If you have attention deficit hyperactivity disorder (ADHD), you might feel like your emotions are on a roller coaster—intense joy one moment, frustration or sadness the next. This experience has a name: emotional dysregulation. It’s a common but often overlooked aspect of ADHD that affects how you process and express feelings.
Some people with ADHD say they feel like their emotions are “turned up to 11” while everyone else seems to operate at a 6 or 7. That intensity isn’t a character flaw or lack of willpower—it’s a difference in how your brain processes emotional information.
While neurodivergence is gaining visibility, people rarely talk about how emotional dysregulation can be as disruptive as better-known ADHD symptoms like inattention and hyperactivity. But with targeted strategies and support, plenty of ADHDers find ways to harness their emotional intensity and view it as a strength, not a limitation.
Let’s explore how you can do just that.
What Is Emotional Dysregulation in ADHD?
If your emotions are dysregulated, it means you’re having a hard time managing your feelings and returning to a calm state. It’s like having emotions that feel bigger and harder to control than those of neurotypical people.
Emotional challenges aren’t always discussed as core symptoms of ADHD in diagnostic criteria, but studies show that 34-70% of adults with ADHD struggle to control their emotions.1 For many people, deficient emotional self-regulation just as disruptive as feeling hyperactive or not being able to focus.
When you have ADHD and emotional dysregulation, you might:
- Feel emotions more strongly than situations seem to call for
- Switch quickly from one feeling to another
- Find it hard to calm down once you’re upset
- Struggle to put your feelings into words
- Have trouble shifting your attention away from things that upset you
This isn’t about being too emotional or overreacting. Your brain simply processes feelings differently, which makes it harder to use the mental tools that generally help people manage their emotions.
