Rehab is just the first step in making long-term changes to your lifestyle. Because many people choose to go to rehab in response to a crisis, it’s easy to approach this process with a sense of urgency. In the moment, that urgency is warranted. However, when you’re so focused on the short term, it can be difficult to imagine a better future. People tend to catastrophize, picturing themselves going through crisis after crisis, and this emotional spiral can lead to poor decision-making.
Preparing for hard times is helpful, but catastrophizing is not. You are a dynamic, learning, growing person. And the more time you spend focused on healing, the more tools you will develop to navigate any hardship that comes your way.
After rehab, it’s natural to be concerned about relapsing. And that’s understandable, because relapses do happen. But they’re not the end of the world. By the time you leave rehab, you’ll be prepared to work through these setbacks. Nearly 75% of people who experience addiction ultimately recover.1 This includes people who experience relapses.
The process of preventing a relapse begins the moment you enter rehab. Addiction treatment providers understand that your goal isn’t just to complete the program, it’s to successfully reenter the world and live a sustainably healthy life. Your experience of rehab will prepare you for what comes next.
Relapse is a valid concern for many clients. That’s why so many good-quality rehabs focus on giving you the tools you need to work through it.

What Causes Relapse?
Stress
Stress is a natural part of life, and research shows that people with a history of addiction may be more sensitive to stress. Even positive events can be stressful,2 like getting a promotion or planning a wedding. The goal isn’t to eliminate these triggers, but to manage them in a healthy way.
Following rehab, stress can make you vulnerable to relapse.3 That’s because there’s a well-understood link between stress and addiction4—and this is especially true of chronic stress. Many people first turn to substances in response to difficult life situations. And without strong coping mechanisms, it’s easy to fall back into those unhealthy patterns. During rehab, you’ll learn how to manage your responses to stressful situations.
Although mindfulness is something of a buzzword these days, it’s also an effective tactic for coping with stress. This and other emotion regulation techniques taught in rehab can help you focus on the issue at hand, instead of getting lost in a series of overwhelming reactions.
Unexamined Trauma
Don Lavender, Program Director of Camino Recovery in southern Spain, explains the impact of unresolved trauma on relapse:
“The biggest contributor to relapse is stress, and the biggest contributor to stress is unaddressed or unresolved trauma.”
Trauma can result from any number of things, and no two people have the same experience. One person might develop PTSD from a car accident, while another walks away with no lasting psychological effects. Ongoing trauma, such as an abusive relationship or a toxic living situation, can result in complex PTSD (CPTSD), which has slightly different symptoms than PTSD.
With either of these conditions, it’s quite common to develop triggers. A trigger is an experience that evokes feelings of the original trauma, which are often disproportionate to the present moment. For example, open flames might trigger a person with PTSD from a house fire. When they see a burning candle, they may feel a sense of fear and urgency or even rush to put out the flame. In life, this isn’t always an appropriate response. That’s why, in healing from PTSD and CPTSD, clients are encouraged to pinpoint their triggers and develop more effective coping mechanisms.
Substance abuse is a common response to triggers5 like these. When you feel frightened or hurt, substances can short-circuit your emotional state. However, mind-altering substances are just tools, and each one of them has a specific effect. And when substances are the only tool you have available, it makes sense that you would try to use them to fix emotional problems. That’s why rehab is designed to give you more tools, so you can always use the right one for the task at hand.

How to Plan Ahead
Rehab is designed to give you the resources you need to not only guard against relapse, but to deal with it when it happens. Many people have concerns about transitioning out of rehab and back into their regular lives. It’s important to remember that rehab is not a vacation; it’s more like a class. You won’t be expected to go back to your old routine when you finish the program. In fact, your experience in rehab will help you decide how to change that routine in order to prioritize your long-term health.
By the time you decide to go to rehab, you probably already know that your habits need to change. Your team of healthcare providers understands this, and they want to help. The process of planning for your reentry into the wider world begins the moment you enter the program, says Rowland Tweedie, the Health and Fitness manager at Paracelsus Recovery:
“Often I tell clients their job, in that initial period after the treatment, is them: it’s their health, it’s their wellbeing. We should plan that…It’s important to have local support in place.”
Planning for life after rehab is different for everyone, and your providers will help you come up with strategies that fit your needs. Some clients find it helpful to create an emotional first aid kit, in which they write down strategies to employ in the future. It can be difficult to think clearly during times of extreme stress, and this is one way to remind your future self of the tools you have available. For example, an emotional first aid kit might include the following:
- The phone number of your therapist or sponsor
- A list of activities you enjoy, like cooking or exercising
- A list of distress tolerance skills you learned in therapy, such as listening to a song you love, lighting a scented candle, or holding an ice cube in your hand
- A comfort object, like a soft pillow or a worry stone, that you can pick up and hold in the moment
- A mantra you can repeat to yourself during meditation
Rehab is a valuable opportunity to learn from experts, and many programs include educational components. You might learn about the root causes of addiction, including biological predispositions, risk factors in your upbringing, and co-morbid diagnoses. Many rehab centers offer skills coaching, equipping you with healthy habits intended to improve your quality of life. You might learn how to exercise properly, how to cook, or even how to paint. Craving management classes provide strategies for working through any urges you experience in the future.
