Completing a treatment program is a major accomplishment, but it’s only the beginning. Addiction and mental health recovery is about more than abstinence or even symptom management. Long-term recovery requires planning, support, and new strategies for managing life outside of a structured environment.
This guide explores what comes next and how to build a sustainable path to well-being. Treatment is just the beginning of an exciting, new, and healthy life, one that is supported by personal growth and ongoing care.1
1. The Importance of Aftercare
What happens after discharge can make or break your recovery journey. Relapse rates or recurrence of use for substance use disorder are comparable to other chronic conditions, such as hypertension and type 2 diabetes. These conditions, like addiction, require ongoing care.
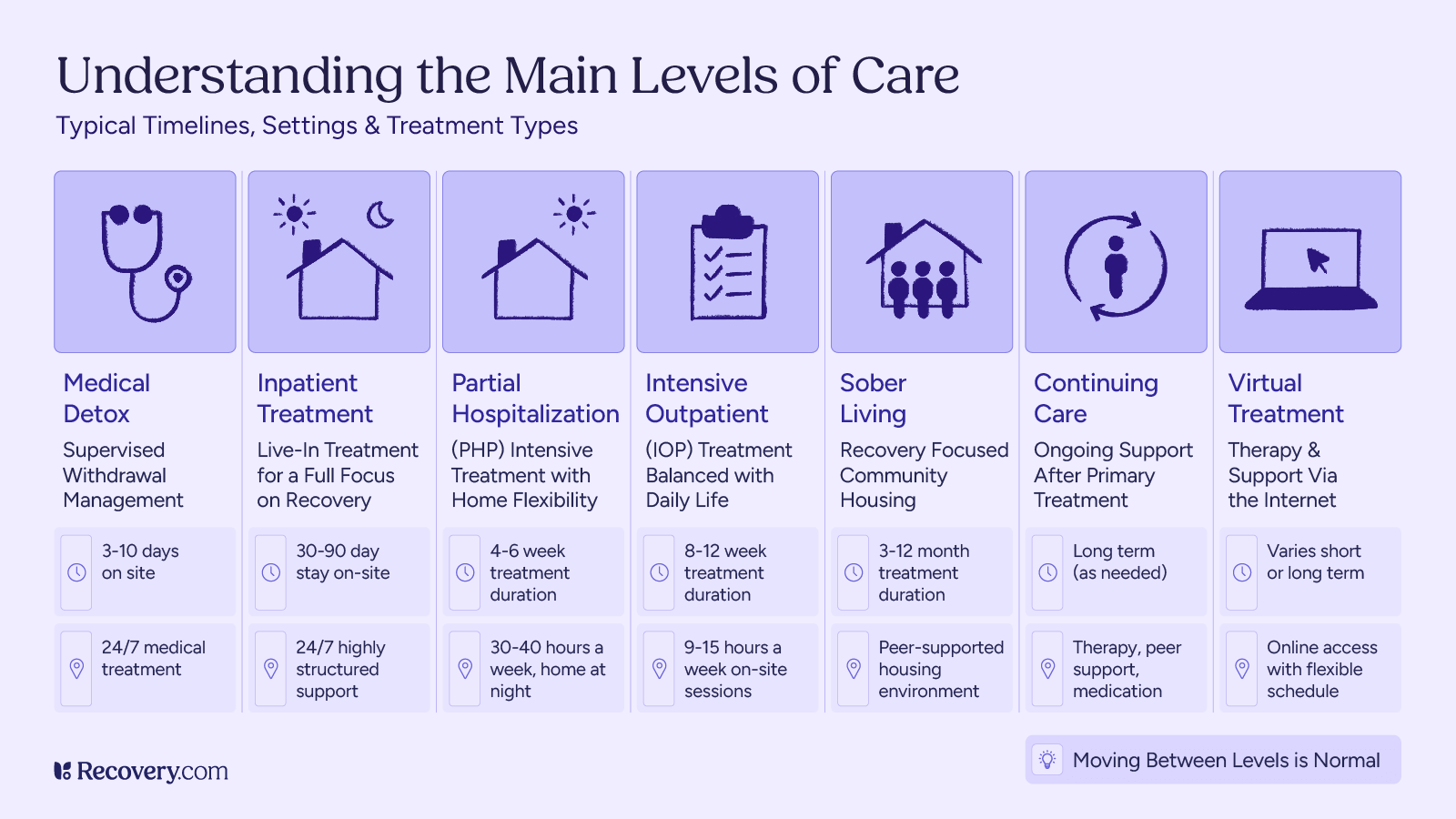
Aftercare refers to the structured support and treatment options that follow residential treatment or inpatient programs. Research shows that individuals who engage in aftercare services have higher abstinence rates and fewer relapse episodes.2 These services extend the recovery process by offering continued care,3 structure, and accountability as individuals transition back into everyday life.
