Battling depression can feel like being stuck in a deep pit with no way out. The weight of sadness, lack of energy, and loss of interest in life can be overwhelming, making even simple daily tasks feel impossible. But what if there were not just one, but many paths to finding your way back to feeling good?
In a recent episode of the Giving Voice to Mental Health Podcast by Recovery.com, Sabra, a woman navigating career transitions and significant grief, shared her powerful journey through depression and recovery. Her story highlights a crucial message: options are beautiful, and not having options can be dangerous.
Sabra’s experience underscores the multifaceted nature of depression and the importance of a personalized approach to healing. From navigating seasonal affective disorder and deep depressive episodes to exploring different medications and ultimately finding profound relief through ketamine treatment, her story is a testament to resilience and the evolving landscape of mental health care.
1. Recognizing the Nuances of Depression
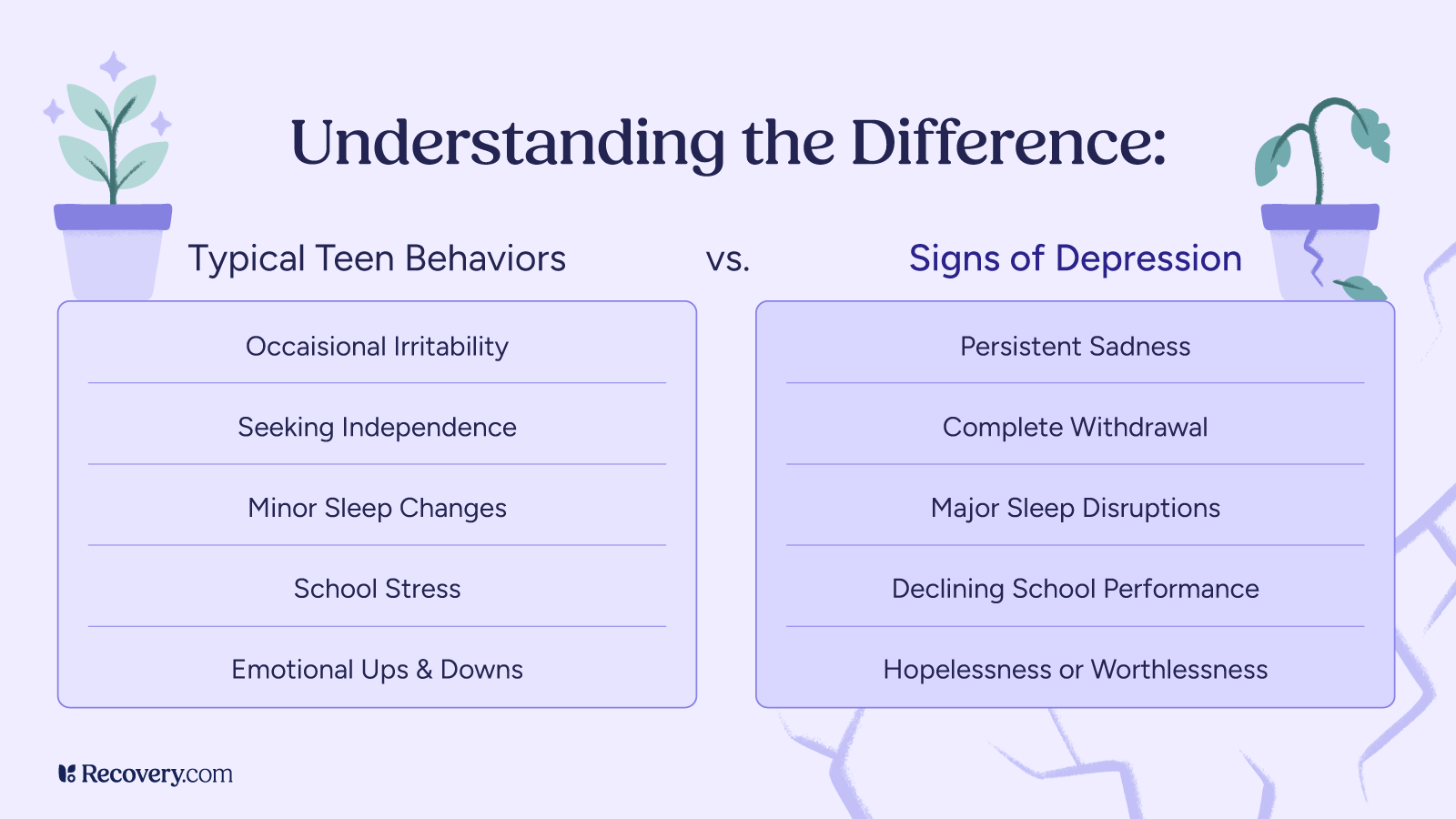
Depression isn’t a one-size-fits-all experience. It can manifest in various forms, from persistent low-grade sadness to severe, debilitating episodes. Sabra’s narrative beautifully illustrates this spectrum. She openly discussed her diagnosis of seasonal affective disorder (SAD), a type of depression linked to changes in seasons, typically in winter. However, she also spoke of “deep depressions” triggered by significant life events, such as a traumatic divorce, a devastating breakup, and the compounding grief of losing her father and beloved dog.
For Sabra, a self-proclaimed “type A person, artist who has hustled and worked and been doing all of the things all of the time,” depression brought her to a jarring halt. She describes it as slowing her down, making her feel like “nothing is functioning.” Even when she appeared “normal” to others, internally, she felt a profound loss of energy, passion, and drive.
“It may look normal, but it’s not your normal,” she powerfully stated, emphasizing the internal struggle that often goes unseen. This highlights a critical aspect of depression: its impact is often deeply personal and may not always be evident to those around you. Recognizing this internal disparity is a vital first step toward seeking help.
2. Acknowledging and Navigating Triggers