The good news is that more doctors and researchers are starting to recognize emotional dysregulation as an important feature of ADHD. “In the last 15 years or so, we’ve come to realize that emotion dysregulation is a key component of ADHD,”2 says psychologist and ADHD researcher Paul Rosen, PhD. This growing awareness means better understanding, and ultimately, more helpful approaches to treatment.
What Emotional Dysregulation Looks Like in Daily Life With ADHD
What does emotional dysregulation actually look like in everyday life? Here are some common examples:
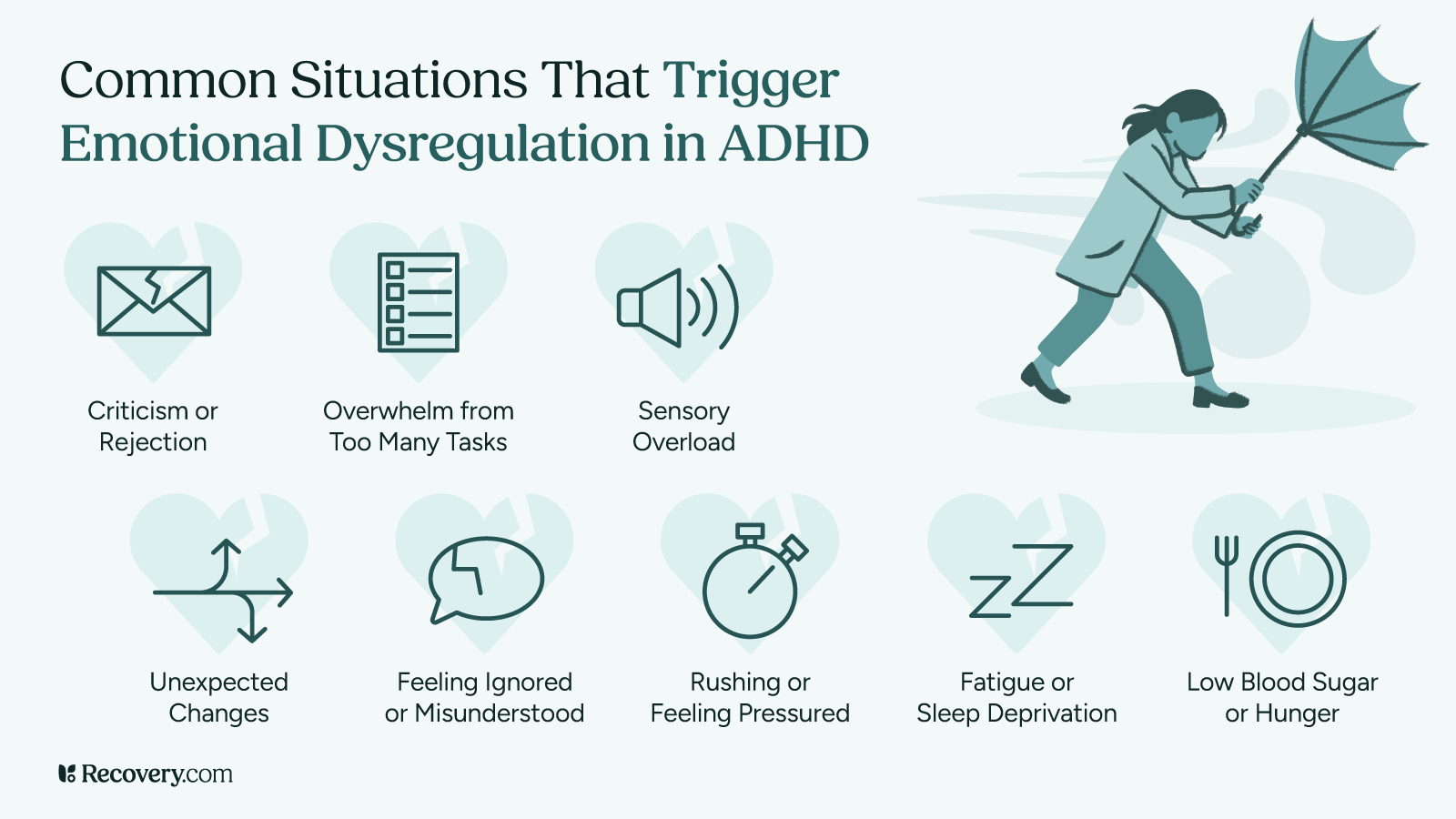
In adult ADHD,3 emotional dysregulation might appear as:
- Getting frustrated when plans change unexpectedly
- Feeling overwhelmed by criticism, even when it’s constructive
- Getting intensely excited and talking over people
- Having trouble letting go of perceived slights or rejections
- Feeling emotions so strongly that they interfere with your decision-making
For children with ADHD,4 it might look like:
- Having meltdowns that seem out of proportion to the situation
- Showing extreme excitement that’s hard to settle down from
- Getting discouraged easily when they’re dealing with challenges
- Reacting intensely to changes in their routine
- Struggling with transitions between activities
Emotional dysregulation is different from typical emotional responses because of its intensity, how quickly it arises, and how hard it is to return to a baseline state. Some people describe it as being overwhelmed by emotions that are too strong to handle using their regular self-soothing techniques.
Why People With ADHD Experience Emotional Dysregulation
The correlation between ADHD and emotional dysregulation5 has to do with brain function. It’s not a choice or a personality trait—it happens because of how your brain is wired.
In the ADHD brain, the areas responsible for controlling emotions (such as the amygdala and prefrontal cortex) don’t communicate as efficiently with the emotional centers. That means the feelings arise normally, but the brain’s braking system for those feelings doesn’t engage as quickly or effectively.