Whether you’ve completed detox, inpatient rehab, or another form of substance use disorder treatment, an aftercare plan provides the scaffolding needed for long-term success.
You may also have experienced a relapse or recurrence of use. This can be a normal part of the recovery process. An important thing to remember is that you can always reconnect with your aftercare plan and continue your recovery journey no matter what setbacks occur.
Types of Aftercare Plans
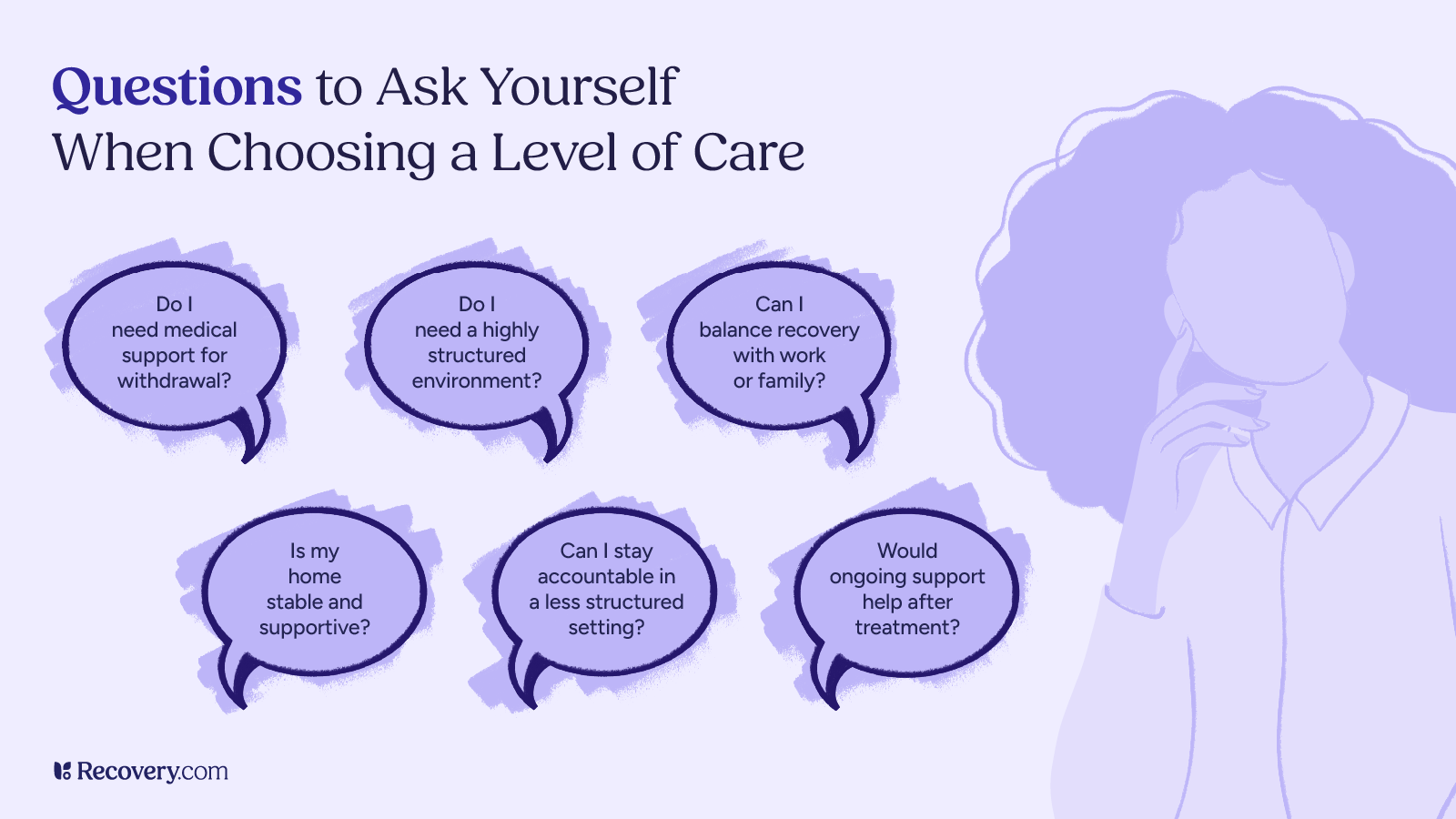
There is no one-size-fits-all recovery path.4 The most effective treatment plans are personalized based on your substance use history, mental health conditions, and social circumstances.
