Reaching out for help takes courage—and you’ve already shown that by being here. Whether you’re dealing with addiction, mental health concerns, or both, we know how overwhelming it can feel to find the right care. But you don’t have to figure this out alone. We’ll walk you through your options so you can feel empowered to make the choices that feel right for you.
A quick note about us: Recovery.com is an independent organization that helps people find quality care. We don’t own any treatment centers or take payments to recommend them. Our mission is simple: To give you honest, straightforward information so you can make the best choices for your recovery.
Understanding Types of Treatment
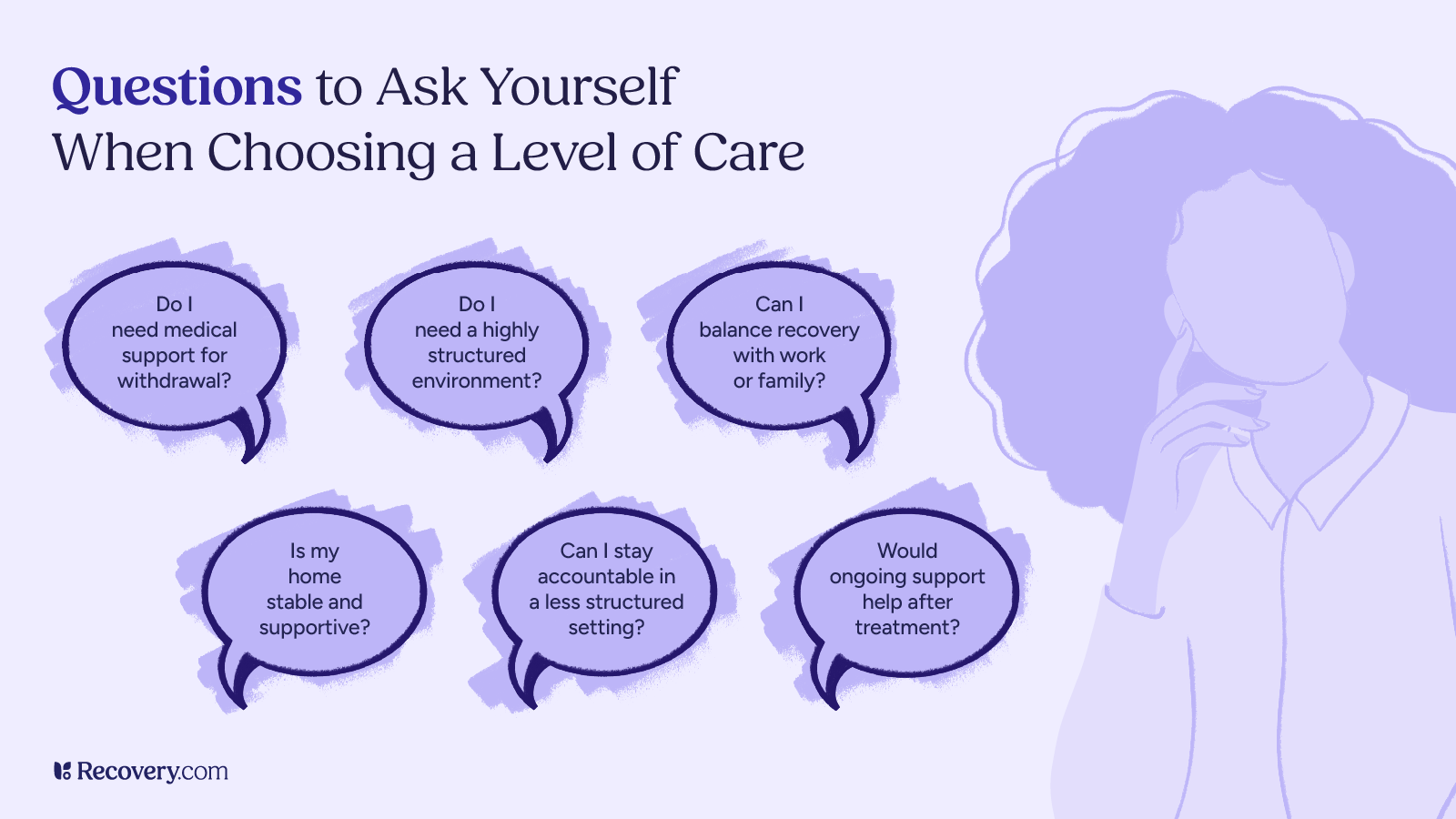
Recovery programs offer different levels of care to match your needs. Here’s what you need to know about each option:
Medical Detox: Getting Started Safely
If you’ve been using alcohol, opioids, or benzos regularly, starting with medical detox isn’t just helpful—it’s crucial for your safety. Detox is a safe landing pad where caring medical staff help ease you through those first challenging days. Many treatment centers offer detox onsite, or they can connect you with trusted detox centers nearby.
