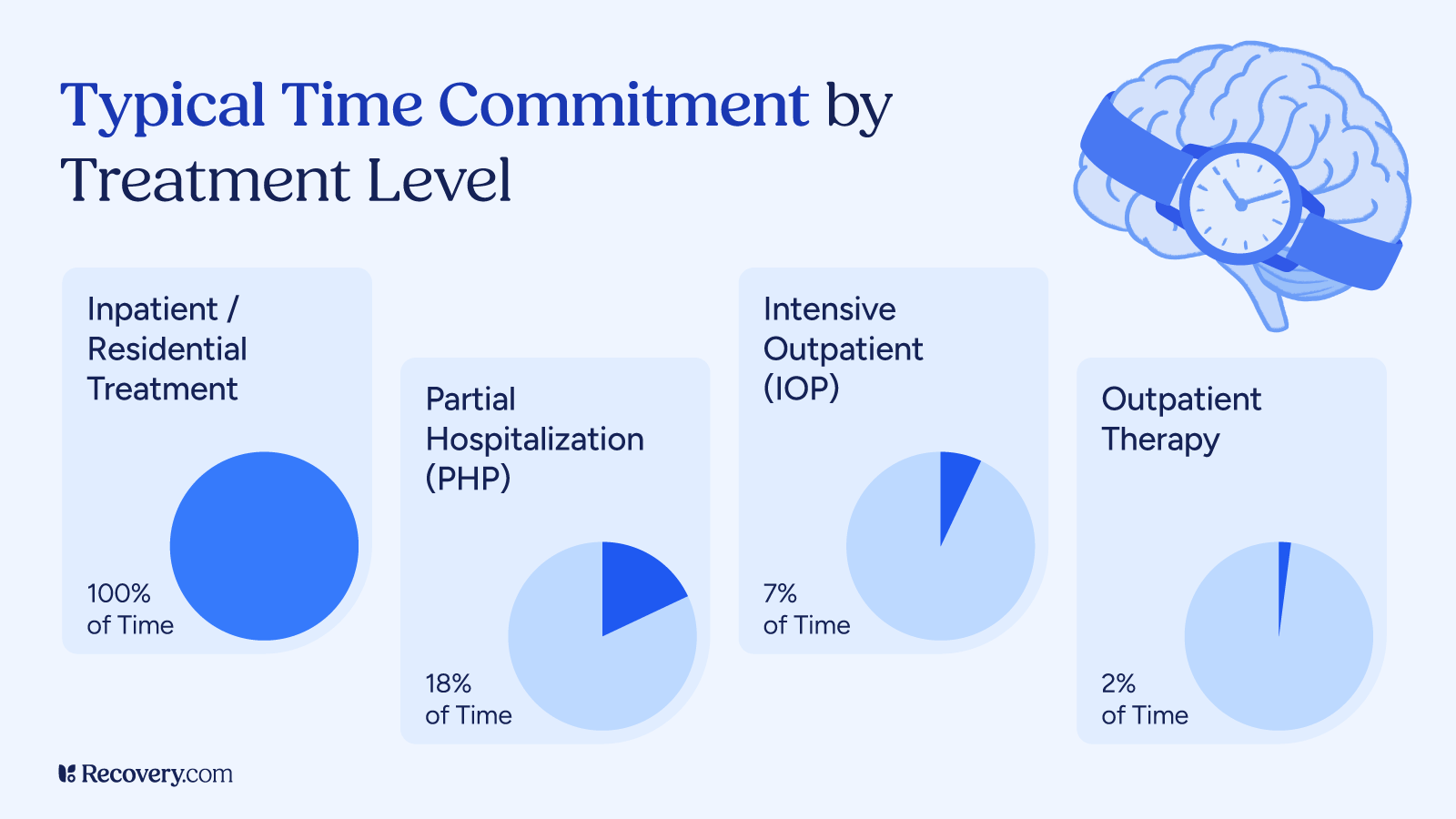
Types of Rehab and Their Typical Durations
Residential or Inpatient Rehab
Residential treatment programs typically range from 30–90 days, with some extending to 6 months or longer for complex cases. These programs provide 24/7 medical supervision and a highly structured environment that removes you from triggers and stressors in daily life. The immersive nature of these programs allows for faster skill development and medical stabilization.