Common Aftercare Options Include:
- Outpatient therapy: Includes ongoing therapy sessions with a licensed mental health professional or addiction counselor. Cognitive behavioral therapy (CBT),5 trauma-informed care, and dialectical behavior therapy (DBT) are evidence-based approaches that can reduce relapse risk and enhance coping skills.
- Intensive Outpatient Programs (IOPs): These structured programs6 offer therapy and group support several times a week without requiring overnight stays, helping bridge the gap between inpatient care and independent living.
- Sober living homes: Transitional residences for individuals in recovery. These environments support a drug-free lifestyle and promote peer accountability,7 reducing the risk of early relapse.
- Recovery coaching: One-on-one support from a trained peer who offers lived experience, goal setting assistance, and motivational guidance. Recovery coaching is increasingly recognized as an effective form of community-based support.
- Medication-assisted treatment (MAT): For those with opioid or alcohol use disorder, medications like methadone, buprenorphine, or naltrexone8 can reduce cravings and support recovery. MAT has been shown to reduce overdose risk and improve long-term outcomes.
Aftercare should be initiated before discharge, with referrals made by healthcare providers or treatment centers to ensure continuity of care.
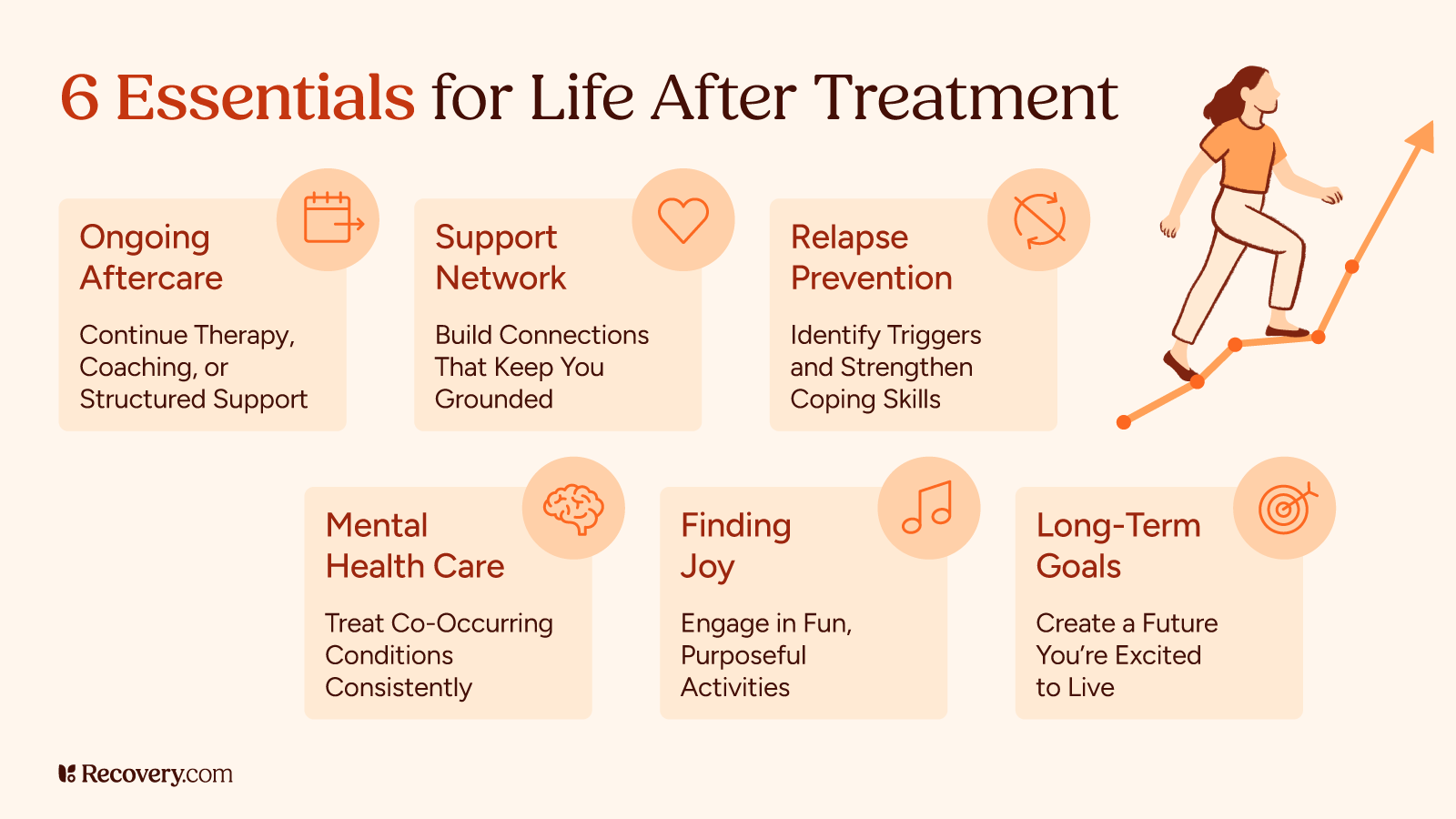
2. Building a Support Network
No one recovers alone. A strong support system improves mental health, lowers relapse risk, and offers a sense of belonging during difficult times.
