Seeking professional help for addiction is a brave and important step toward healing. But when you’re starting recovery, you might encounter an unexpected hurdle: a waitlist for admission into rehab.
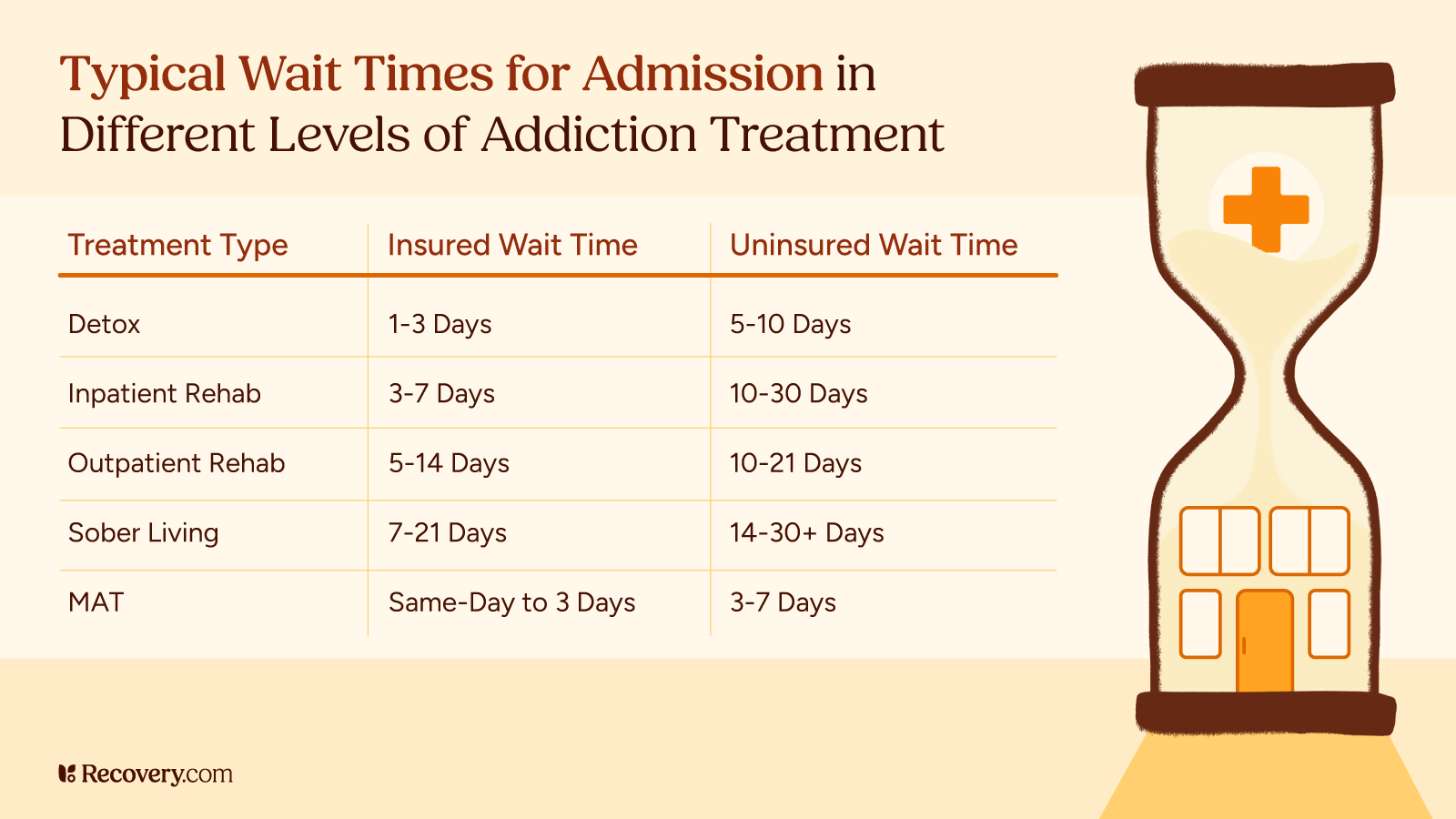
Depending on the location, the size of the center, and their staff capacity, certain rehabs may not have immediate availability. This is also due in part to an increasing demand for addiction treatment. As a result, there may be a waiting period before you can start the program of your choice.
Addiction recovery is an urgent need, and intervening early is important for your treatment outcomes. So what can you do if you’re facing a waitlist?
Use these strategies and resources to access support and maintain your progress on your path to healing:
While You Wait: Evaluate Your Needs
Assess the Severity of the Situation
Understanding the severity of your situation helps you make informed decisions and find appropriate support. Here are 2 approaches:
1. Professional Assessment
Ask for an assessment from your primary care doctor or therapist. Admissions staff at rehabs usually provide a brief intake screening over the phone, even if you can’t be admitted immediately. This evaluation might involve discussing your substance use history and assessing for co-occurring conditions.