Experts often recommend residential care for people with severe addictions,8 multiple failed outpatient treatment attempts, co-occurring medical conditions, or less stable home environments. A longer stay at a residential rehab facility might be helpful if you have complex trauma or multiple addictions.
Partial Hospitalization Programs
Partial hospitalization programs (PHPs) typically last 2–4 weeks to several months, depending on your needs. These programs provide day treatment services 5–7 days per week, offering more intensity than traditional outpatient care while allowing you to return home evenings and weekends.
PHPs are a bridge between inpatient treatment and outpatient care. They can be especially beneficial for people who need medical monitoring, medication adjustments, or intensive therapy, but don’t require 24-hour supervision. The schedule allows for gradual reintegration into daily life while maintaining therapeutic support and structure during the most vulnerable period of early recovery.
Intensive Outpatient Programs
Intensive outpatient programs (IOPs) commonly last 3–6 months, meeting 3–5 days per week for 3–4 hours per session. This format allows you to maintain work, school, or family responsibilities while receiving substantial treatment support. IOPs often serve as step-down care after residential treatment or as primary treatment for people with strong support systems.
The extended timeline in outpatient settings allows for more practice of recovery skills. You can apply what you learn in therapy to real-world situations and work through challenges with the support of your treatment team. This approach bridges the gap between intensive treatment and independently maintaining your recovery.
The Science Behind Treatment Duration
Understanding the biological and psychological processes involved in recovery helps explain why certain treatment lengths are more effective than others.
Brain Healing and Neuroplasticity
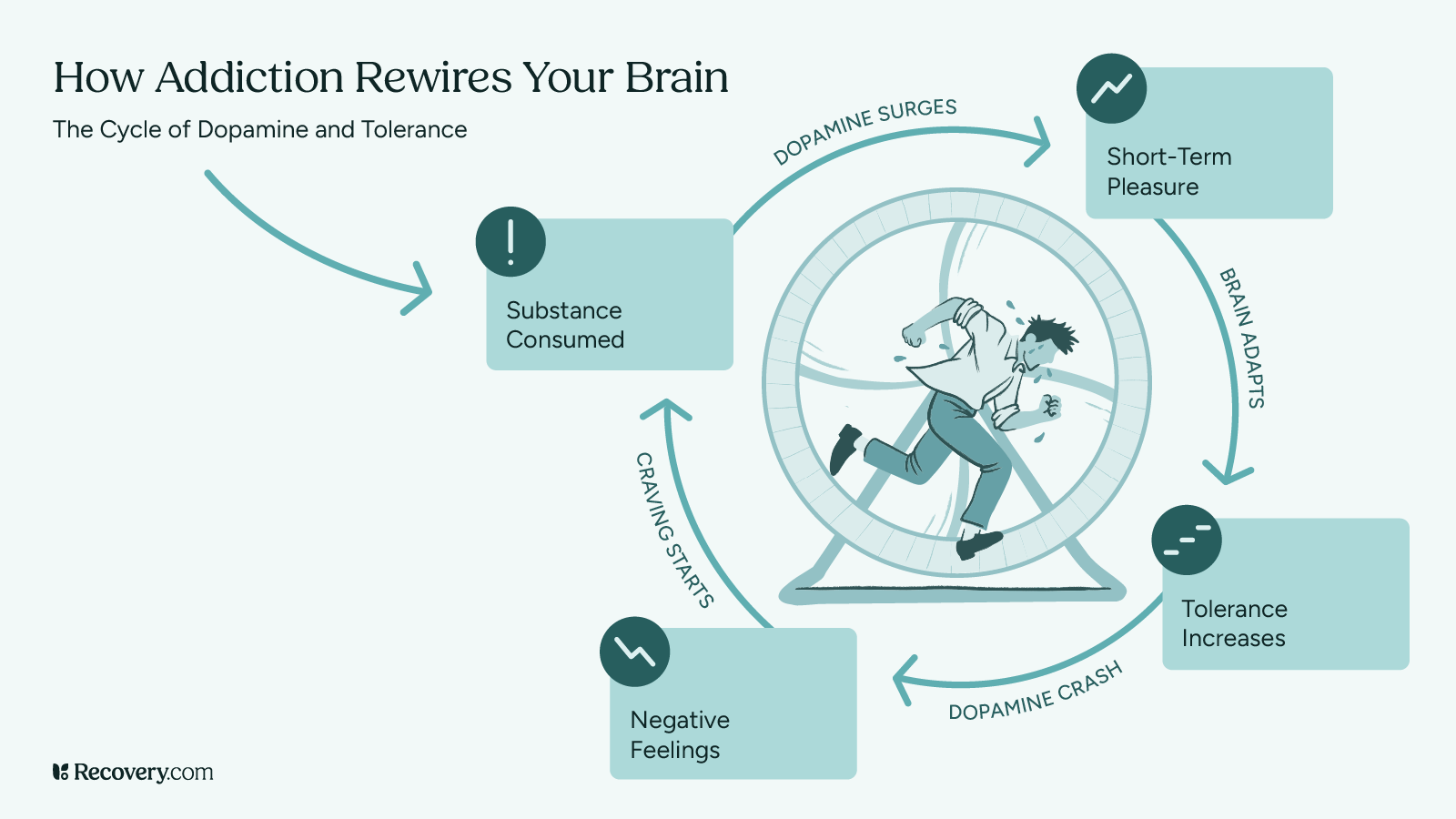
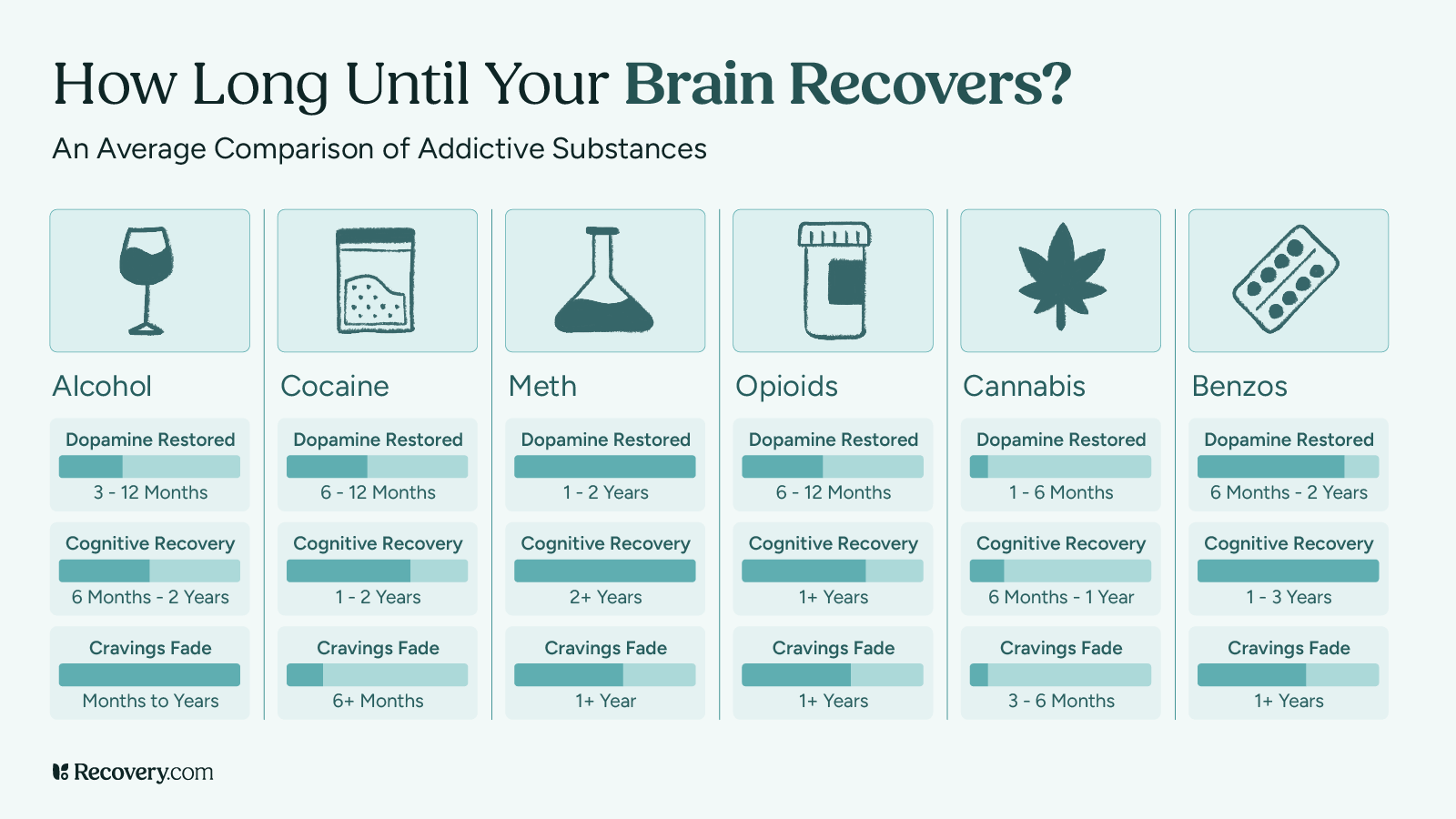
Addiction creates lasting changes in brain chemistry and neural pathways, particularly in areas responsible for decision-making, impulse control, and reward processing. Research shows that the brain begins healing within days of stopping substance use,9 but significant structural and functional recovery can take months to years.