Recovery Support May Include:
- Sponsors and mentors: Individuals in long-term recovery who guide and support you through 12-step programs like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA). These relationships offer accountability and shared experience.
- Alumni groups: Many treatment centers host alumni events and meetings to help former clients stay connected and inspired.
- Family involvement: Family therapy helps loved ones understand addiction, rebuild trust, and become active allies in recovery. Evidence supports family therapy as a tool for improving communication and reducing substance use.
- Online communities: Virtual meetings,9 support forums, and recovery apps can provide round-the-clock encouragement and connection.
3. Relapse Prevention Strategies
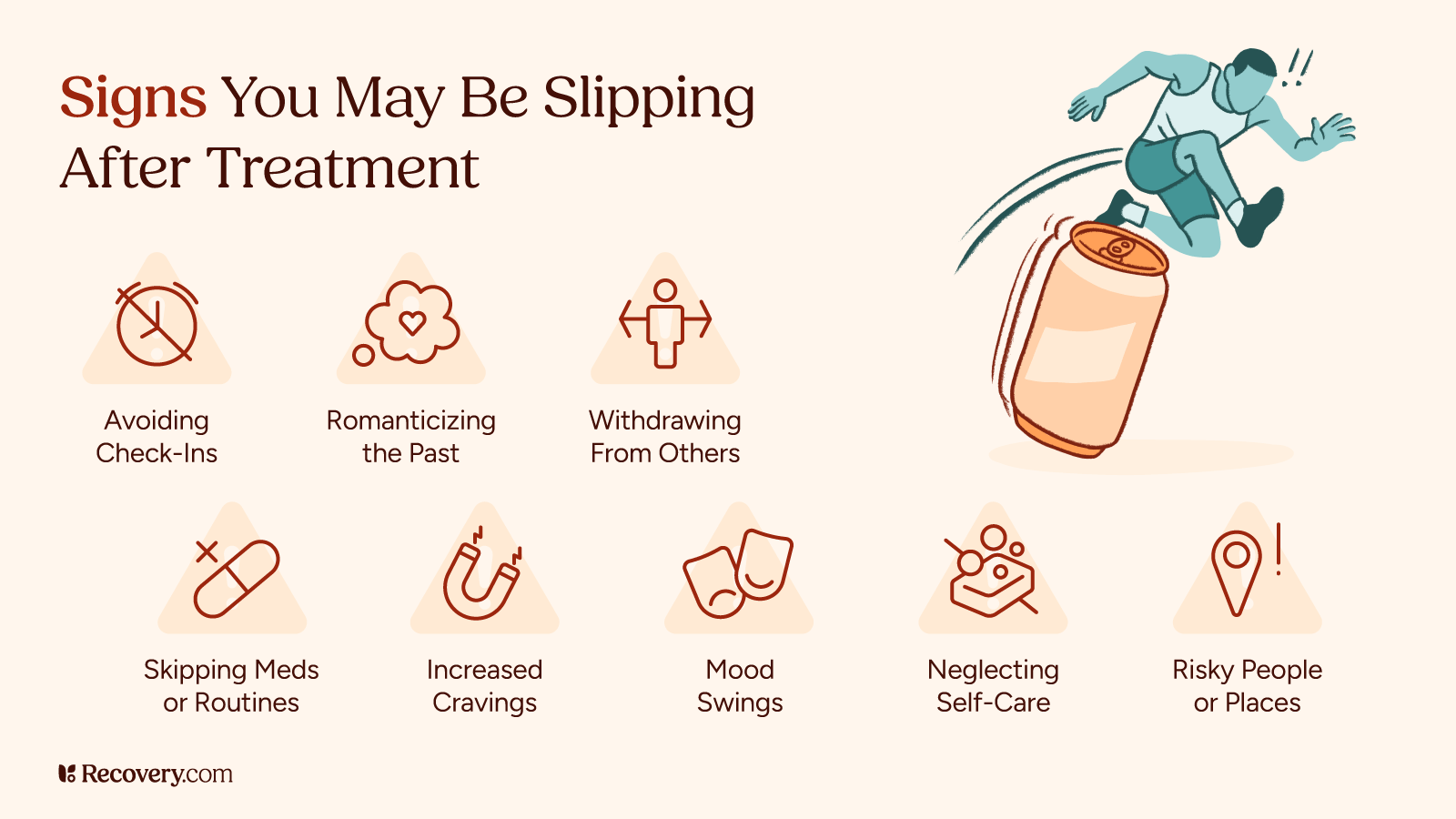
Preventing relapse isn’t just about avoiding drugs or alcohol—it’s about recognizing what leads to cravings and having tools ready to respond. The American Society of Addiction Medicine emphasizes the importance of proactive relapse prevention planning in sustaining recovery.
Core Relapse Prevention Tools:
- Trigger identification: Learn what situations, emotions, or environments increase your risk of substance use. Triggers may include stress, isolation, boredom, or reconnecting with old social circles.
- Coping mechanisms: Practice evidence-based strategies such as mindfulness, breathing techniques, journaling, and physical activity. These approaches have been shown to reduce anxiety and improve emotional regulation.10
- Accountability systems: Regular check-ins with sponsors, recovery coaches, or behavioral health professionals help you stay grounded and committed.
- Emergency plans: Create a “lifeline” contact list of trusted people you can reach out to when struggling. Have a plan for how to manage high-risk situations and cravings.
If a relapse does occur, it’s important to seek support and adjust your recovery plan. Relapse is not failure—it’s an opportunity for learning and recalibration.
4. Staying Connected to Purpose
