Recognizing the signs of excessive alcohol consumption is crucial because it can significantly impact your health, relationships, and overall well-being. This article will explore ways to identify how your drinking habits affect your life. Then, discover how early intervention and support can help you address alcohol-related issues and lead to a healthier and more fulfilling life.
Understanding Excessive Alcohol Consumption
Exceeding the recommended level of alcohol consumption, commonly referred to as binge drinking, can be dangerous and potentially lead to hazardous health effects. The amount of alcohol that is considered to be excessive drinking can vary from person to person, based on factors such as gender, age, and overall health.
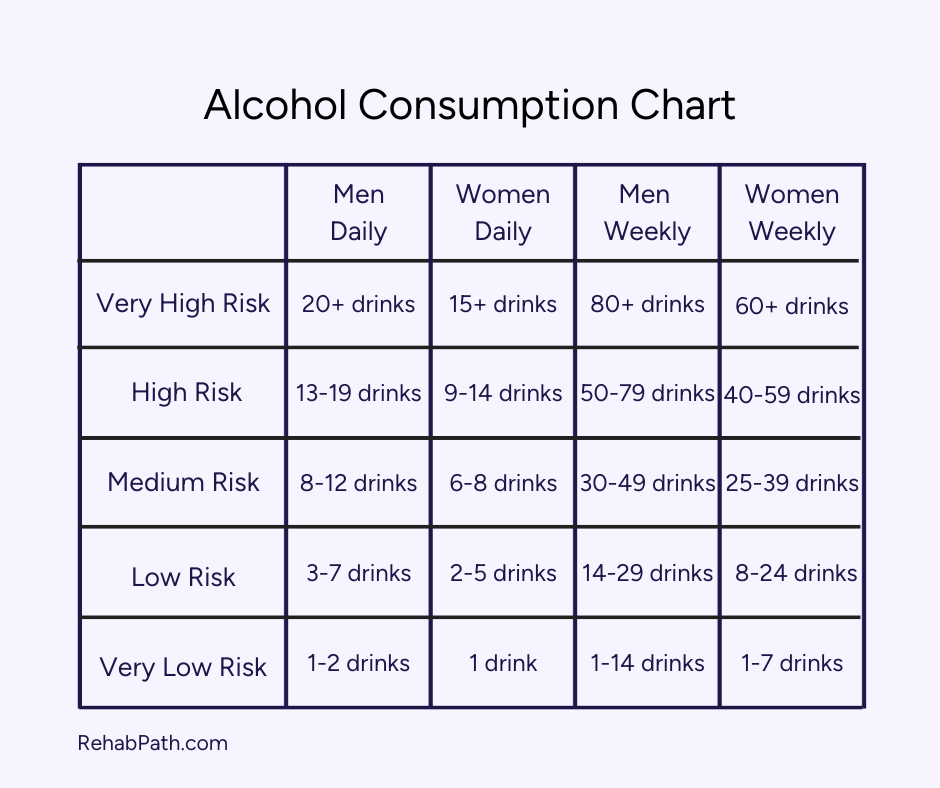
To help you understand where your alcohol consumption falls, drinking can be split into these categories:
- Moderate Drinking: This typically refers to up to one drink per day for women and up to two drinks per day for men1.
- Binge Drinking: Binge drinking is characterized by consuming a large amount of alcohol in a short period, leading to a blood alcohol concentration (BAC) level of 0.08% or higher. For men, binge drinking usually occurs after consuming five or more drinks within two hours, while for women, it is after four or more drinks in the same timeframe.
- Heavy Drinking: Heavy drinking is often defined as consuming more than the moderate drinking guidelines.
Physical Signs of Drinking Too Much
Your body will likely indicate if you’re drinking too much alcohol. You may have:
- A higher tolerance
- Due to consistent alcohol consumption over a long period of time, you might need to drink more to feel the same effects you used to.
- Frequent hangovers
- Dehydration
- Health problems
- Alcohol can damage your whole body. You might develop liver disease, a weakened immune system, and cardiovascular problems.
Consistently drinking heavy amounts of alcohol can take a toll on your body. There isn’t an amount of alcohol that doctors can deem “safe,” so you could be slowly hurting your mind and body.
Physical Health Consequences
Heavy drinking could cause liver damage, cirrhosis, and other alcohol-related diseases. You also have an increased risk of cardiovascular problems and compromised immune function, making you more likely to have worse illness symptoms.
Alcohol causes poor sleep quality2 by disrupting your rapid eye movement (REM) cycle. This impacts your mood because getting proper rest is necessary for energy and productivity.
Dehydration from drinking also negatively affects your mood3 because hydration is a crucial component of energy and mood. Without proper hydration, you may have heightened fatigue and anxiety. While alcohol may temporarily relax, its long-term effects on sleep, energy levels, and overall health outweigh the relief.
