Have you noticed that your pain medication isn’t working as well as it used to? Or wondered why you need higher doses of anxiety medication after using other substances? This might be due to cross-tolerance, a fascinating but often misunderstood process that affects people taking multiple medications or using substances alongside their medications.
Cross-tolerance happens when building tolerance to one substance affects how your body responds to another, seemingly different substance. This isn’t just a curiosity; it has real impacts on medication effectiveness, overdose risk, addiction recovery, and your everyday health management.
Let’s explore how cross-tolerance develops, look at some real-world examples, and discuss practical strategies for managing its effects on your treatment and your health.
What Is Cross-Tolerance?
Cross-tolerance is when your body’s adaptation to one substance lessens your response to another substance that works in similar ways. If your brain gets used to one type of substance, it might also become less responsive to other substances that affect similar receptors.
The American Psychological Association defines cross-tolerance2 as:
A condition in which tolerance to one drug results in a lessened response (i.e., increased tolerance) to a related drug.
This happens because many substances share common pathways in your brain and body. In pharmacology, this is understood as a shared mechanism of action, meaning the substances influence the same biological targets in the body.
When you use a substance repeatedly, your brain adapts to maintain balance. It might produce fewer natural chemicals, become less sensitive to the substance’s effects, or create more enzymes to break down the substance faster. These adaptations don’t just affect the original substance—they can also impact other substances that work through the same biological systems.
Different Substances, Similar Neural Pathways
Cross-tolerance is most common between substances that affect the same brain receptors2 or neurotransmitter systems. For example, if you develop tolerance to prescription opioid painkillers, you might also have reduced sensitivity to other opioids, including illegal ones like heroin. This happens because all opioids work on the same receptor system in your brain.
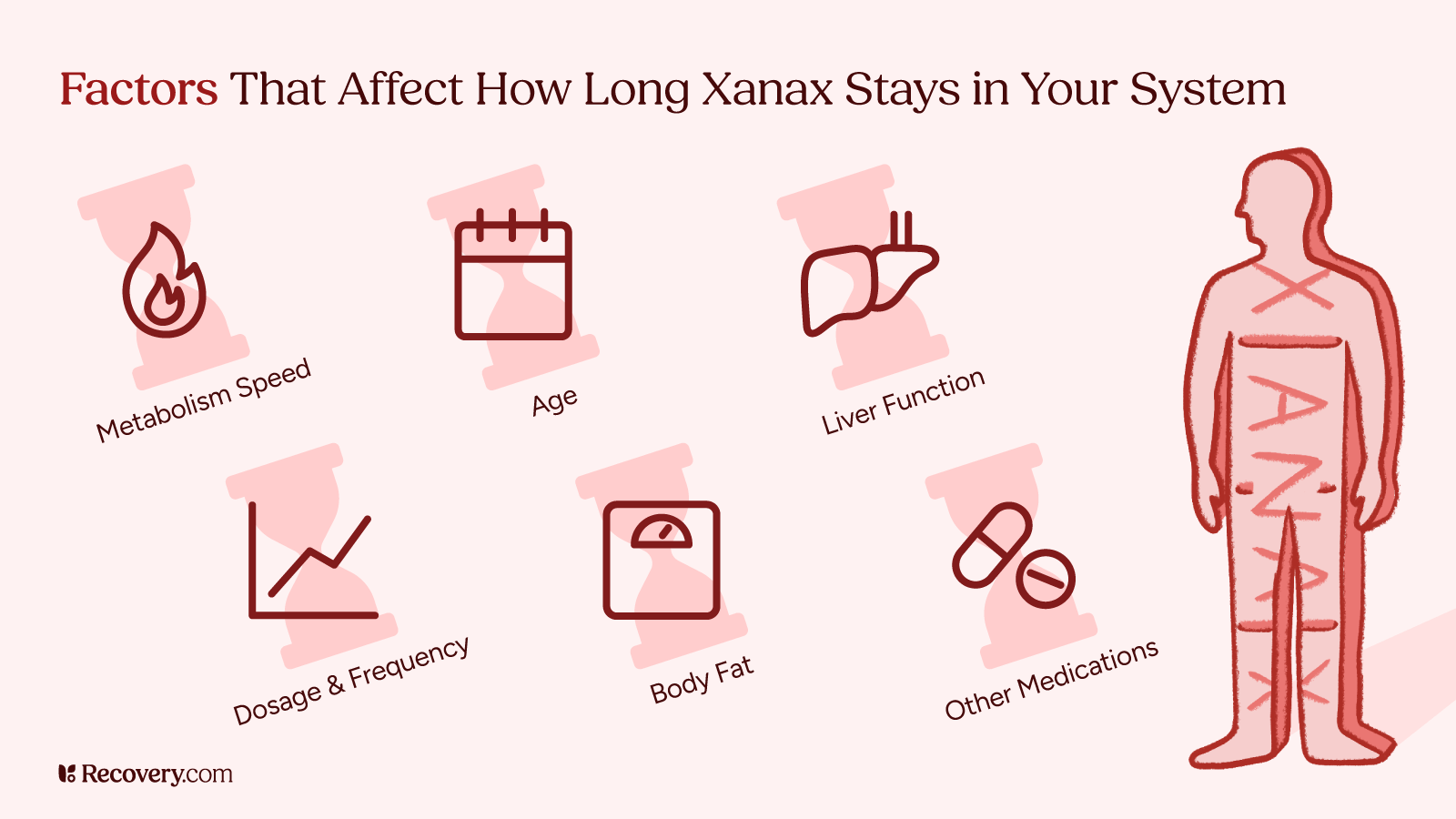
The process isn’t always predictable or complete. You might have strong cross-tolerance between some substances but not others. Your degree of cross-tolerance depends on factors like how similar the substances are, how much you’ve used, how long you’ve been using, and your individual biology.