Recovery isn’t just about what you leave behind, it’s about what you move toward. Rediscovering or creating meaning in your life provides long-term motivation and strengthens your identity beyond addiction.
Ways to Reclaim Purpose:
- Volunteering or service work: Studies show that helping others11 can reduce depressive symptoms and improve life satisfaction.
- Pursuing education or skills training: Reengaging with learning fosters self-efficacy and goal-setting.
- Spiritual or religious practice or mindfulness: Spirituality and mindfulness-based interventions like yoga or meditation have been shown to support recovery and reduce relapse risk.
- Goal setting: Establishing short- and long-term goals helps you track progress, stay motivated, and shape a positive vision of your future.
Rebuilding relationships, embracing new interests, or engaging in creative expression can all play a role in nurturing your recovery identity.
5. Managing Mental Health Long-Term
Many individuals in recovery also live with co-occurring mental health disorders such as depression, anxiety, PTSD, or bipolar disorder. Treating these conditions is essential to maintaining stability and avoiding relapse.
Key Mental Health Strategies:
- Medication management: Work closely with your healthcare provider to monitor prescriptions, especially if you’re taking medications for mood, anxiety, or medication-assisted treatment.
- Routine check-ins: Consistent appointments with a licensed mental health professional can catch emerging issues before they escalate.
- Lifestyle habits: Sleep hygiene, balanced nutrition, regular exercise, and creative or spiritual outlets all support mental wellness.
- Ongoing therapy: Continued engagement in evidence-based therapy (e.g., CBT or trauma-informed approaches) fosters long-term emotional resilience and healing.
If you or a loved one needs additional support, visit Recovery.com.
6. Embrace Joy and Live Life to the Fullest
Recovery isn’t just about avoiding what hurts, it’s about discovering what lights you up. Fun, play, and new experiences are not only allowed in recovery—they’re essential.