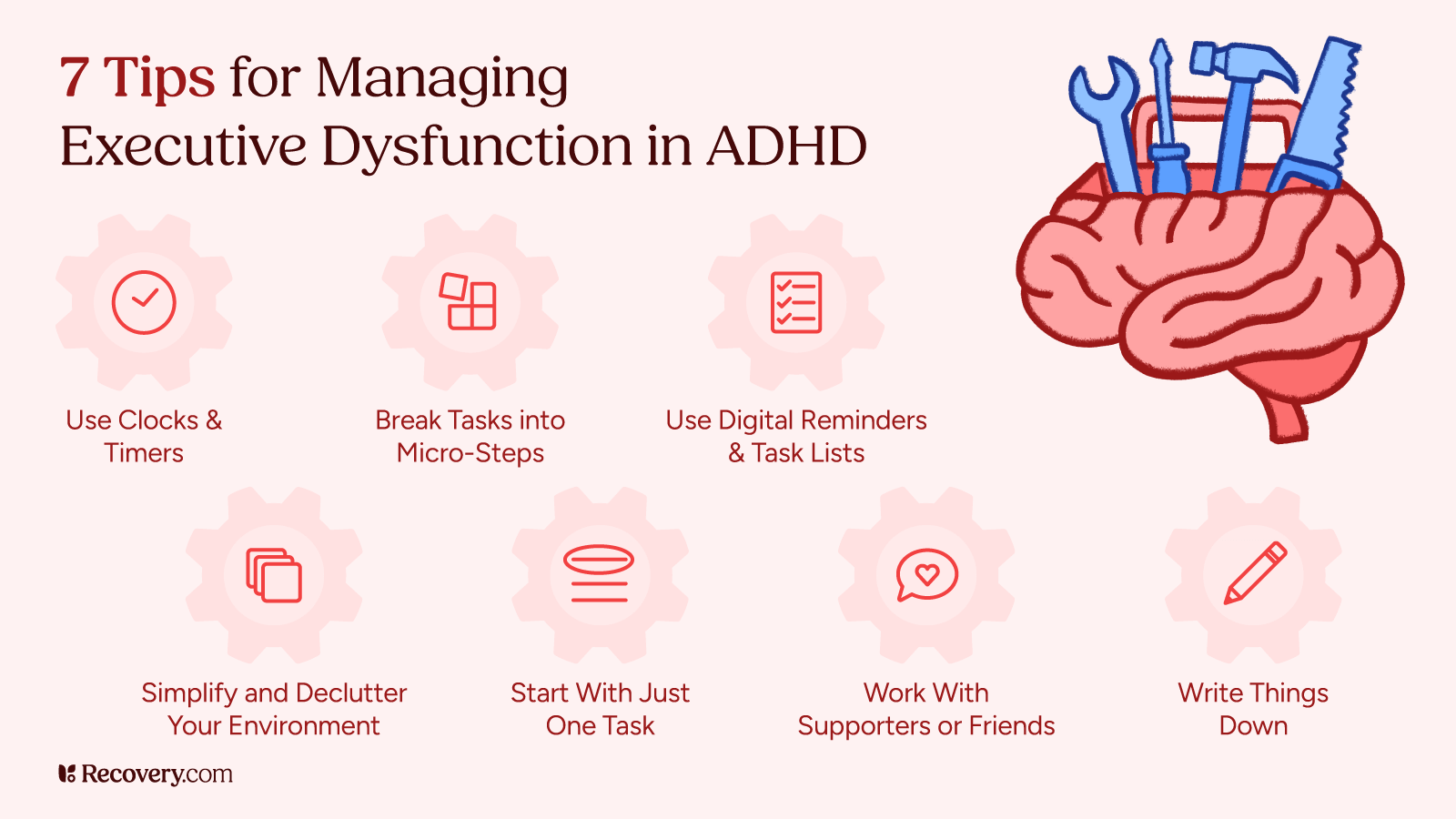
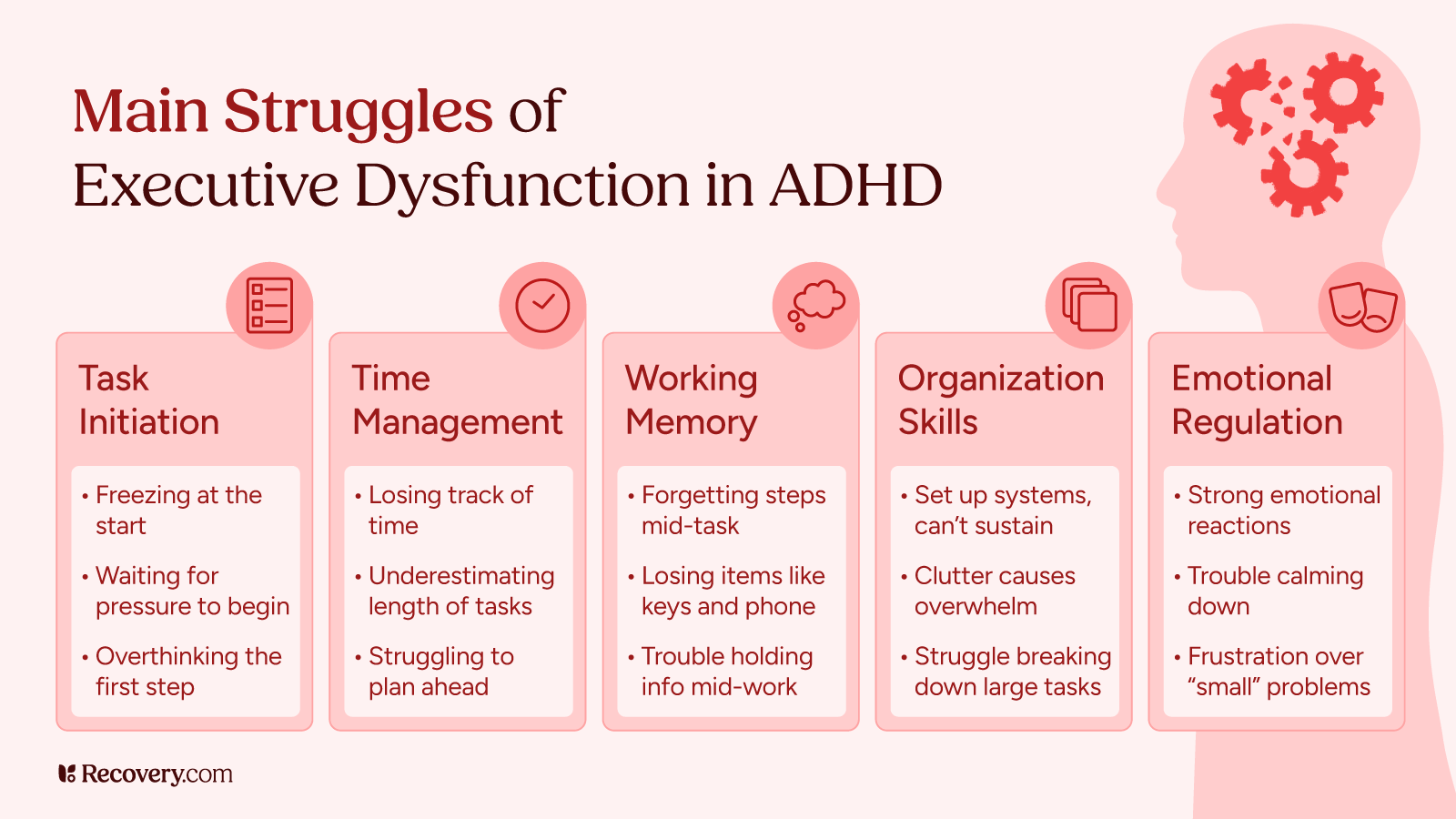
ADHD affects executive functioning:6 mental skills like working memory, flexible thinking, and self-control that play a major role in regulating your emotions. When your executive functions aren’t operating at full capacity, managing emotions is harder.