Have questions about the detox process? Our detox FAQ covers everything you need to know about starting treatment safely.
Inpatient (Residential) Rehab
This is what most people think of as “rehab”—you live at a treatment center while focusing completely on your recovery. It’s like pressing pause on daily life so you can concentrate on healing, with 24/7 support from qualified healthcare professionals. Inpatient programs usually run 30-90 days, and you can stay longer if needed.
Want to learn more about what residential treatment is really like? See our detailed guide to what happens in residential rehab.
What is the best way to find mental health and addiction treatment?
It often takes a few tries to find someone who really gets you. I always recommend starting with therapist directories, and don’t underestimate the power of asking trusted friends, family, or other healthcare providers for referrals. Look for someone who feels attuned to your needs. It’s okay if you don’t click with the first person; fit matters, and it’s worth finding someone who truly feels like a good match.
– Amanda Stretcher, MA, LPC-S | Crescent Counseling
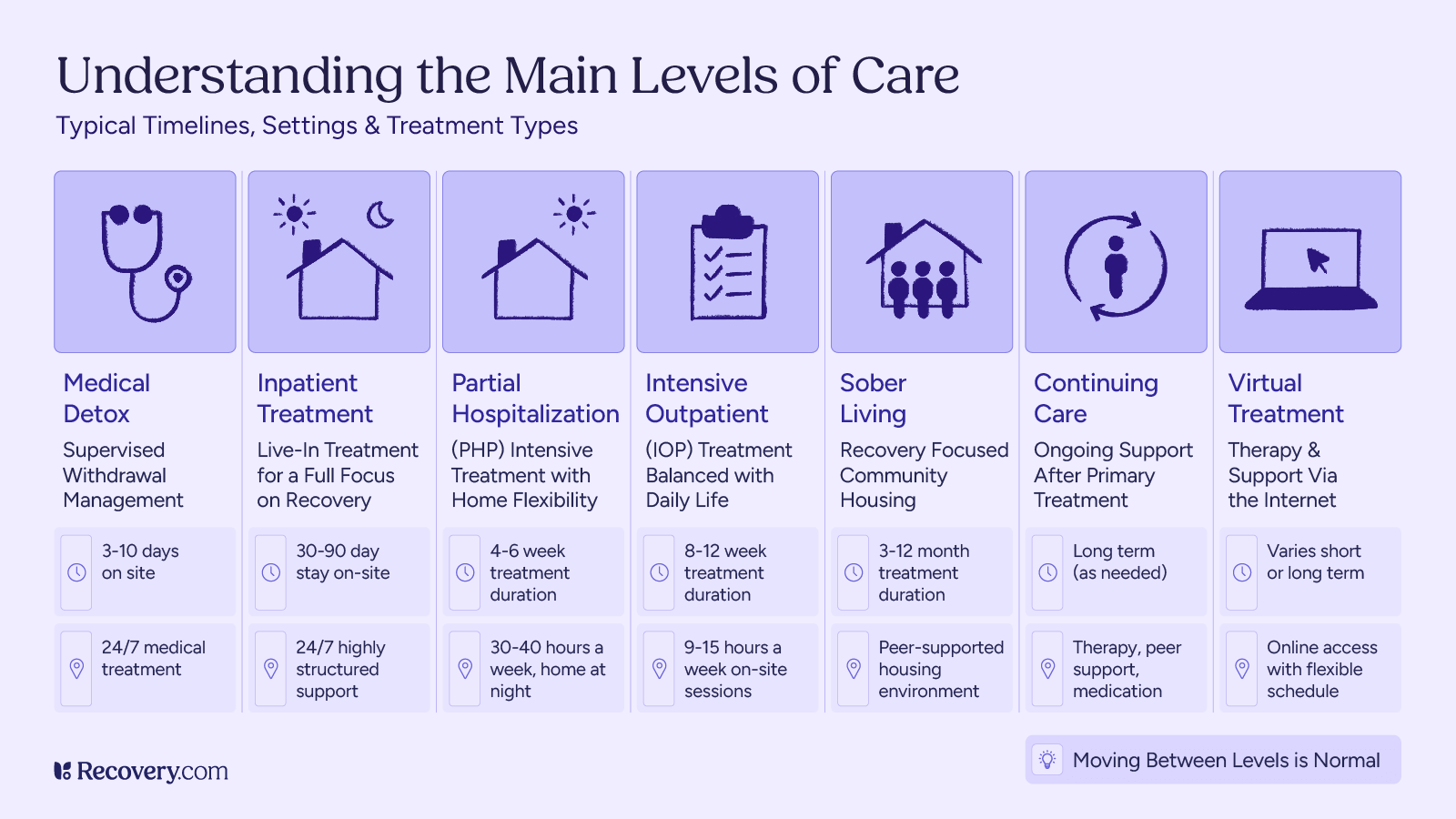
Partial Hospitalization Programs (PHP): The Middle Ground
Want intensive support but need to sleep in your own bed? Day treatment might be right for you. You’ll spend your days in treatment (usually 30-40 hours weekly) but head home each evening. It’s ideal if you have a stable home life or you’re stepping down from residential care but want to keep that strong support system.
Intensive Outpatient Programs (IOP): Flexibility Meets Structure
IOPs are great when you need to balance recovery with real life. You’ll attend treatment 3-5 days a week for a few hours each day, getting solid support while maintaining your daily routine. Many people choose this option when they have work or family commitments they can’t step away from.