Drinking’s Impact on Mental Health
Studies found a significant link between excessive alcohol consumption and co-occurring mental health disorders4. The relationship between alcohol and mental health is complex and bidirectional, meaning alcohol abuse can contribute to the development of mental health disorders, and pre-existing mental health issues can lead to the use of alcohol as a form of self-medication.
While alcohol causes an initial feeling of euphoria or relaxation5, it is a depressant, meaning it can ultimately lead to adverse changes in mood. Alcohol is a central nervous system depressant6 that can lead to chemical imbalances in your brain, contributing to anxiety, depression, and mood swings. And cortisol, the stress hormone, releases after drinking7, making you even more anxious.
Even with all of these negative effects, you may continue your drinking habits because it can act as self-medication. Alcohol temporarily diminishes some depression and anxiety symptoms; however, using alcohol as your coping mechanism for uncomfortable feelings will cause harm in the long run.
Behavioral Indicators of Heavy Drinking
On a surface level, it might be easier to spot physical signs of heavy drinking; however, alcohol’s impact runs deeper. It can affect your whole personality and daily behaviors. You might be more secretive about how much you drink. You could also neglect your responsibilities, like being too hungover to work. And you may be more irritable with friends and family.
The behavioral and psychological signs have an interdependent connection. The mental changes from alcohol can start the onset of negative habits. And over time, your behavioral changes can spur psychological repercussions. Soon, it’ll be hard to distinguish between cause and effect.
Social Implications of Excessive Drinking
Relationships
Alcohol affects you and your relationships. Excessive drinking can lead to conflicts, arguments, and breakdowns in relationships with family members, friends, and significant others. You might even start isolating yourself from your loved ones because they want you to cut back on drinking, causing further conflict.
Professional Life
Spending more time drinking may make you less efficient at work. Your thoughts might be consumed by when you’ll get your next drink, interfering with healthy daily habits. And your hangovers could make it hard to be productive.
Risk-Taking Behaviors
The consumption of alcohol impairs the decision-making abilities of the frontal lobe in the brain8, resulting in risky behaviors such as drunk driving, having unprotected sex, and sustaining injuries. These not only put oneself at risk, but also those around them. For instance, one may face a DUI charge and other potential criminal convictions.
Signs of Alcohol Dependency and Addiction
If this article resonates with you, see if your behaviors align with alcohol dependency. Some signs of addiction include:
- Alcohol cravings
- Being unable to stop drinking until you’re drunk
- Developing a high tolerance
- Experiencing physical and psychological withdrawal symptoms when attempting to cut down or stop drinking
- Withdrawing from friends and family, becoming secretive about drinking habits
- Using alcohol to cope with stress, anxiety, depression, or other emotional problems
- Continued drinking despite negative consequences
Assessing Your Alcohol Consumption
Assessing your alcohol consumption is essential in understanding whether your drinking habits are within safe and healthy limits.
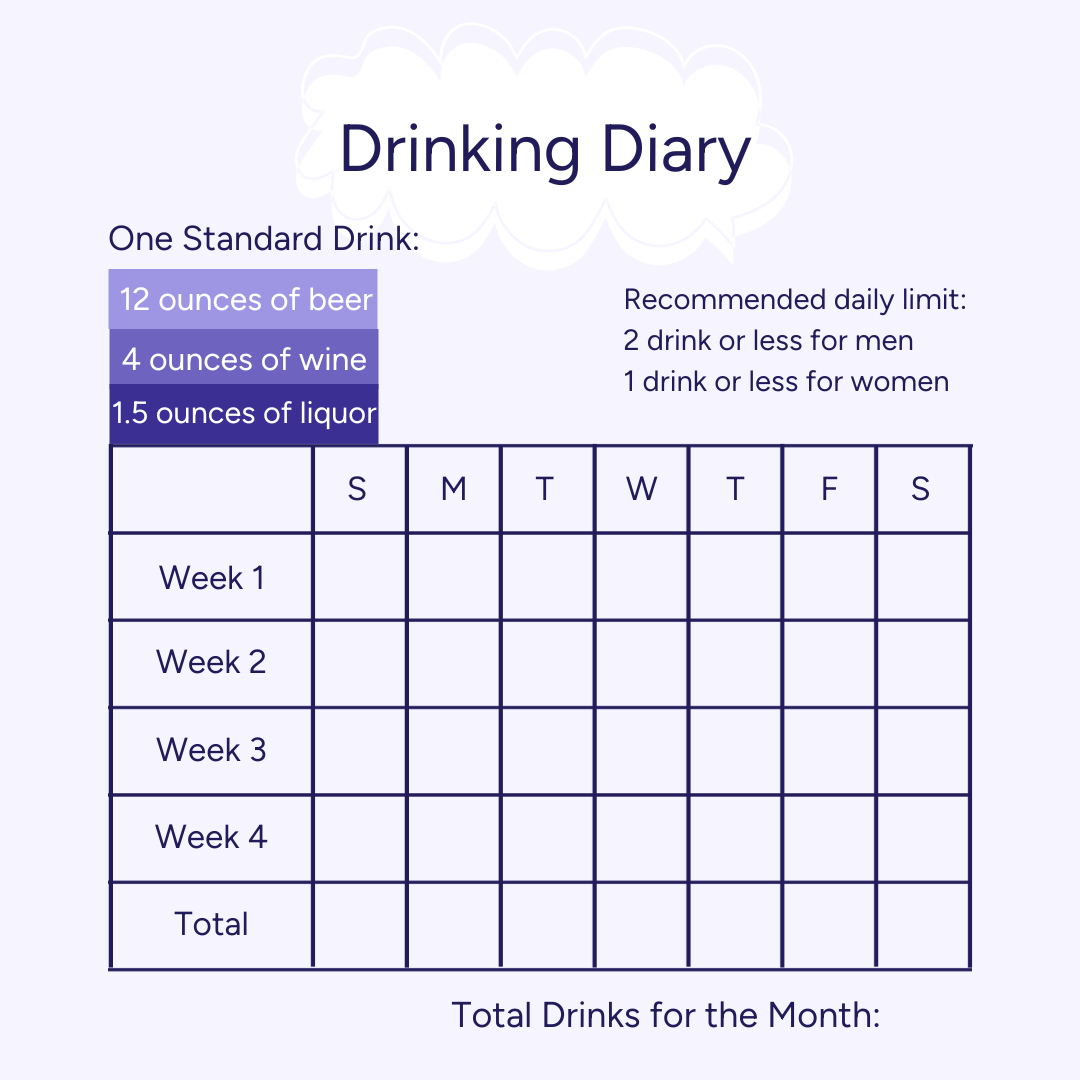
You can start a drinking diary to record all the alcoholic beverages you consume for at least 1 month. Write about the type of drink and the volume (in milliliters or ounces) of each beverage. This can serve as a visual representation of your alcohol consumption, so you can easily evaluate if it’s at a healthy limit.