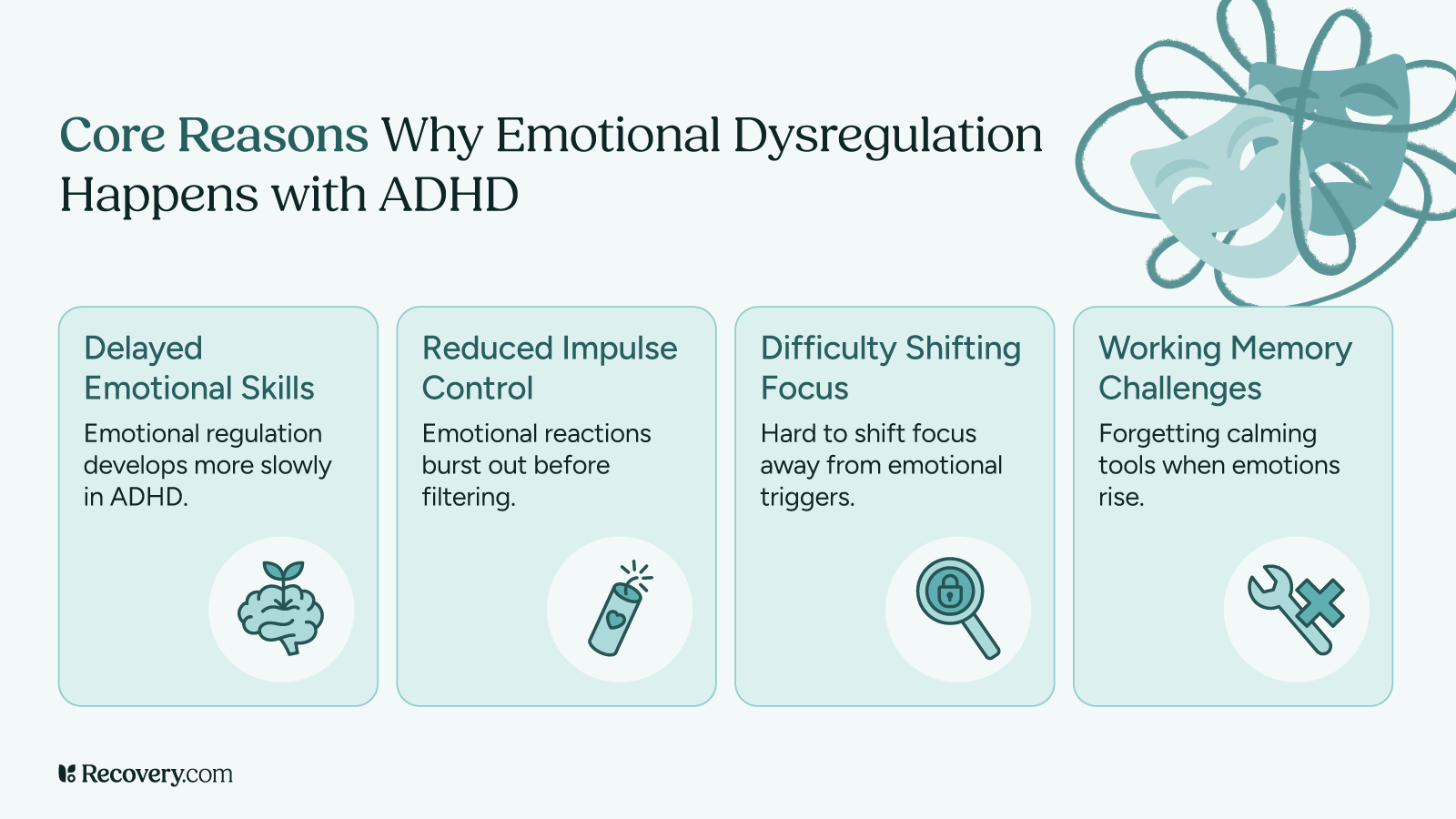
These key factors contribute to emotional dysregulation in ADHD:7
- Delayed development of emotional regulation skills: The ability to manage emotions develops more slowly in people with ADHD, which means you might still be working on skills that others developed earlier.
- Reduced impulse control: ADHD increases emotional impulsivity, meaning your emotional reactions may tend to come out before your brain has a chance to filter them.