Not sure whether you need day treatment or intensive outpatient? Our guide breaks down the key differences between PHPs and IOPs.
Sober Living: Your Recovery Community
Think of sober living as your home base for recovery after completing primary care treatment. You’ll live with others who get what you’re going through, in a substance-free environment that supports your new life. It’s perfect when you want that extra layer of support or need a fresh start.
Continuing Care: Growing Stronger
As you move forward, your needs will change—and that’s totally normal. Your care team will help you build a plan that grows with you, whether that’s regular therapy check-ins, medication support, or practical help with life skills.
Wondering what happens after rehab? Our guide to continuing care explains how to build lasting support for your recovery journey.
Virtual Treatment: Recovery at Your Fingertips
While online health services aren’t for everyone (especially if you need detox or round-the-clock support), they are making care more accessible than ever. If transportation is tough or you need extra scheduling flexibility, virtual options might be just what you’re looking for.
What to Look for in a Treatment Provider
When you’re looking at treatment programs, it helps to know what sets the great ones apart from the rest. Let’s start with one of the most important things to check—their credentials.
All About Licensing and Accreditation
Accreditation is a stamp of approval from organizations that check healthcare providers for quality and safety. Good programs will have their credentials proudly on display and be happy to talk about them. Not sure about a program’s credentials? You can always double-check them through your state’s licensing board or the Joint Commission’s website.