2. Self-Assessment
Reflect on your experience with addiction. Consider factors like the frequency and intensity of your substance use, the impact it has on your daily life (your relationships, work, and health), and any withdrawal symptoms you have. Use reputable online resources like the National Institute on Drug Abuse’s screening tools to gauge your level of need.
While self-assessment is a good starting point, a professional assessment can provide a more accurate and in-depth picture of your situation. Use the information from your assessment to guide your search for immediate support while you wait for rehab placement.
Take Immediate Steps for Safety and Support
If you can’t get into treatment right away, you’ll still need to prioritize your safety and minimize potential harm. Here are some steps you can take:
Implement harm reduction strategies. Explore harm reduction strategies specific to your addiction. This might involve switching to safer alternatives, using designated use spaces, or carrying naloxone (if applicable) to reverse opioid overdoses.
Connect with crisis support. If you experience intense cravings or thoughts of self-harm, reach out to crisis hotlines like the National Suicide Prevention Lifeline (988) or the Crisis Text Line (text HOME to 741741) for immediate addiction support.
Inform people you trust. Share your situation with a close friend, family member, or therapist who can offer support and intervene if necessary.
Practice self-care. If you can, try to eat well, get adequate sleep, and try techniques like urge surfing1 to help you manage cravings.
Alternatives to Traditional Inpatient Rehab
While waitlists for inpatient rehab are frustrating, exploring other support options can be incredibly beneficial.
Outpatient Programs
These programs offer a structured and supportive environment for recovery without requiring a full-time residential stay.
Outpatient programs involve regular sessions with therapists, counselors, and support groups. These sessions address the core issues of addiction, provide healthy coping tools, and teach relapse prevention skills. The frequency and intensity of these sessions vary depending on the specific program and your individual needs.
Compared to inpatient rehab, outpatient programs offer more flexibility, allowing you to continue working, going to school, and fulfilling your other essential responsibilities. This can be especially useful for people who may not have the option of leaving their daily lives for an extended period.
Outpatient programs are not a substitute for inpatient care in all situations. But they can be a useful tool for managing your addiction while waiting for a spot in a residential facility. It’s also common for people to step down to an outpatient program after completing inpatient rehab to maintain their continuity of care, prevent relapse, and get support for long-term recovery.
Online Therapy and Support Groups
The digital world offers valuable resources for immediate support while waiting for inpatient rehab. Online therapy and virtual support groups can provide helpful connection and guidance during this critical time.
Online Therapy
Numerous online platforms connect patients with licensed therapists who specialize in addiction treatment. These sessions take place via virtual meetings, phone calls, or chat, and are an accessible way to receive professional support while staying home. Online therapy can help with various aspects of your recovery journey:
- Identifying triggers and developing coping mechanisms
- Managing withdrawal symptoms and cravings
- Building self-esteem and motivation
- Addressing co-occurring mental health conditions
Virtual Support Groups
Online support groups provide a safe, confidential space to connect with people who share similar struggles. These communities provide a range of benefits:
- Emotional support and encouragement
- Sharing experiences and coping strategies
- A sense of acceptance and belonging
Online resources are a great way to complement primary addiction treatment, but they shouldn’t replace professional, in-person care. They’re an additional tool in your toolkit to stay on track toward your recovery goals, before and after treatment.
Community Resources for Addiction
Your community is also a valuable resource to support you while you wait for rehab. Look for these options:
- Free support groups: 12-Step organizations like Alcoholics Anonymous (AA), Narcotics Anonymous (NA), and Al-Anon host free support groups for people struggling with addiction and their loved ones. You can also look into non-12-Step groups like SMART Recovery.
- Harm reduction programs: These programs offer practical support and resources to help people manage the risks of addiction, including advice on safer substance use and Narcan training.
- Community mental health centers: Some government-funded centers offer services like individual and group therapy, medication management, and case management, often at affordable rates or on a sliding scale.
Leverage Your Support Network
Your existing support network is a source of strength and stability. Don’t be afraid to lean into it during this challenging time.
Addiction can strain relationships, and mental health struggles can put us in a place where we’re afraid to ask for help. Use these steps to get the social support you need:
- Identify your support system. Confide in close friends and family members who understand what you’re going through and are willing to offer non-judgmental support.
- Communicate your needs. Openly share your situation and challenges with trusted people in your support network. Be specific about what kind of support you need, whether it’s emotional encouragement, practical help, or simply someone to listen.