Cross-tolerance can happen between a lot of different types of substances. The APA notes that cross-tolerance is commonly seen with “amphetamines,1 benzodiazepines, hallucinogens, and opiates, among other drugs.” It can also occur between alcohol and various medications, different types of antidepressants, and even between prescriptions and street drugs.
Why This Matters to You
Understanding cross-tolerance is important for both medical treatment and harm reduction. It affects how doctors prescribe medications, how effective treatments might be, and what risks you face when combining different substances. It’s also a major factor in addiction treatment and recovery planning.
Common Examples of Cross-Tolerance
Cross-tolerance can show up in a lot of different situations, from prescription medications to recreational substances. Here are some of the most important patterns to understand.
Cross-Tolerance Between Opioids
Because they work on the same opioid receptors, all opioids can cause cross-tolerance3 (most commonly, incomplete cross-tolerance) with each other. That means if you’ve been taking prescription painkillers like oxycodone or morphine for a while, your body might also be less sensitive to other opioids, including illegal ones like heroin or fentanyl.
This causes serious risks. Someone who has built tolerance to prescription opioids might think they need a large amount of street opioids to feel effects. But because street drugs are often much stronger and less predictable than prescription medications, this miscalculation can lead to overdose.
For people in medical treatment, opioid cross-tolerance can complicate pain management. If you’ve developed tolerance to one type of pain medication, your doctor might need to try different approaches or higher doses to help manage your pain effectively.
If you or someone you know uses opioids, see our article on How to Use Naloxone to learn about this life-saving overdose reversal medication.
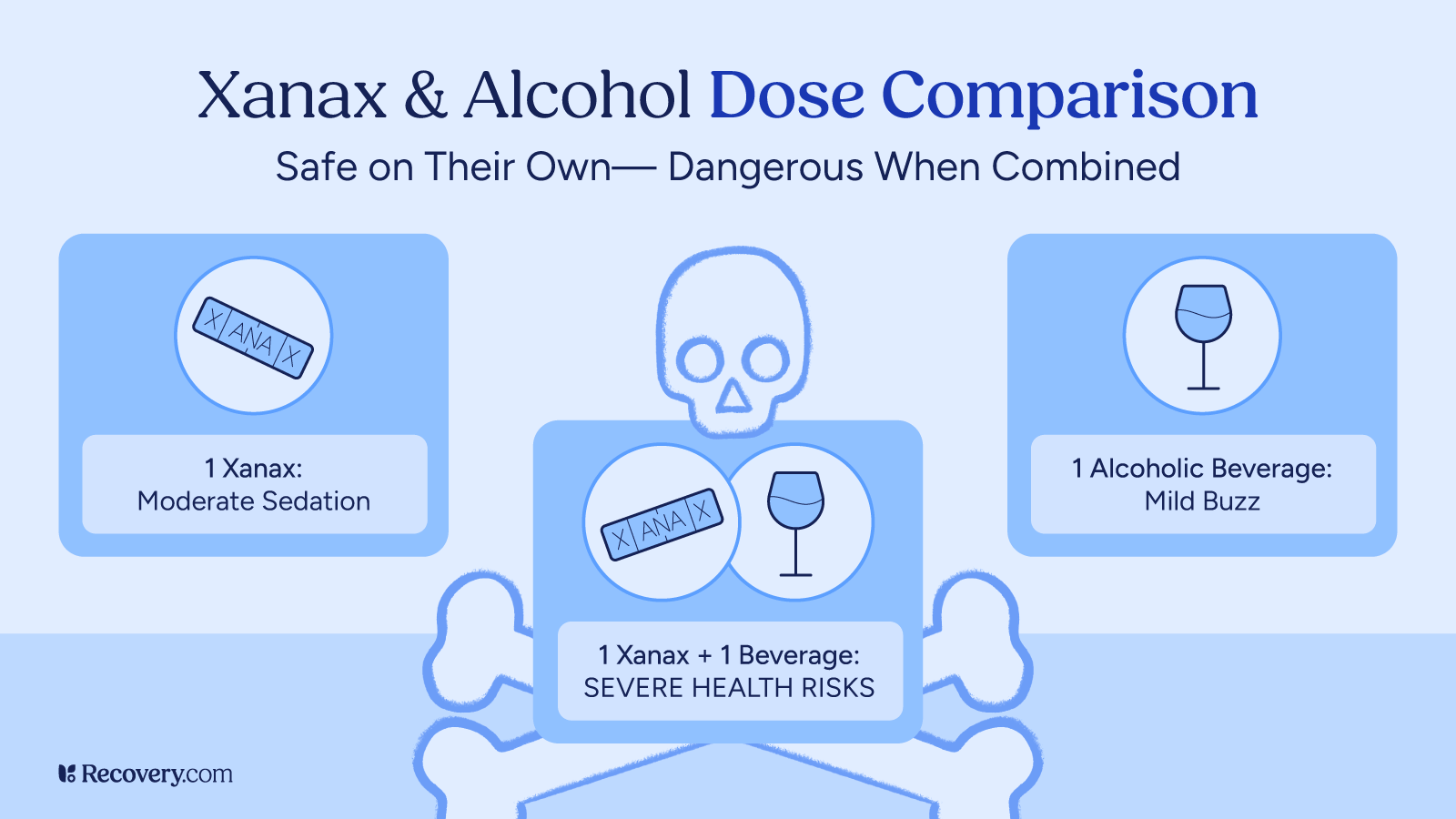
Alcohol and Benzodiazepines
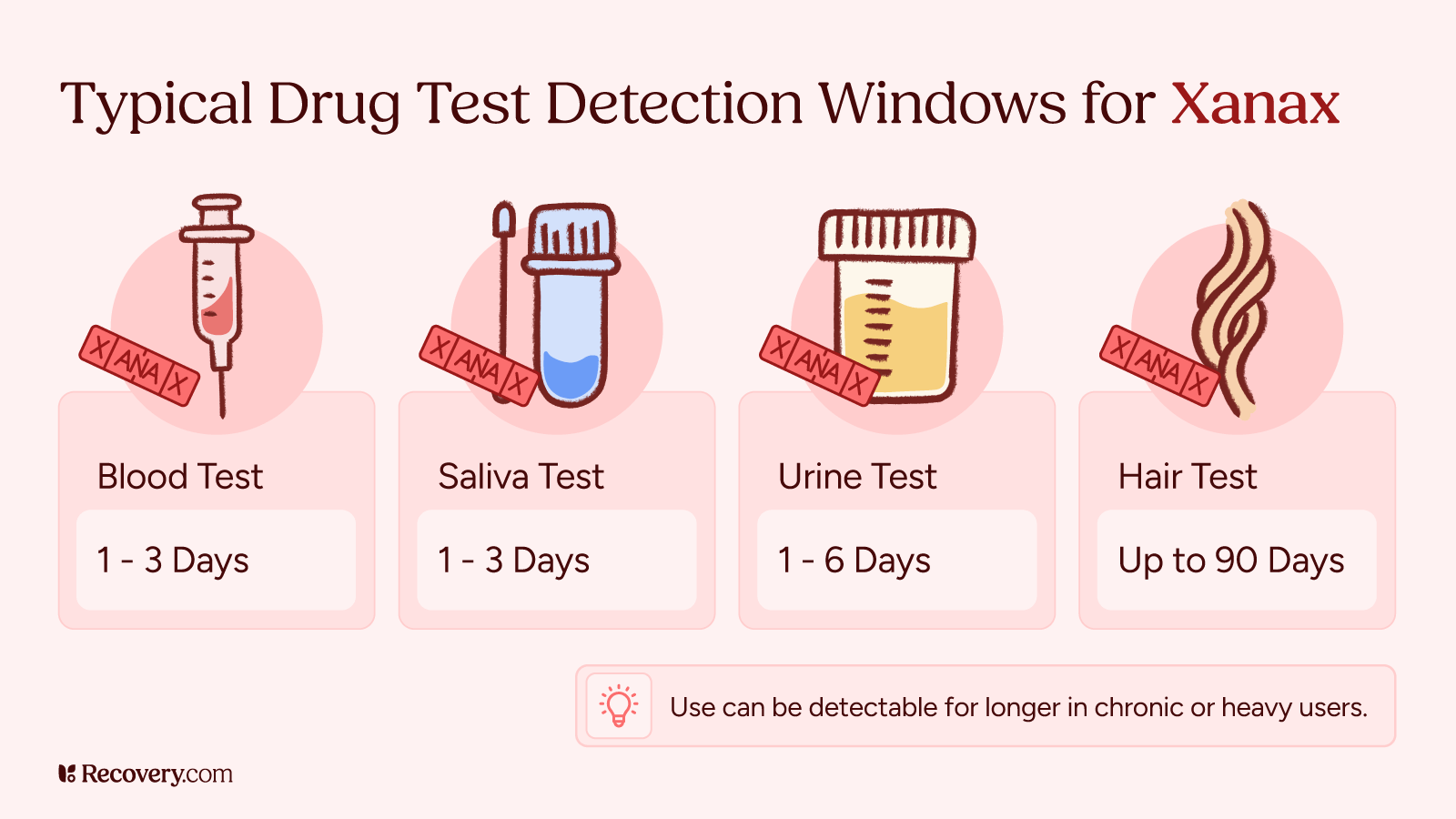
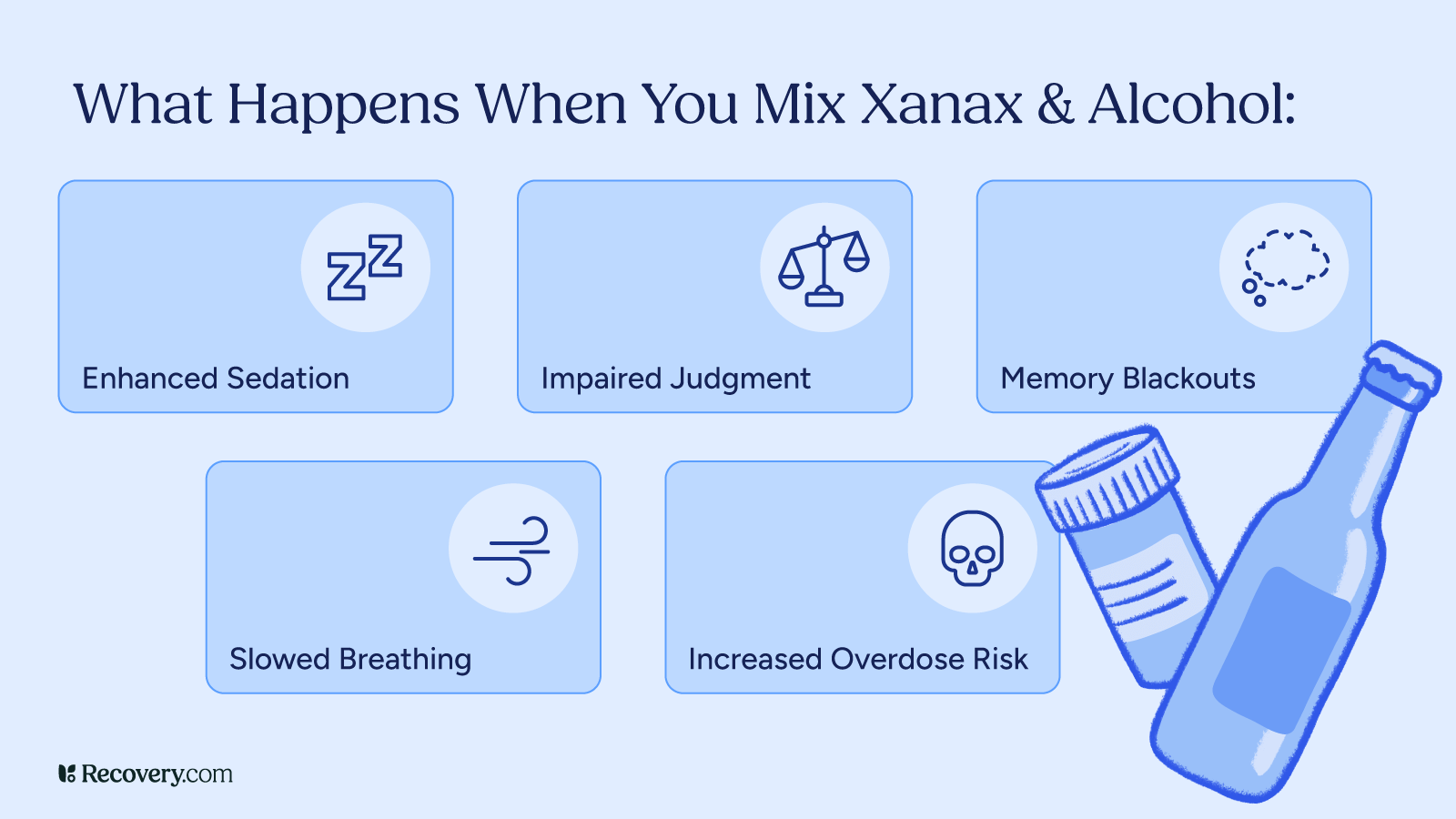
Alcohol and benzodiazepines (like Xanax, Valium, or Ativan) are both agonists that work on the same brain system called GABA.4 That means people who drink regularly often need higher doses of these medications to feel the same effects.
This type of cross-tolerance is especially dangerous because both alcohol and benzos slow down your breathing and heart rate. When people have cross-tolerance, they might use more of both substances, which can lead to life-threatening overdose.
Barbiturates, an older drug class of sedatives sometimes used for seizure control or anesthesia, also act on the GABA system. People with alcohol or benzodiazepine tolerance may also be less sensitive to barbiturates, which makes dosing less predictable and increases overdose risk.
Doctors need to know about your drinking habits when they’re prescribing benzodiazepines. If you have alcohol tolerance, you might need different medications or special monitoring to stay safe.
Learn more about how to keep yourself safe in our article on the risks of mixing benzos and alcohol.
Other Important Cross-Tolerance Patterns
Prescription stimulants can cause cross-tolerance with cocaine,5 meth, and other stimulants. This includes ADHD medications like Adderall and Ritalin, and it can affect both the effectiveness of ADHD treatment and the risks of using other stimulants.
Cannabis can also show partial cross-tolerance with other substances6 that affect similar brain receptors, such as certain sedatives. Regular cannabis use may also influence how your body responds to medications that impact mood, sleep, or appetite.