Here are the important ones to look for:
- The Joint Commission: This is the gold standard in healthcare. When you see this seal, you know the program meets the highest quality standards.

- CARF (Commission on Accreditation of Rehabilitation Facilities): This organization thoroughly reviews treatment centers to ensure quality care. Their seal means a program has met rigorous standards for treatment and safety.

- Your state’s Department of Health license: This is your state’s official oversight of treatment programs. Every quality program should have this license, which shows they meet local requirements for providing safe, ethical care.
Want to verify a program’s credentials? Just ask! Ethical admissions teams will be happy to provide any information you need to feel comfortable moving forward.
The People Who Will Support Your Recovery
The heart of any great treatment program is its team. You want people who bring both expertise and compassion to your care. Quality programs have a mix of professionals—from psychiatrists and therapists to counselors and nurses—all working together to support you. Many programs also include team members who’ve been through recovery themselves, bringing both professional knowledge and personal understanding to your care.
Here’s who you’ll meet on your care team:
- Medical team (doctors, nurse practitioners, physician assistants, etc.): These professionals hold current state medical licenses and specialize in addiction medicine and mental health care. They’re there to keep you safe and comfortable and care for any medical conditions, especially when you’re first starting recovery as a new patient.
- Therapists and counselors: Your therapists will have state licenses (look for credentials like LMFT, LCSW, or LPC) and experience helping people through recovery. They’re the ones who will work with you one-on-one and in groups to build your recovery skills.
- Holistic practitioners: Many programs employ wellness professionals who support your whole-person healing through practices like meditation, yoga, art therapy, or nutrition counseling. They work alongside your core clinicians to support your overall well-being.
Don’t hesitate to ask about the team’s experience and credentials—quality programs are proud of their staff and happy to tell you about their qualifications.
Learn what credentials to look for in a quality treatment team in our guide to understanding rehab staff qualifications.
Proven Treatment Approaches
The best programs use approaches that science has shown actually help people heal. These aren’t just trendy techniques—they’re proven methods that have helped many people build strong, lasting recovery.
You’ll work with therapists trained in evidence-based interventions like CBT (cognitive behavioral therapy), which helps you change unhelpful thought patterns and behaviors. Other proven methods like DBT (dialectical behavior therapy) teach you how to manage emotions and stay present, while ACT (acceptance and commitment therapy) helps you build a meaningful life in recovery. These practical tools give you real skills for lasting change.
Want to learn more about what makes these approaches so effective? Check out our guide to evidence-based addiction treatment methods.
Family Involvement
Quality programs understand that addiction affects the whole family. They’ll typically include your loved ones in the recovery process through family therapy sessions, educational programs about addiction, and support for rebuilding relationships. Many also provide resources to help family members with their own healing journey—because recovery is stronger when families heal together.
Get the details on how family therapy works in treatment in our guide to understanding family programs in rehab.
Open Communication
Good treatment programs prioritize clear, honest communication. The staff should take time to explain things clearly, answer your questions thoughtfully, and include you in treatment decisions. They understand that keeping you informed and involved is crucial to your recovery success.
Understanding Costs and Coverage
A trustworthy treatment center will be completely open about the financial side of care. They should explain all costs upfront, help you understand what your insurance plan will cover, and be clear about any additional expenses you might face. Good programs will also walk you through payment options and help you verify your health insurance coverage before you commit. There shouldn’t be any surprise fees or hidden costs along the way.
Get the full details on pricing, insurance coverage, and payment options in our guide to understanding rehab costs.