- Difficulty shifting attention: Getting “stuck” on emotional triggers can make it harder to move past negative feelings (like when a small criticism replays in your head all day).
- Working memory challenges: Even when you know what helps calm you down, your brain might forget these tools right when you need them most.
Your upbringing also plays a role. Growing up with undiagnosed ADHD often means your caregivers frequently criticize or misunderstand you, which can make your emotional responses even more intense as a protective mechanism.
For more insight into how early experiences can impact emotional regulation throughout life, see our guide to healing from childhood trauma.
Treatment Approaches for Emotional Dysregulation in ADHD
If big emotions are making life harder for you, there’s good news! Several interventions can help. Most people do best with a mix of approaches that fit their specific needs.
Medication
ADHD medications8 help a lot of people get a better handle on their emotions. Stimulants like Ritalin, Concerta, Adderall, and Vyvanse work by boosting certain brain chemicals that help with focus—and often emotional control, too.
Non-stimulant options like Strattera, Intuniv, and Wellbutrin might also help some people manage emotional symptoms.
Note: Recovery.com does not give medical advice, and medication affects everyone differently. You should work with an ADHD-specialized mental health professional who can give you a thorough assessment and create a treatment plan accordingly. They can help you understand if medication might be helpful for your specific situation and monitor how it’s working for you.
Therapy Approaches
Several types of psychotherapy can be especially helpful:
- Cognitive behavioral therapy (CBT) helps you spot thought patterns that trigger strong emotions and teaches you healthier ways to think.
- Dialectical behavior therapy (DBT) focuses on specific skills for handling negative emotions, dealing with stress, and improving relationships.
- Mindfulness-based therapy teaches you to notice your feelings without immediately acting on them by observing your emotions without judgment.
Self-Management Strategies
There are also some things you can do on your own to manage your emotions better:
1. Know Your Triggers
Start paying attention to what sets you off. Learn how to recognize the patterns. Maybe it’s running late, feeling criticized, or even being hungry or tired. Keep a note on your phone about what happened before you got upset. Learning to recognize your patterns can help you avoid or prepare for these situations.
These tools can help:
- Tracking your moods, and what caused them, in a daily journal or mood tracking app
- Taking a self-assessment using a standardized questionnaire (like the SR-WRAADDS) to rate your emotional responses and regulation difficulties
- Scheduling regular check-ins with your therapist or a friend
2. Create Your Own Pause Button
Come up with a quick routine to use when you feel your emotions building. This could be as simple as taking a few deep breaths, stepping outside for a moment, or even just saying “let me think about that” before responding to someone. The trick is to put a little space between what happens and how you respond.
3. Build a Toolbox of Coping Skills
Different emotions might need different tools. When you’re angry, a quick walk and some deep breaths might help you burn off some energy. When you’re anxious, try the 5-4-3-2-1 method9 (name 5 things you see, 4 things you feel, and so on) bring yourself back to the present moment. Much of what you learn in therapy is building your internal resources to better cope with challenges in the future.
4. Be Kinder to Yourself
People with ADHD are often hard on themselves. Try talking to yourself like you would to a good friend who’s struggling. Instead of “What’s wrong with me?” you might try, “This is hard, but I’m doing my best.” How you talk to yourself10 plays a big role in your self-esteem.