- Set boundaries. It’s okay to let people know when you need space or time alone. Communicate your needs clearly and respectfully.
By tapping into these connections, you can navigate your wait time with more resilience and stay focused on your recovery goals.
Stay Engaged in the Recovery Process
Develop Healthy Habits
Even before rehab, cultivating healthy habits can benefit your healing progress. These positive changes not only help you manage cravings and stress, but also lay the groundwork for long-term well-being.
- Get some rest. Addiction is hard on your mind and body. It can also interfere with your ability to sleep. Finding ways to get your sleep schedule on track can set you up for success in recovery.
- Maintain a healthy diet. To the extent that you can, try to eat regularly and healthily. Eating nutritious meals and snacks helps regulate your body chemistry and provides essential vitamins and minerals to support your recovery. Focus on fruits, vegetables, and other whole, nutrient-dense foods.
- Move your body. Exercise releases endorphins that improve your mood, reduce stress, and help you sleep. If you don’t feel up to a workout, try a gentle walk outside.
- Practice relaxation techniques: Simple techniques like deep breathing2 can effectively manage stress and anxiety, which often trigger cravings.
Building healthy habits takes time and consistency—go easy on yourself while you’re not feeling your best. Start with small, achievable goals, and congratulate yourself for your progress.
Use Education and Self-Help Resources
While waiting for rehab, educating yourself through self-help resources can empower you on your path to recovery. Here are some options to explore:
Books
- In the Realm of Hungry Ghosts by physician and addiction specialist Gabor Maté explores the traumas people experience as a result of substance use and recommends strategies for change.
- In The Addiction Manifesto, author J.R. Weaver reflects on his experience with addiction and the approaches that helped him recover.
- Why Don’t They Just Quit? by Joe Herzanek debunks common myths around addiction and explores topics like rock bottom, enabling, and intervention.
Podcasts
- A Sober Girls Guide podcast explores mental health, self-development, and wellness through interviews with notable women in recovery.
- In The Addicted Mind podcast, licensed therapist Duane Osterlind talks with both professionals and people in recovery who offer guidance and encouragement.
- The Recovery Happy Hour podcast hosts people who share their stories of recovery for those who are curious about getting sober from alcohol.
Helplines
- SAMHSA’s National Helpline is a free, confidential, 24/7 hotline that can refer you to addiction recovery resources.
Note that not all helplines are reputable. Some are owned by treatment centers and designed to refer clients to their businesses. Learn more about this in our article on recovery hotlines.
Communicating With Rehab Facilities
Maintain Contact While You Explore Your Options
While you look for rehab waitlist alternatives, stay connected with your preferred rehab center.
- Schedule regular follow-up calls. Schedule regular check-ins to inquire about updates on the waitlist and potential openings due to cancellations or last-minute changes.
- Express your willingness to consider alternatives. Express your eagerness to begin treatment and ask about different programs they offer.
- Explore their additional resources. Many rehabs offer resources and support groups that are open to the public. Participating in these offerings allows you to be involved with the facility, get a glimpse into the treatment experience, and learn about additional resources.
Taking initiative and committing to recovery by communicating proactively can increase your chances of being admitted sooner.
Expand Your Search
While staying in touch with your preferred rehab center is helpful, don’t limit yourself. Broadening your search can increase your chances of finding immediate support.
Consider a wider geographical area. While staying close to home can be ideal, facilities in other cities or states (or even countries) may have immediate availability.
Use online search tools. Use our treatment finder tool to find rehab facilities across the US and abroad. You can filter based on location, insurance coverage, and specific treatment approaches to find a program that aligns with your needs and doesn’t have a waitlist.
Research different programs. Some rehabs have specialized programs, such as gender-specific, faith-based, or programs for specific addictions. You might find a good match with open availability while still effectively addressing your recovery needs.
Expanding your search doesn’t mean compromising your recovery goals. Being flexible and exploring various options increases your chances of securing immediate placement.