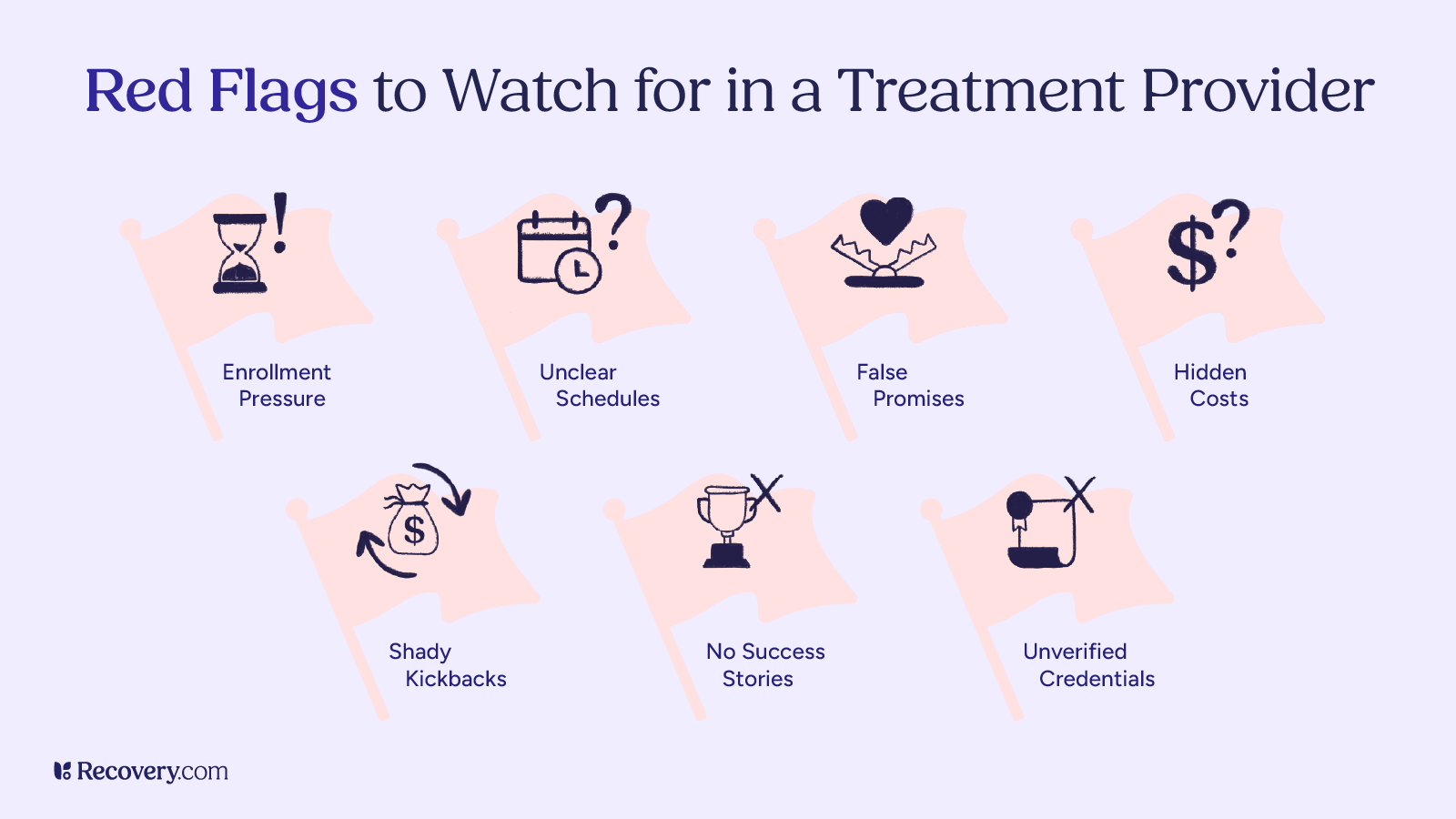
Watching Out for Red Flags
While there are plenty of reputable treatment programs out there, it’s important to trust your gut if something feels off. Be cautious if a program:
- Pressures you to enroll right away using aggressive sales tactics
- Gets vague when you ask about daily schedules or treatment details
- Makes promises that sound too good to be true, like guaranteeing success
- Isn’t clear about costs or adds surprise fees
- Offers kickbacks or referral fees for signing up (this is actually illegal!)