Psychedelic drugs also show cross-tolerance patterns.7 If you use LSD, you might find that mushrooms (psilocybin) or mescaline don’t work as well for several days afterward. These substances all affect similar brain pathways.
Different types of sedatives and sleep medications often have cross-tolerance too. This includes prescription sleep aids, muscle relaxers, and some seizure medications. If you take one regularly, others in the same category might be less effective.
How Cross-Tolerance Develops in Your Body
Your brain is constantly working to keep things balanced. When you use a substance regularly, your brain notices and starts making changes to cope. You can think of it as a thermostat that’s trying to keep the temperature just right. When a substance comes in and turns up the heat, your brain responds by turning down its own systems to balance things out.
Your brain has special spots called receptors that substances attach to. When you use a substance often, your brain might make fewer of these receptors or make them less sensitive. Your brain also makes its own natural “feel-good” chemicals like dopamine and serotonin. But when you use substances regularly, it starts making less of these natural chemicals.
Cross-tolerance usually develops gradually over weeks or months of regular use, but some people develop it faster than others based on their genetics, age, and overall health. The changes that cause cross-tolerance can last for weeks or even months after you stop using a substance.
Cross-Tolerance and Substance Use
If you use drugs recreationally, cross-tolerance can significantly impact both their effects and the risks involved.
Impact on Drug Effectiveness
Cross-tolerance often means you won’t get the effects you’re expecting from substances. If you’ve built tolerance to one drug, you might find it much harder to achieve the same desired effect with a different drug that has similar effects on your brain.
This can be frustrating and dangerous. You might end up using more of a substance than you planned to, thinking it’s not working. But the problem isn’t with the substance—it’s that your brain has adapted to other substances that work on the same pathways.
Overdose Risks
Cross-tolerance creates a serious risk of overdose that many people don’t realize. Just because you can handle large amounts of one substance doesn’t mean you’re safe with large amounts of another—even if they seem similar.
Here’s why this is so dangerous: tolerance affects how high you feel, but it doesn’t always protect you from overdose. Your brain might be less sensitive to the euphoric effects of heroin, for example, but your respiratory system can still shut down from too much of it.
Street drugs are especially risky because you never know exactly what you’re getting or how strong it is. Someone with opioid tolerance might take what seems like a reasonable amount of street fentanyl, not knowing it’s much more potent than their usual pills.
Fentanyl is an extremely potent synthetic opioid that’s causing overdoses even among people who aren’t aware that it’s in their drugs. Learn more about what you can do to prevent these risks in our article on fentanyl use and addiction.
Complications With Polydrug Use
Cross-tolerance often leads people to mix different substances to get the effects they want. This is called polydrug use, and it’s much more dangerous than using one substance at a time.
The unpredictability of polydrug use makes it especially risky. You might be fine mixing substances one day but have a dangerous reaction the next, depending on factors like how much you’ve eaten, how tired you are, or what other medications you’re taking.
Researchers warn about the dangers of this practice, even going so far as to call it “Russian roulette”. According to one study,
Using benzos or z-drugs and opioids together was likened to playing Russian roulette due to an unregulated drug market, unpredictable potency, availability and contents of illegal drugs and a lack of information about how these drugs work together.
When you combine substances, they can interact in unpredictable ways. Even if you have tolerance to each substance individually, combining them can overwhelm your body’s ability to cope.
For more insight into the risks and treatment options for using multiple substances, see our article on polydrug addiction.
Cross-Tolerance and Medical Treatment
Cross-tolerance can significantly impact your medical care, making treatment more complex and sometimes less effective.
Challenges in Pain Management
The development of tolerance to opioid analgesics like oxycodone or morphine can make managing pain much more difficult. Your doctor might need to prescribe higher doses, try different types of pain medications, or use a completely different approach.
This puts both you and your doctor in a tough spot. Higher doses increase the risk of side effects and addiction. But undertreated pain can seriously impact your quality of life and ability to heal.
Some doctors might be hesitant to prescribe adequate pain medication if they know you have tolerance. It’s important to be honest with your healthcare team about your substance use history so they can find safe, effective ways to manage your pain.
Effects of Psychiatric Medication
Cross-tolerance can affect medications for depression,8 anxiety, bipolar disorder, and other mental health conditions. If you have tolerance to substances that affect the same brain systems as your psychiatric medications, those medications might not work as well.
For example, if you take medication for anxiety and drink heavily, Your provider may adjust your treatment plan to ensure it works effectively and safely. If you use stimulants, your ADHD medication might be less effective. This can make treating mental health conditions much more challenging.
Your psychiatrist needs to know about any substance use to prescribe medications safely and effectively. They might need to adjust doses, try different medications, or monitor you more closely.
Learn more about the importance of regularly reviewing and updating your medication plan in our article on medication management.
Managing Chronic Diseases
Cross-tolerance can impact medications used for conditions like high blood pressure, diabetes, and heart disease. When the medication doesn’t work as expected, it can be harder to control these serious health conditions.
This is especially concerning because a lot of chronic diseases require precise medication management. If your medications aren’t working properly due to cross-tolerance, your health condition could get worse.