In recovery, neural pathways associated with craving and compulsive behaviors gradually weaken over time, while areas responsible for executive functioning strengthen. This neuroplasticity process9 is part of why longer treatment periods often lead to better outcomes—they provide time for both brain healing and the development of new, healthier neural patterns through repeated practice of recovery skills and behaviors.
Breaking Cycles and Forming New Habits
Popular culture often references the “21-day rule” for habit formation, but research shows that complex behavior change takes much longer.10
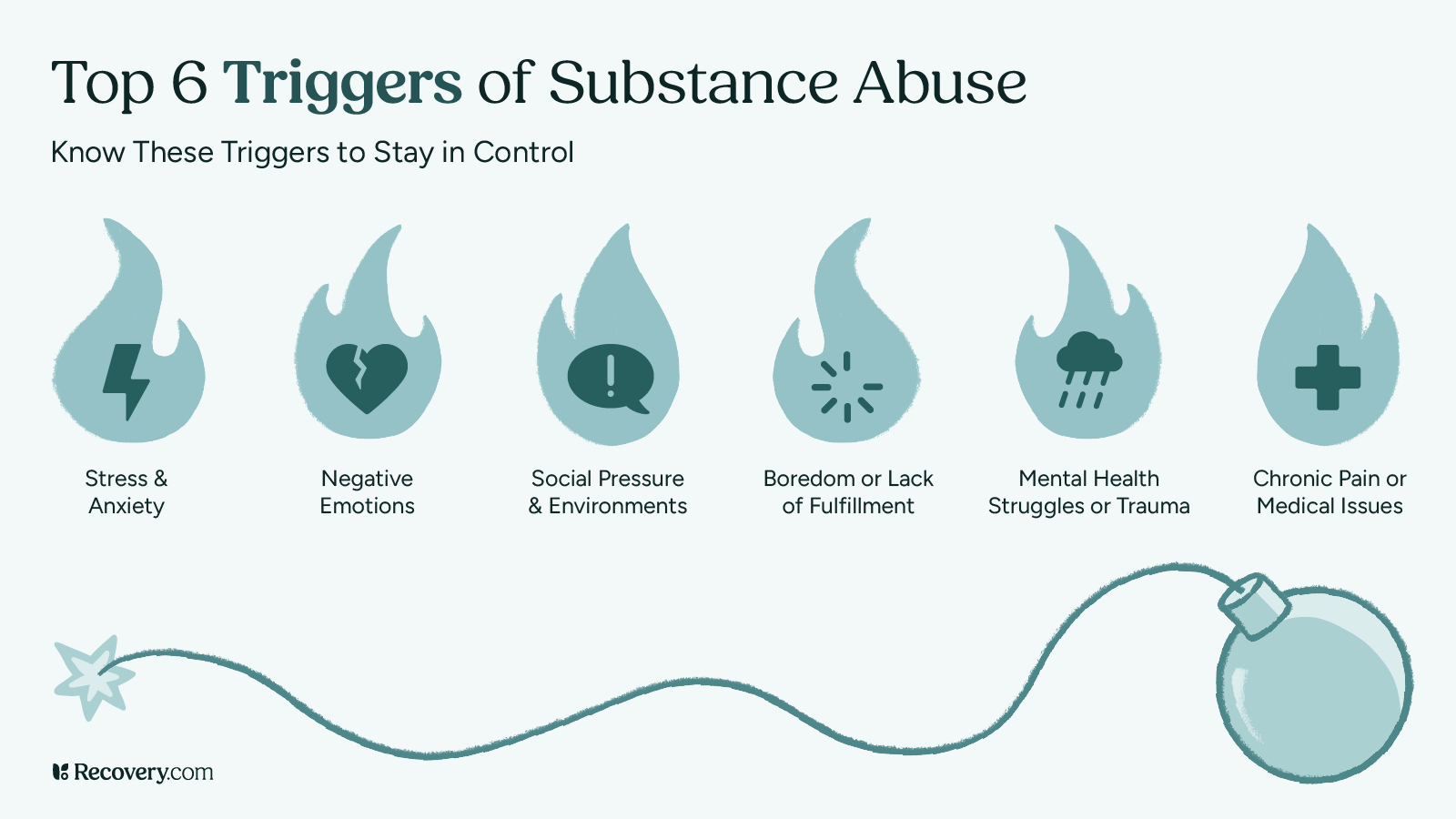
Addiction involves deeply ingrained patterns that extend beyond simple habits to include emotional regulation, social behaviors, and stress responses. Breaking these complex cycles requires time to identify triggers, practice new responses, and build confidence in using different coping strategies.
This involves unlearning automatic responses while simultaneously developing new skills—which is why intensive treatment periods are more effective than brief interventions for most people with more severe addictions.
What to Expect When Working with Treatment Professionals
When you contact a treatment center, they’ll start with an assessment to understand your situation. This involves talking with counselors and medical staff about your addiction history, mental health, any medical issues, and your home life. They use this information to figure out what type of treatment might work best and how long you might need to stay.
Good treatment centers will include you in these discussions. They’ll ask about your goals, what you’re comfortable with, and practical things like work or family responsibilities. As you go through treatment, they should check in regularly to see how you’re doing and adjust the plan if needed.
Quality vs. Quantity
Length of stay alone doesn’t determine how effective your treatment is. What’s more important is the quality of care, including evidence-based therapies, qualified staff, and comprehensive services. A well-designed 30-day recovery program with excellent aftercare planning may be more effective than a longer program with less therapeutic effectiveness.
When you’re looking at programs, pay attention to what types of therapy they use. Look for places that use proven methods like evidence-based therapies and trauma-informed care. The best programs don’t just focus on addiction—they also help with mental health, physical health, family issues, and relational skills. They should also have a clear plan for supporting you after you leave treatment.