This type of learning is extremely important, and you’ll ideally come away from it with many useful coping strategies. However, finishing rehab doesn’t mean you’re simply “fixed.” When you exit the program, you’ll begin a whole new learning process. The environment of a rehab facility is very different from the wider world, and it will take you time to reacclimate. There will be times when you’re overwhelmed and unsure of how to react to a new situation. Each of these moments is an opportunity to put your new skills into practice.

Life After Rehab
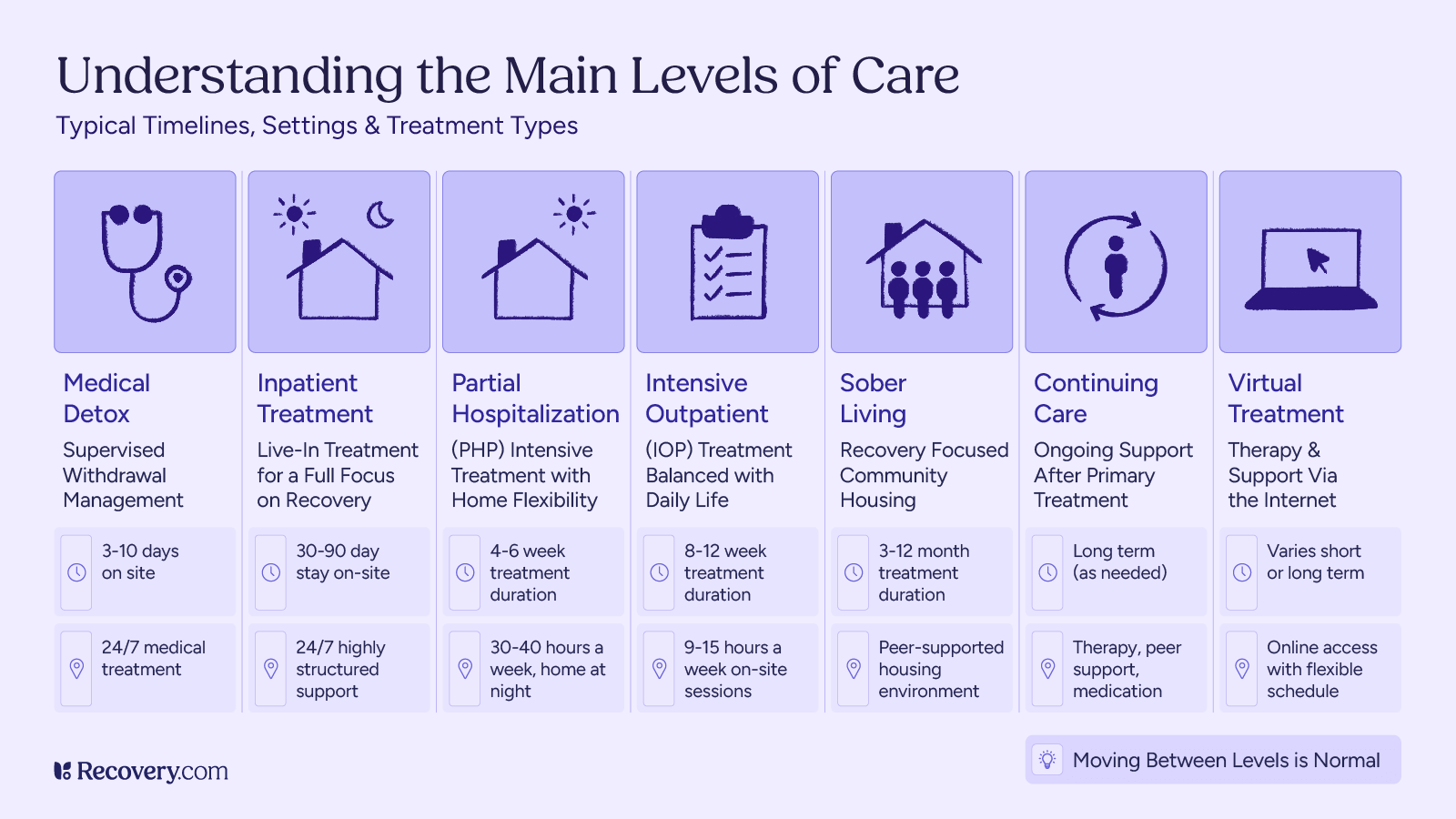
By the time you leave rehab, you’ll have a very specific plan in place for aftercare. Although the transition may be jarring, your team will work with you to make it as seamless as possible. Most clients make plans for continuing care, which may be ongoing or may just see them through the transitional period. These services may be offered by your original treatment facility, or you may work with a different provider after you complete the program. Certain types of care may be covered by insurance, but that’s not universally true.