Life throws curveballs, and for individuals prone to depression, these curveballs can act as powerful triggers. Sabra’s story is a prime example. The end of a challenging marriage, a subsequent heartbreak, and then the successive losses of her father and dog plunged her into deep depressive states. These external factors exacerbated her underlying tendencies toward depression and SAD.
“I knew that there were other factors involved, like having tried a few different medications within the year and that they didn’t work. And just being triggered more and saying, yeah, this is more than just grief. This is uncontrollable grief, this is depression,” Sabra recounted.
Recognizing triggers is an essential part of managing mental health. Whether it’s seasonal changes, significant life stressors, relationship difficulties, or grief, understanding what might precipitate a depressive episode allows for proactive strategies and seeking support before symptoms become overwhelming. It’s about understanding that while grief is a natural response to loss, when it becomes “uncontrollable” and leads to a significant decline in functioning, it may have transitioned into depression.
3. The Journey Through Different Treatment Paths
The path to recovery is rarely linear, and Sabra’s experience with various treatments perfectly illustrates this. Her initial attempts with traditional antidepressants, Zoloft and Lexapro, yielded mixed results. While they offered some support, the side effects and lack of significant improvement led her to discontinue them. This highlights a common reality: finding the right medication and dosage often requires patience and collaboration with a healthcare provider.
Sabra’s candidness about the challenges she faced with these medications—sleep disturbances, headaches, and a general feeling of not receiving enough support—is a crucial reminder that not every treatment works for everyone, and it’s okay to advocate for yourself and explore alternatives.
“I did not respond well to the Zoloft. I didn’t sleep well. I had headaches all the time. It was making me very unhappy and uncomfortable. And so that was not the right thing,” she explained.
Explore treatment options for depression.
4. Embracing Novel and Emerging Treatments: Ketamine
When traditional approaches weren’t providing the relief she desperately needed, Sabra was introduced to ketamine treatment through a friend who is an ER doctor and co-owns a ketamine clinic. This marked a significant turning point in her recovery journey. Despite her initial fear and unfamiliarity with psychedelic drugs, the structured, clinical setting and the presence of a supportive nurse helped alleviate her anxieties.