What Happens After Initial Rehab
Recovery doesn’t end when formal treatment concludes. Continuing care planning is essential for maintaining progress and preventing relapse. This typically includes ongoing therapy sessions, support group participation, regular medical follow-ups, and sometimes sober living arrangements.
Sober living homes provide a transitional environment where you can practice recovery skills while gradually resuming independence. These residences typically require 3–12 months of participation and provide structure, peer support, and accountability during early addiction recovery.
Long-term sobriety involves creating a lifestyle that sustainably supports your recovery. This includes building healthy relationships, finding meaningful activities, learning to manage stress effectively, and having a plan for handling potential relapse triggers. Many people benefit from ongoing therapy or support groups for months or years after initial treatment. The key is creating a recovery plan that evolves with you over time.
Find the Right Program for You
Finding the right treatment program length for yourself or a loved one is an important decision that deserves careful consideration with qualified professionals. Recovery.com connects you with treatment centers that offer personalized care and evidence-based programs. Search for accredited facilities in your area and take the first step on your recovery journey today.
FAQs
Q: How long do you normally go to rehab for?
A: Most people attend residential rehab centers for 30–90 days, followed by outpatient care lasting 3–6 months or longer.
Q: Why is rehab 90 days?
A: Research shows that longer programs provide sufficient time for brain healing, skill development, and behavior change, leading to better long-term outcomes.
Q: What factors determine the length of a rehab program?
A: The severity of substance use disorders, mental health conditions, previous treatment history, support systems, and individual treatment response all influence the length of treatment.
Q: How long does rehab last for different substances?
A: While treatment principles are similar across substances, some may require longer detoxification periods or specialized approaches that can affect overall duration.