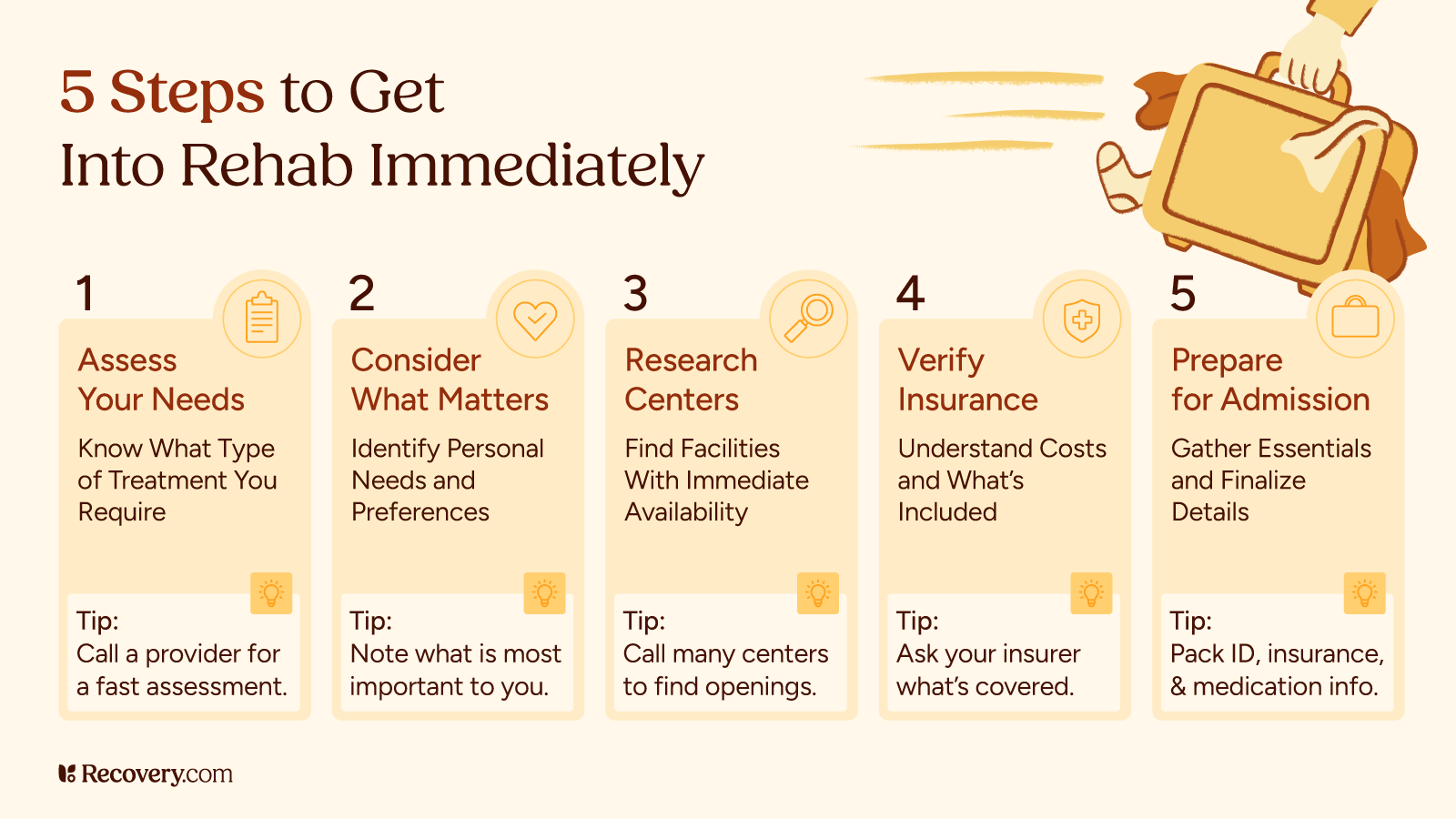
Planning for Admission
Being prepared to start rehab once you get news of an opening can set you up for a smooth transition. Here are some steps you can take:
- Take care of your personal obligations
- Inform your employer
- Manage your financial responsibilities
- Pack for your stay
See more on this, and get a downloadable checklist, in our article on preparing for rehab.
Preparing in advance, both mentally and practically, will help you make the most of this life-changing opportunity.
Keep Calm and Maintain Your Progress
Encountering a waitlist for rehab can be discouraging, but it doesn’t have to derail your recovery journey. Use these strategies to navigate this hurdle, and remember that it’s only temporary.
While securing immediate admission is ideal, you can still take action while you wait.
Look for addiction treatment centers that meet your criteria and contact them directly to inquire about their availability.
Frequently Asked Questions About Being Waitlisted for Rehab
Is it possible to receive immediate support while on a rehab waitlist?
Yes, it’s crucial to seek immediate help while on a rehab waitlist. Options include professional assessments, crisis hotlines, harm reduction strategies, self-care practices, and connecting with people you trust for support.
What alternatives exist for those unable to get into rehab immediately?
If you’re waitlisted for a rehab, you can explore alternatives like outpatient programs, online therapy, virtual support groups, and community resources. These options offer vital support for managing addiction while waiting for inpatient treatment.
How can I increase my chances of getting admitted to rehab sooner?
To increase your chances of earlier admission to rehab, stay in contact with your preferred treatment center, express your readiness to consider alternative programs, expand your search to include broader geographical areas, and be prepared for admission by managing your personal affairs in advance.