Surgery and Emergency Care
Cross-tolerance significantly affects surgical procedures and emergency medical care. If you have tolerance to opioids or other substances, anesthesia might not work as expected during surgery.9 You might wake up during procedures or experience inadequate pain control afterward.
Emergency situations become more complicated when cross-tolerance is involved. Emergency room doctors might struggle to provide effective pain relief or sedation if they don’t know about your tolerance. This can make traumatic situations even harder to manage.
It’s important to make sure everyone on your medical care team knows about your substance use history, even in emergencies. This information helps them provide safer, more effective care and can prevent dangerous complications during treatment.
Cancer Treatment and Chemotherapy
Cancer patients often face unique challenges with cross-tolerance. Chemo and other cancer treatments affect how your body processes medications. If you also have substance tolerance, managing pain and other symptoms becomes much more complex.
Cancer pain is often severe and requires strong medications. If you have cross-tolerance to opioids, your oncology team might need to use higher doses, different medications, or alternative pain management approaches. This requires careful coordination between all your healthcare providers.
Addressing Cross-Tolerance in Addiction Recovery
Cross-tolerance creates unique challenges during treatment for substance use disorders.
Medication-Assisted Treatment (MAT)
Medication-assisted treatment (MAT) programs use medications like methadone, buprenorphine, or naltrexone to help people recover from opioid addiction. If you have cross-tolerance, these medications might not work as expected, and your treatment team might need to adjust the approach.
Detox and Withdrawals
Cross-tolerance makes managing withdrawals more complicated. You might experience withdrawal symptoms from multiple substances, even if you were only actively using one. This can make detox longer and more uncomfortable.
Risk of Relapse
Cross-tolerance also affects relapse risk. If you’re in recovery and your usual substances don’t give you the effects you remember, you might be tempted to try stronger substances or use multiple substances together. Both of these approaches are highly dangerous.
Recovery programs need to address cross-tolerance specifically. Good-quality treatment programs will assess your complete substance use history and create a personalized plan that takes any possible effects of cross-tolerance into account.
Cross-Tolerance in Specific Patient Groups
Different groups of people face unique challenges with cross-tolerance that require special consideration and care.
People Who Are Pregnant and Breastfeeding
Cross-tolerance during pregnancy can create complex medical situations. Pregnant people might need different pain medications during labor and delivery if they have tolerance to opioids. Healthcare needs to balance effective pain relief with safety for both the birthing parent and the baby.10
Substance use during pregnancy affects babies’ developing brains, potentially making them more likely to develop tolerance issues later in life. If you’re pregnant and have substance tolerance, specialized maternal care programs11 can help manage both your health and your baby’s safety.
Those who are breastfeeding while managing cross-tolerance need to choose medication carefully. Because so many substances can pass through breast milk, healthcare providers need to select treatments that are safe for nursing babies while still effective for their caregiver.
Medication Interactions for Older Adults
Older adults often take multiple medications for different health conditions, making cross-tolerance more dangerous and more likely. Their bodies also process medications differently than younger people, which also makes the effects of tolerance less predictable.
Falls and confusion are serious risks for elderly people with cross-tolerance.12 If their medications aren’t working properly, they might be more likely to have accidents or experience dangerous side effects from taking higher doses.
Family members and caregivers should be aware of cross-tolerance risks in elderly loved ones. Regular medication reviews and honest communication with healthcare providers are especially important for this population.
Teenagers and Young Adults
Young people’s brains are still developing, which makes them more vulnerable to developing cross-tolerance quickly. What might take months to develop in adults can happen in weeks for teenagers who use substances regularly.13
ADHD medications are a common concern for this age group. Many teens and young adults take stimulant medications for ADHD, and cross-tolerance with other stimulants can affect both their treatment effectiveness and their risk if they use other substances.
College environments often involve alcohol and substance use, which can interact dangerously with prescription medications. Young adults need education about these risks to make informed decisions about their health and safety.
For more information about the risks and treatment options for stimulant medications, see our article on Adderall addiction.
Risk Factors for Developing Cross-Tolerance
Several factors make some people more likely to develop cross-tolerance14 than others:
- Individual sensitivity: Some people’s brains are naturally more or less sensitive to substances, which affects how quickly tolerance develops.
- Frequency and duration of use: Regular, long-term use increases your chances of developing cross-tolerance compared to occasional use.
- Age and developmental factors: Teenagers and young adults develop tolerance faster because their brains are still developing and more adaptable to change.
- Environmental influences: High stress, trauma, and chaotic environments can speed up tolerance development and make cross-tolerance more likely.
- Underlying health conditions: Mental health conditions, chronic pain, and some genetic factors can increase your risk of developing cross-tolerance.
- Genetic predisposition: Your family history and genetics affect how your body processes substances and how quickly you develop tolerance.
- Polydrug use patterns: Using multiple substances regularly increases your risk of developing cross-tolerance between them.
- Metabolism differences: How fast or slow your body breaks down substances affects how quickly tolerance develops.