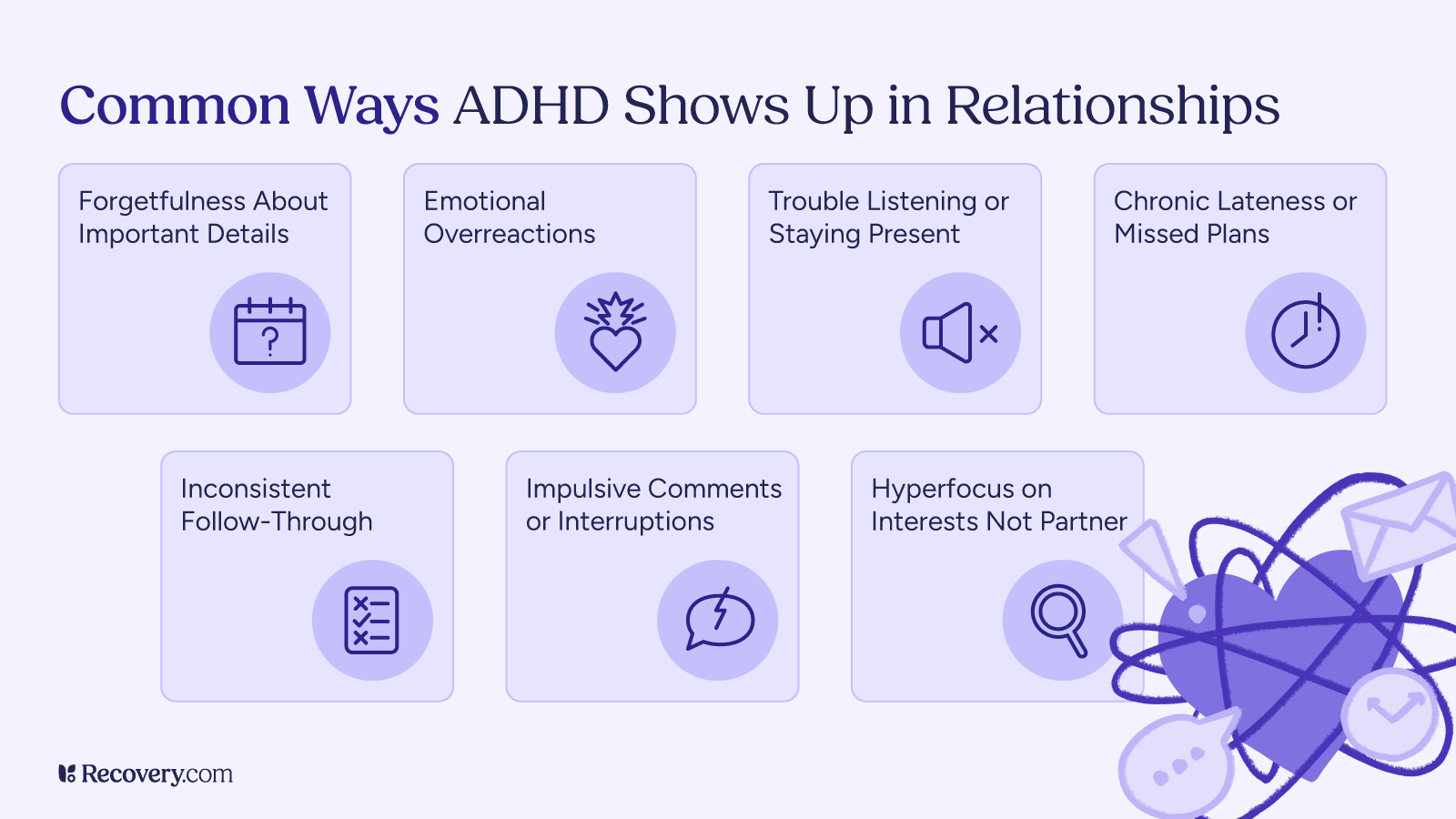
Ways to Support Someone With ADHD Emotional Dysregulation
If someone you care about has ADHD and struggles with big emotions, here’s how you can help:
- Just listen: When they’re upset, sometimes the best thing you can do is simply hold space without trying to solve the problem. Even if their reaction seems over-the-top to you, you can acknowledge how they’re feeling with something like, “I understand you’re really upset about this.”
- Don’t invalidate: Phrases like “calm down,” “you’re overreacting,” or “it’s not that big a deal” usually make things worse. They can feel dismissive and often increase frustration.
- Create a signal: Together, come up with a word or gesture that either of you can use when emotions start simmering. This gives your loved one a chance to use their coping skills before things escalate.