Ketamine-assisted therapy is an emerging treatment for severe depression, PTSD, and other mental health conditions, often used when other treatments haven’t been effective. Administered in a controlled environment, it can rapidly reduce depressive symptoms and offer a new perspective for individuals struggling with persistent mental health challenges.
“She said, it’s okay to cry. There’s nothing wrong with that. Just experience what you can and I’ll be right here with you the whole time,” Sabra shared about her nurse, highlighting the compassionate support that made a difference.
After six sessions of ketamine treatment, Sabra experienced a profound shift. Less than a month later, she was “smiling and laughing and telling the story and out and about and feeling great.” While she still grieves her dog, the debilitating depression that consumed her had lifted.
This transformative experience underscores the importance of staying open to evidence-based, newer interventions when conventional methods fall short. It’s a reminder that the landscape of mental health treatment is continually evolving, offering new avenues for healing and recovery.
5. The Power of Community and Support
Beyond formal treatments, Sabra emphasized the critical role of community and support in her recovery. Her best friend, who advocated for ketamine treatment and provided a vital connection, played a significant role in her journey. Having someone who could see her suffering and offer a concrete solution was invaluable, especially when Sabra felt too overwhelmed to seek help herself.
“My best friend is married to an ER doctor and they own a ketamine clinic here in town, and she had been telling me, I wish you hadn’t gone on those antidepressants. I really think the ketamine would help,” Sabra explained, showing the pivotal role her friend played.
This highlights a universal truth in mental health recovery: you don’t have to go through it alone. Whether it’s friends, family, support groups, or peer communities, having a network of people who understand and care can make a profound difference. As the podcast hosts discussed, mental health challenges can be incredibly isolating, and having someone simply listen without judgment can be a powerful form of healing.
“When we can just listen, that alone can be like a treatment. That alone is one of the things that helps us get through, get past or find a little bit of peace in whatever pit we happened to be stuck in at the time,” one reflected.
6. The Evolving Nature of Recovery and Self-Compassion
Recovery from depression isn’t a destination; it’s an ongoing journey. As Sabra and the hosts discussed, what works today might not be what’s needed a year from now. Our needs change, and so too should our approach to mental well-being. This calls for a flexible mindset and a willingness to continually reassess and adapt our coping mechanisms and treatment strategies.
The idea that “all of those things that maybe felt like they didn’t work, they were leading us somewhere,” is a powerful perspective. Each attempted treatment, even if seemingly unsuccessful, provides valuable information and nudges us closer to what does work. It’s about building a comprehensive toolkit of strategies and resources rather than relying on a single “fix.”
Furthermore, self-compassion is key. Depression often comes with intense self-criticism and feelings of inadequacy. Sabra, as a “type A” individual, struggled with feeling “substandard” when her energy and drive diminished. Learning to extend grace to oneself during these challenging periods is vital for healing.
7. The Importance of Options and Accessible Resources
Perhaps the most resonant takeaway from Sabra’s story is the profound importance of having options and access to resources. When depression takes hold, the ability to seek out and evaluate different pathways to healing can be severely impaired. This is where comprehensive, accessible resources like Recovery.com become invaluable.
“I think to know that there are many options, but you have to find the one that works for you because there’s not one right solution and it might be a multitude of things,” Sabra wisely advised.
A platform that allows individuals to explore various treatment modalities, filter by location, insurance, and specific conditions, can significantly reduce the barrier to seeking help. When someone is at their lowest, the thought of navigating complex healthcare systems can be overwhelming. A streamlined resource that presents available options empowers individuals to take that crucial first step.
“Because having options is a lot better than not having any options,” the hosts concluded, summarizing the core message of Sabra’s empowering narrative.