Managing and Preventing Cross-Tolerance
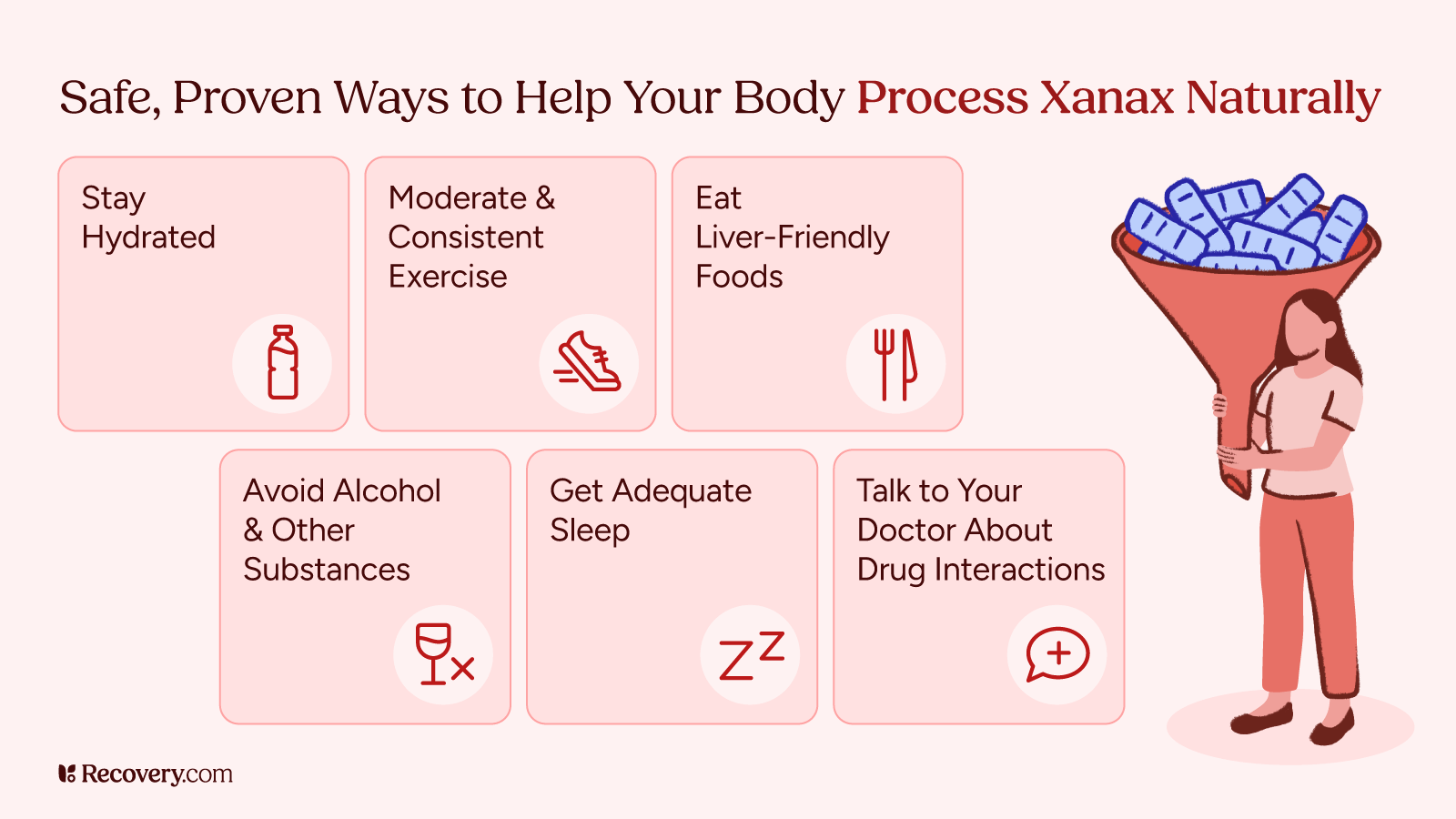
Professional Treatment Approaches
Healthcare providers use several strategies to manage cross-tolerance effectively. The first step is always a thorough assessment of your substance use history that includes prescription medications, over-the-counter drugs, alcohol, and any illegal substances.
Regular medication reviews are essential. Your doctor should check how well your medications are working and watch for signs of tolerance or cross-tolerance. They may need to adjust doses, switch medications, or try a combined approach.
What works for one person might not work for another, especially when cross-tolerance is involved. That’s why it’s so important for your care to take place according to a personalized treatment plan that takes your specific tolerance patterns into account.
Advocating for Yourself in Healthcare Settings
Being honest with your healthcare providers is important for safe, effective treatment. This includes telling them about all substance use, even if you’re worried about judgment. Healthcare providers need this information to keep you safe.
If you’re using multiple substances and not ready to quit, harm reduction strategies can help keep you safer. This includes using one substance at a time when possible, having someone with you who can get help if needed, and knowing the signs of overdose.
If your doctor isn’t already doing them, ask for regular medication reviews. If your medications don’t seem to be working as well as they used to, cross-tolerance might be the reason.
Keep a record of all medications and substances you use, including over-the-counter drugs, supplements, and any recreational substances. This information can be vital in emergency situations and helps your healthcare team make better treatment decisions.
Consider working with specialists who understand cross-tolerance, such as addiction medicine doctors or pain management specialists. These providers have extra training in managing complex tolerance situations and can often offer more effective treatment options.