Take Care of You, Too
Supporting someone with mental health conditions can be draining. Make sure you’re looking after your own needs and setting healthy boundaries.
Learn more about maintaining your own well-being while supporting others in our article on how to honor your own needs and break free from codependent patterns.
It also helps to remind yourself that your loved one isn’t choosing to have big emotional reactions—this is a real part of ADHD that requires patience and understanding.
Embracing Your Emotional Range: Learn to Thrive With ADHD Emotions
Emotional intensity isn’t all bad. It can fuel creativity, passion, and deep connections when it’s channeled effectively. With support and practice, the emotional side of ADHD can become more manageable—and even become your superpower.
Remember, the goal isn’t to stop having feelings (they’re an essential part of being human!) but to express them in ways that work better for you and your relationships.
Reaching out for help is a smart move, and finding a provider who gets the emotional challenges of ADHD makes a huge difference. Our treatment finder lets you search for programs that match your needs—connect with an ADHD treatment provider today and start creating an emotional life that works for you.
FAQs
Q: What is an example of ADHD emotional dysregulation?
A: Someone with ADHD might overreact to minor frustrations—like snapping in anger when plans change unexpectedly or feeling devastated over small mistakes—due to difficulty regulating emotional responses.
Q: What helps emotional regulation in ADHD?
A: Mindfulness techniques, behavioral therapy, regular routines, and sometimes medication can help individuals better manage emotional ups and downs.
Q: How to treat emotion dysregulation?
A: Treatment typically involves a combination of cognitive behavioral therapy (CBT), skills training in emotional awareness, medication (like stimulants or antidepressants), and lifestyle changes that support emotional stability.
Q: What does emotional dysregulation look like?
A: It can appear as mood swings, impulsive outbursts, difficulty calming down after becoming upset, or feeling emotions more intensely than others might in similar situations.
Q: Is emotional dysregulation part of ADHD?
A: Yes, emotional dysregulation is not part of the core diagnostic criteria, but it is a common and clinically significant feature of ADHD, particularly in adults and adolescents.
Q: How is emotional dysregulation treated?
A: Besides therapy and medication, structured daily habits, emotional coaching, and support groups can provide effective ways to cope and improve self-regulation.
Q: When are adaptive strategies most predictive of psychopathology?
A: Studies show that the absence of adaptive emotional regulation strategies—especially during childhood or adolescence—can predict later development of mood disorders or anxiety, particularly in individuals with ADHD.
Q: Do inattention and hyperactivity symptoms equal scholastic impairment?
A: Not always, but they often correlate. These symptoms can disrupt focus, memory, and organization, leading to academic struggles, especially when emotional dysregulation is also present.
Q: How can mobile devices be optimized for users with attention deficit hyperactivity disorder?
A: Apps that promote task management, mindfulness, and structured reminders—along with distraction blockers—can support focus and emotion regulation in people with ADHD.
Q: What are some strategies to improve emotional regulation?
A: Deep breathing, journaling, practicing delay before reacting, naming emotions out loud, and using grounding techniques are simple but powerful tools to build better emotional control.
Q: Can emotional dysregulation in ADHD be managed with therapy?
A: Absolutely. Therapies like CBT and dialectical behavior therapy (DBT) are effective in teaching coping skills, emotional awareness, and self-regulation strategies.
Q: Can therapy help with emotional dysregulation in ADHD?
A: Yes—therapy provides a safe space to build emotional insight and practice tools that reduce the intensity and duration of emotional reactions.
Q: Can emotional dysregulation in ADHD lead to other mental health issues?
A: Yes, unmanaged emotional dysregulation may contribute to anxiety, depression, low self-esteem, and relationship difficulties over time.
Q: Can ADHD medication help with emotional dysregulation?
A: In many cases, yes. Stimulant and non-stimulant ADHD medications can help regulate attention and impulsivity, which in turn can reduce emotional reactivity and improve mood regulation.