You can compare your drinks to standard drink sizes to better gauge how much you’re drinking. A standard drink size in the United States is 12 ounces for a beer, 5 ounces for wine, and 1.5 ounces for distilled spirits. For example, if you drank on Friday and had 3 beers and 1 glass of wine, you’d write down 4 drinks.
Talking to a Provider About Heavy Drinking
For reliable advice and support regarding alcohol-related matters, it’s best to consult with a healthcare professional. They are able to offer valuable insights, precise evaluations, and the necessary aid to address any difficulties in an effective manner.
To begin addressing your drinking habits, start by speaking to your primary care physician. Be honest and open with them, and tell them about your concerns. Describe the amount of alcohol you consume in a week, what type of drinks you have, and the activities you typically do while drinking. Additionally, explain how your drinking has affected your relationships with family and friends. Furthermore, you could ask them to refer you to a specialist if needed, who can offer further help and advice.
Once your doctor has a good understanding of your situation, they can guide you towards the right treatment. Develop a strategy to cut down or stop your excessive drinking. This could include setting specific goals, finding alternative activities to replace drinking, and identifying triggers that lead to excessive drinking.
Steps Towards Change and Seeking Help
Acknowledging the need for change and setting treatment goals are crucial steps to progress toward a healthy lifestyle. It takes courage and determination to confront your issue and make these positive changes. You and your trusted circle of friends and family can explore treatment options to determine the best fit for your individual needs.
Detox
Many people begin their journey by going through the detox process, so you can safely rid your body of alcohol. You’ll have medical professionals there to ensure you’re as comfortable as possible. This can help you feel more focused and prepared to take on therapy.
Residential Programs
Residential rehab may benefit you if you need a more intensive, distraction-free environment to focus on therapies and working through your alcohol dependency. You’ll get to the root cause of your drinking habits and develop new strategies to cope with uncomfortable feelings and situations.
You might participate in evidence-based therapies like cognitive behavioral therapy (CBT). Your loved ones can engage in family therapy, so you can find common ground and work towards healthier relationships.
PHP/IOP
Your care team may recommend an outpatient program if your drinking habits need less intensive care. Outpatient treatment has varying levels of care, with partial hospitalization (PHP) providing a more intensive level of care and outpatient (OP) providing the least intensive. You’ll participate in the program for a few hours a day on certain days of the week, allowing you to go to work or attend school simultaneously. You’ll learn new coping mechanisms to manage your triggers. And your support network will grow as you heal with others in therapy.
Support Groups
Joining support groups like Alcoholics Anonymous and SMART Recovery9 provides a sense of community, understanding, and accountability in your recovery. They offer a safe space to share experiences, learn from others, and receive ongoing support.
Freeing Yourself from Alcohol
If you feel like you can’t drink at a healthy pace and use alcohol to cope with uncomfortable feelings, it might be time to seek treatment. You can discover, and sustain, a healthy and balanced lifestyle that prioritizes your well-being. Embrace a life without alcohol. Begin your search by browsing our list of treatment centers for alcohol addiction.