Common Misconceptions About Drug Tolerance
A lot of dangerous myths surround cross-tolerance that can put people at serious risk. Understanding the truth can help you make safer decisions.
“If I have tolerance to one drug, I’m safe taking larger amounts of similar drugs.”
This is extremely dangerous thinking. Tolerance affects how high you feel, but it doesn’t protect you from overdose. Your brain might be less sensitive to euphoric effects, but your body can still shut down from too much of a substance. Many overdoses happen to people who midjudge their tolerance.15
“Cross-tolerance means all similar drugs affect me the same way.”
Cross-tolerance isn’t complete or predictable. You might have strong tolerance to one opioid but much less tolerance to another. Street drugs especially vary in strength and purity, making this assumption potentially fatal.
“If my medication isn’t working, I just need a higher dose.”
While dose adjustment might be necessary, jumping to higher doses without medical supervision is dangerous.16 Your reduced response might be due to cross-tolerance, but it could also be due to other factors that require different solutions.
“Cross-tolerance goes away quickly when I stop using substances.”
Brain changes from cross-tolerance can last weeks or months after stopping substance use. Don’t assume your medication sensitivity has returned to normal right away. This is why medical supervision is important during recovery.
“Prescription drugs don’t cause cross-tolerance with illegal drugs.”
Many prescription medications can cause cross-tolerance with illegal substances. Prescription opioids and street opioids, for example, affect the same brain systems. Benzodiazepines prescribed for anxiety can cause cross-tolerance with alcohol. Just because a drug is legal doesn’t mean it can’t have dangerous effects.
“I can prevent cross-tolerance by switching between different drugs.”
Rotating between substances that affect the same brain systems won’t prevent cross-tolerance. In fact, it might make it worse by exposing your brain to multiple substances17 that cause similar adaptations.
Current Research and Future Directions
Research on cross-tolerance continues to reveal important findings that could improve treatment approaches.
Recent studies on heroin addiction recovery show that cross-tolerance to buprenorphine18 (a medication used in addiction treatment) is linked to faster relapse rates. This research is helping doctors understand how to adjust treatment plans for better success.
Emerging research on anesthesia shows that people with substance tolerance often need different approaches during surgery.19 Anesthesiologists are developing better ways to provide safe, effective anesthesia for people with cross-tolerance.
Studies on ADHD medications reveal that using multiple stimulant medications can lead to cross-tolerance20 and reduced effectiveness over time. This research is helping doctors find better ways to manage ADHD treatment long-term.
Future neuroscience research directions include mapping exactly how different substances affect brain pathways, identifying genetic markers that predict cross-tolerance risk, and developing new medications that are less likely to cause cross-tolerance.
Understanding Cross-Tolerance Is the First Step Toward Safer, More Effective Care
Cross-tolerance is a complex but important concept that affects millions of people taking medications or using substances. Understanding how it works can help you make safer decisions and get better medical care.
The key takeaway is that substances often affect each other in ways you might not expect. Being honest with healthcare providers about all substance use—prescription, over-the-counter, and recreational—is essential for your safety and effective treatment.
If you’re struggling with substance use and cross-tolerance is complicating your situation, professional help is available. Find a treatment center near you that understands these complex issues and can provide the specialized care you need.
FAQs
Q: How long does cross-tolerance last after stopping substance use?
A: Cross-tolerance can persist for weeks to months after stopping substance use, depending on how long you used substances, what types you used, and your individual biology. Some people notice their medication sensitivity returning to normal within a few weeks, while others may take several months.
Q: Can cross-tolerance be reversed?
A: Yes, cross-tolerance often decreases over time when you stop using the substances that caused it. However, the process is gradual and varies a lot from person to person. Working with healthcare providers during this time is important for safe medication management.
Q: How do doctors calculate medication doses when cross-tolerance is present?
A: Doctors consider your substance use history, current tolerance levels, and individual response to medications. They often start with standard doses and adjust based on your response, monitoring you closely for both effectiveness and side effects.
Q: Does cross-tolerance affect all medications the same way?
A: No, cross-tolerance only affects medications that work on similar brain pathways as the substances you’ve used. For example, opioid tolerance won’t affect your blood pressure medication, but it might affect other pain medications.
Q: Can you prevent cross-tolerance from developing?
A: The most reliable way to prevent cross-tolerance is to avoid using substances that affect the same brain systems. If you need to take medications long-term, work closely with your doctor to monitor for tolerance and adjust treatment as needed.
Q: Is cross-tolerance the same as drug interactions?
A: No, these are different concepts. Drug interactions happen when substances affect each other directly in your body. Cross-tolerance is when your brain’s adaptation to one substance affects your response to another.
Q: How quickly does cross-tolerance develop?
A: Cross-tolerance can develop anywhere from days to months, depending on the substances involved, how often you use them, and individual factors like genetics and age. Some people notice changes within just a few weeks of regular use.
Q: Can cross-tolerance affect emergency medical treatment?
A: Yes, cross-tolerance can affect emergency treatments, especially pain medications and anesthesia. This is why it’s important to be honest with emergency medical staff about your substance abuse history, even in crisis situations.