If you traveled to a destination rehab center, you can still find providers that will be locally available when you return home. This may take a little more effort on your part, but it’s important to at least begin the process before you finish the program. You’ll want to have ground support as soon as you arrive, so that your new team can help you process the move to a new place. At this point, you’ll also be navigating brand new big changes. You may need to restructure your relationships, move to a new home, or change careers. It’s far easier to do this with a team standing by to support you in person.
Continuing care refers to any type of support that sustains your ongoing recovery. Components of continuing care may include the following:
- Individual therapy
- Psychiatry
- Group therapy
- Support groups (12-Step programs, harm reduction meet-ups, etc.)
- Work with a nutritionist
- Personal training and exercise
- Massage therapy or acupuncture
- Family support (family of origin or chosen family)
- Community support (friends and loved ones)
- Recreational groups (hiking groups, sports teams, fan clubs, knitting circles, etc.)
Any or all of these types of care may be appropriate for you. And remember that healing can be fun! Joy and passion are essential components of recovery. Taking pride in your accomplishments—whether a big presentation at work or a doodle of your cat’s face—allows you to find meaning in your daily life. It’s also important that you find healthy and sustainable ways to unwind. As you transition out of your old lifestyle, it can be difficult to imagine having fun without using substances. But don’t be afraid to try new things. There are countless ways to enjoy yourself, and you may be surprised to find you have much more fun when your head is clear.
Responding to Relapse
Relapses happen. Even when you have new skills, a strong support network, and the very best of intentions, this is a risk that you’ll face during recovery. Remember that relapse is not a sign of weakness, and it doesn’t have to be a failure. As Dr. Christine Merzeder, Senior Clinical Coordinator at Paracelsus Recovery, explains:
“When [you] relapse, there’s no moral issue with that. We say, ‘Okay, back to square one.’ If you relapse, phone us, come back to us. We give you advice on what to do. Don’t panic.”
If you do relapse, start by reaching out to a trusted healthcare provider. This could be someone you see regularly, like a local therapist or psychiatrist, or you can call the facility where you started treatment. Don’t isolate yourself or get lost in feelings of shame. There is a strong link between shame and addiction,6 and hiding your struggles often amplifies them.
Remember that this is a relapse. That means you’ve been here before, and you’ve gotten help before. You already have the tools you need to start or restart the healing process. You are living proof that change is possible. Some rehabs offer programs specifically for people who have relapsed after treatment. Depending on where you go, you may be able to return to the same place for a shorter stay. If that’s not available to you, you might also consider an Intensive Outpatient Program (IOP) in your area. In an IOP, you would continue to live at home, attending regular therapy sessions and workshops at a local treatment center.
Healing is a holistic process. If you’re considering rehab as an option, you probably already understand that substance abuse can have an impact on every area of your life. This might include your job, your family, your social life, and even your physical health. The goal of rehab is not just to heal your mind; it also aims to empower you to make big changes to the structures around you. You’ll have to reexamine the way you relate to the world, and take steps to make your life more sustainable. Don’t be daunted by this process. With every positive change, you’ll build momentum. This is true even during setbacks. If you relapse, remind yourself how far you’ve already come.
Lasting change is a long, slow process. The Stages of Change model7 lays out the many steps that go into this process, from precontemplation to ongoing maintenance. Most notably, this model includes relapse as a distinct possibility. Alex Lickerman, M.D., writes:
“Never let a few days, or even weeks, of falling back into bad habits discourage you from fighting to reestablish the good habits you want. Always remember: No one was born with habits. They were all learned, and can all, therefore, be unlearned.”
Relapse is just one step in a lifelong journey. It may feel like a step backward, but it’s also an opportunity to learn more about yourself. Pain of any kind—be it emotional, physical, or spiritual—is just information. When you touch a hot stove, you learn not to do it again. The lessons of relapse are more complex. You may learn that a particular relationship is causing you harm, or that you need to pay more attention to your sleep schedule. Any information about yourself is valuable. This learning process empowers you to build a life aligned with your values.
Remember: the path to healing isn’t linear. Whether you’re recovering from a broken ankle or emotional trauma, setbacks are to be expected. If you can, let these experiences motivate you. Listen to yourself, understand your needs, and focus on doing the next right thing.
If you’re in need of support, many rehabs offer programs that can help. Search for a facility based on your criteria and speak directly with an admissions advisor about the best course of action for you.