- Can’t share any success stories or references from past clients
- Doesn’t have proper licenses and accreditations
The right treatment center will respect your need to gather information and think things through. They know this is a big decision that shouldn’t be rushed—after all, it’s about your health and recovery.
Sadly, treatment scams are out there—but we can help you spot them. Learn more in our guide to avoiding common rehab scams and unethical practices.
How do I find the right treatment provider for what I need?
Finding the right mental health provider starts with checking your insurance network so you can access care without financial stress. From there, read provider bios carefully—look for someone who specializes in your specific concerns and whose approach resonates with you. If something in their bio feels relatable or comforting, that’s a good sign. And remember, finding a therapist is like finding the right pair of shoes—you might have to try a few on before you find the perfect fit.
– Rebecca Tenzer, MAT, LCSW, CCTP, CGCS, CCATP, CCFP, CIMPH | Astute Counseling & Wellness Services
Practical Steps to Finding the Right Provider
1. Start With a Professional Assessment
Many treatment centers offer free, confidential assessments over the phone to help you understand what level of care might work best for you. Their admissions team will ask about your situation and walk you through your options. You can also talk with your primary care provider (PCP), therapist, or local mental health professional to get their recommendations. The goal is to make sure you find care that fits your needs—you don’t have to commit to anything during these initial conversations.
2. Check Your Insurance Coverage
Most treatment centers have insurance specialists who will check your benefits for free—just call and give them your insurance information. They’ll work directly with your insurance company to find out exactly what’s covered, including how many days of treatment they’ll pay for and what your out-of-pocket costs might be.
You can also call your insurance provider yourself to learn about your mental health and substance use benefits. Either way, make sure to ask about in-network treatment centers (which usually cost less) and get clear on things like deductibles, out-of-network costs, and co-pays. Don’t worry if this feels overwhelming—that’s why admissions teams are there to help you figure it all out.
Learn more in our complete guide to using insurance (including Medicare) to pay for rehab treatment.
3. Research Your Options
Take some time to explore different types of providers that interest you. Use our treatment finder to get detailed information about each program, including costs, photos, virtual tours, and what day-to-day life is like there. You can also read online reviews about other people’s experiences (keeping in mind that everyone’s journey is different). Many centers welcome in-person visits, too.
4. Ask the Right Questions
When you talk with treatment centers, don’t be shy about asking questions—the right program will welcome them. Ask what a typical day looks like, what kinds of therapy they offer, and how they’ll help with both substance abuse and mental health conditions. It’s also good to learn about how they include family in treatment and what kind of support they offer after you complete the program. Remember, you’re looking for a place that feels right for you, and these conversations help you get a sense of how they’ll support your recovery.
Make the most of your first conversation with treatment centers using our guide on what to ask when calling rehab admissions teams.
What should I know about health insurance?
When searching for a mental health or addiction treatment provider, understanding your health insurance coverage is crucial to ensure you receive the care you need when you need it without unexpected costs. General considerations may include being knowledgeable of coverage verification, your in- versus out-of-network providers, prior authorization requirements, co-pays, deductibles, co-insurance, out-of-pocket maximums, duration of coverage, treatment types, medications, and anything else specific to your situation. Although your provider’s website may have much of this information readily available, particularly if you explore your personal account, it is recommended to reach out directly should you warrant further clarity. It is especially important to ensure that everything is authorized prior to engaging in treatment, as any issues here may lead to unexpected costs that can add up significantly.
– Matthew Glowiak, PhD, LCPC, CAADC, ACS, NCC | Hazelden Betty Ford Graduate School

Connect With Treatment Today
Recovery is a process that can profoundly change your life for the better. You deserve support in becoming your happiest, healthiest self—and help is available whenever you’re ready to take that next step. Find treatment options near you today.