Rediscovering joy can help reinforce the value of staying sober, reduce stress, and reconnect you with a sense of purpose beyond survival. Studies show that engaging in positive leisure activities can improve emotional regulation, reduce depressive symptoms, and increase life satisfaction for people in recovery.
Ways to Add Fun to Your Recovery Life:
- Try something new: Join a hiking group, take a cooking class, or explore local art or music scenes.
- Laugh often: Watch comedies, play games, or surround yourself with people who bring out your playful side.
- Celebrate your wins: Acknowledge milestones, no matter how small. Treat yourself to sober rewards.
Travel or explore: Even a weekend trip or a walk in a new park can break routine and spark joy. - Stay curious: Reignite your creativity through hobbies like painting, writing, dancing, or DIY projects.
Joy is not a luxury in recovery—it’s part of the medicine. The more you engage with life fully, the more recovery becomes a life worth staying in.
A Lifelong Journey
Recovery is not a destination; it’s a lifelong process that evolves with you. Life after treatment is filled with choices—some easy, some hard—but with a solid aftercare plan, community support, and a commitment to growth, lasting recovery is possible.
Whether you’re managing cravings, rebuilding relationships, or adjusting to life outside residential treatment, know this: your story is still being written, and help is always available.
Explore trusted mental health programs that offer long-term care, flexible options, and evidence-based approaches tailored to your needs.
FAQs
Q: What is the most effective mental health treatment?
A: The most effective treatment varies based on the diagnosis and individual needs. However, evidence-based approaches like cognitive behavioral therapy (CBT), medication management, and integrated care models have proven effective across a range of mental health conditions. Combining therapy, lifestyle changes, and social support typically leads to the best outcomes.
Q: What is the next step after rehab?
A: After completing rehab, the next step is engaging in a structured aftercare plan. This may include outpatient therapy, sober living arrangements, support groups, recovery coaching, and ongoing medical or psychiatric care. These steps help maintain progress and reduce the risk of relapse.
Q: What is the most successful treatment for addiction?
A: The most successful treatment often combines medication-assisted treatment (MAT) for conditions like opioid or alcohol use disorder, behavioral therapies, and peer support. Long-term success is linked to individualized care, consistency, and engagement in recovery support services.
Not sure how to find the best treatment for you? Read more here.
Q: What are the types of substance use disorder?
A: Substance use disorders can involve different substances, including alcohol, opioids, stimulants, cannabis, sedatives, and hallucinogens. Each type varies in severity and may require specific treatment approaches based on the substance used and the individual’s mental health history.
Q: What is substance abuse treatment?
A: Substance use disorder treatment is a structured approach to helping individuals stop or reduce harmful substance use. It may involve detox, inpatient or outpatient care, therapy, medication, and peer support. Treatment plans are typically customized to address both addiction and any co-occurring mental health conditions.
Q: Can I force my family member into treatment?
A: In some states, involuntary treatment is possible under specific legal criteria if the person poses a risk to themselves or others. However, voluntary engagement in treatment is generally more effective. Encouraging open dialogue, expressing concern, and offering support can sometimes motivate a loved one to seek help.
Q: Did the substance abuse treatment fail because of complications from your mental health issue or vice versa?
A: Co-occurring disorders can complicate recovery if not treated simultaneously. If mental health issues go unaddressed, they can contribute to relapse. Integrated treatment that addresses both substance use and mental illness improves the chance of lasting recovery.
Q: Does relapse to drug use mean treatment has failed?
A: No. Relapse is a common part of the recovery process and does not mean failure. It often indicates that the treatment plan needs to be adjusted. Ongoing support, re-engagement in care, and learning from relapse experiences are key to moving forward.
Q: How do behavioral therapies treat drug addiction?
A: Behavioral therapies like CBT, contingency management, and motivational interviewing help individuals change harmful thought patterns, build coping skills, and reinforce positive behaviors. These therapies are often used alongside medication and peer support to address the root causes of addiction.
Q: How can I maintain my mental health and sobriety after treatment?
A: Maintaining recovery includes regular therapy, support group participation, medication adherence (if prescribed), and consistent self-care. Healthy routines, stress management, and a strong support network also play vital roles in preventing relapse and sustaining mental wellness.
Q: How can I support my recovery journey after completing addiction treatment?
A: You can support your recovery by staying connected to your support system, setting meaningful goals, attending follow-up appointments, practicing mindfulness, and engaging in activities that bring purpose. Recovery is a lifelong journey, and maintaining motivation is key to long-term success.