This article summarizes a heartfelt conversation from the Giving Voice to Depression podcast, hosted by Terry McGuire. In Episode 357, “The Power of Yet: Reclaiming Hope,” Terry and co-host Dr. Anita Sanz revisit Lori’s deeply personal journey through persistent depression. With remarkable honesty, Lori shares the painful truths, small victories, and gentle shifts that helped her reclaim a sense of hope after nearly a decade of feeling stuck.
This article isn’t about “quick fixes” or magic solutions. It’s about the power of small steps, the importance of connection, and the courage it takes to remain open to the possibility of change—even when hope feels out of reach. Whether you are navigating depression yourself or walking alongside someone who is, these insights offer gentle reminders that healing is possible—even if you haven’t found the right path yet.
1. Understand That You Are Not Broken, You Are Stuck
The most profound realization Lori took away from her treatment experience was one that challenged the very foundation of how she saw herself:
Lori: You don’t need to be fixed because you’re not broken. You’re just stuck.
Those words softened years of self-blame. Because broken feels permanent. It suggests damage that cannot be undone. But stuck? Stuck means there’s still a way forward. Maybe not easily, maybe not quickly—but forward nonetheless.
Why this matters:
- Stuck means temporary. Broken feels hopeless.
- Stuck suggests there is a way through. Broken suggests there is not.
- Stuck invites compassion. Broken fuels shame.
If you are struggling, please hear this: You are not broken. You are not beyond help. You are stuck—and stuck is something that can change.
2. Know That You Are Not Alone
For so many people living with chronic depression, one of the heaviest burdens is the belief that they are the only one who feels this way. Lori expressed this beautifully when she said:
Lori: I didn’t know anybody at all like me that just lived with that all-the-time depression.
That sense of isolation can deepen despair and reinforce the lie that something is uniquely wrong with you. But Lori’s experience at the treatment center introduced her to others who shared similar struggles. It was life-changing.
Lori: It maybe just took a little bit of the burden off of me just thinking that it was just me.
Ways to remind yourself you’re not alone:
- Join a peer support group
- Listen to stories like Lori’s and others on Giving Voice to Depression
- Seek community through online mental health forums
Connection breaks isolation. It chips away at the lie that you are the only one.
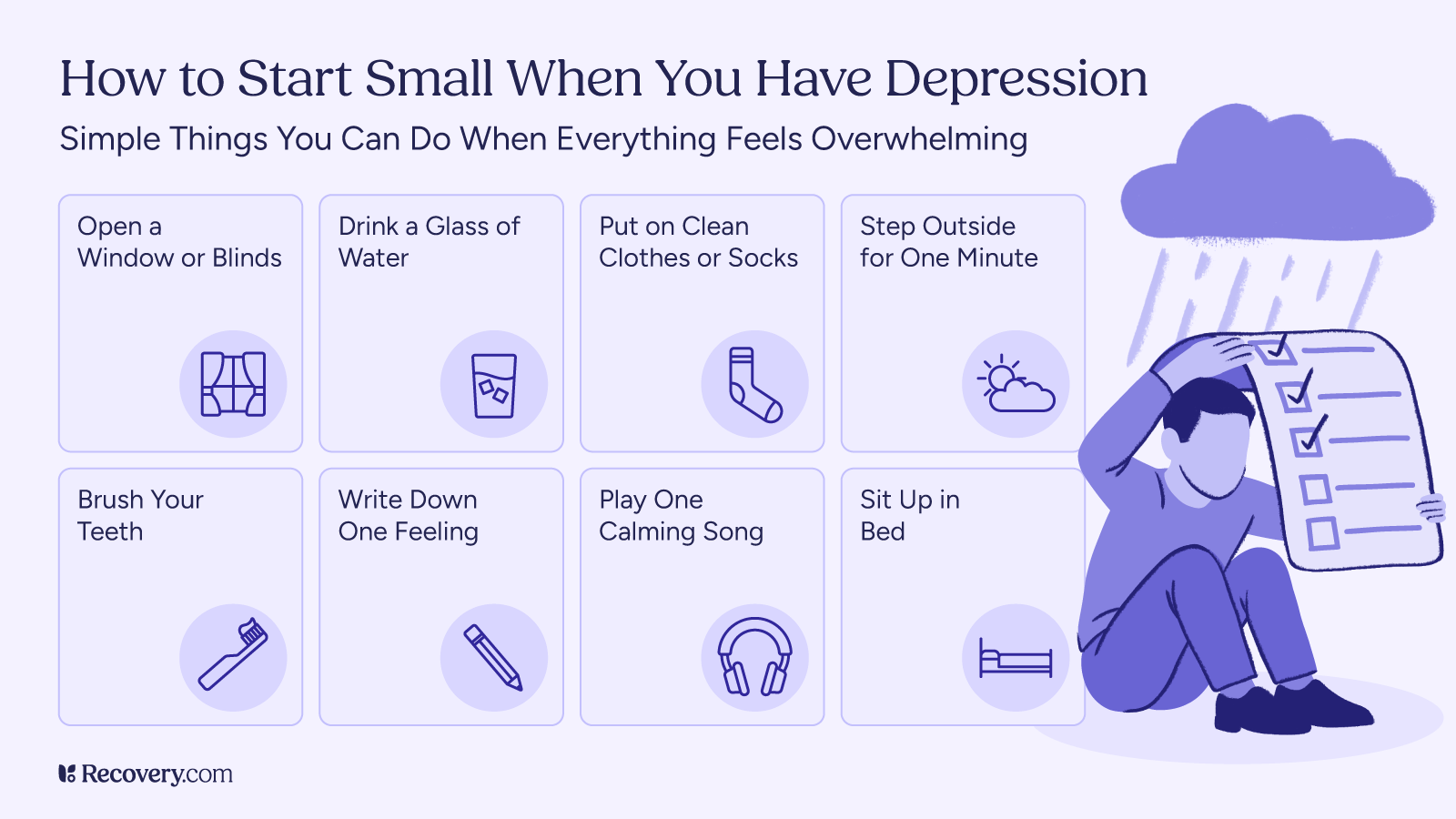
3. Make Small, Consistent Shifts
One of the most powerful lessons Lori learned was the importance of small, manageable changes—what she calls “tiny shifts.”
Lori: They said, what if you’re willing to shift your thinking like one degree? Not 180 degrees—one degree.
It can be tempting to believe that healing requires radical transformation. But often, it’s the small, consistent adjustments that move us toward a better place.
Think of an airplane changing course by just one degree. Over time, that tiny shift leads to an entirely different destination. It’s the same with depression recovery.
Gentle suggestions:
- Try one new coping tool
- Adjust your inner self-talk by just one phrase
- Commit to one small act of self-care each day
You don’t have to overhaul your life. You just have to be willing to try something different—even one degree different.
4. Embrace the Power of “Yet”
Throughout the episode, Terry and Dr. Anita reflect on the significance of one small word: yet. It’s a word that keeps the door to possibility cracked open, even when hope feels impossible.
Instead of saying:
- “I’m not better.”
Try saying:
- “I’m not better yet.”
- “I haven’t found what helps yet.”
“Yet” acknowledges the reality of where you are without closing the door on where you could go. It’s an invitation to remain open to the possibility of change—even if that change hasn’t arrived today.
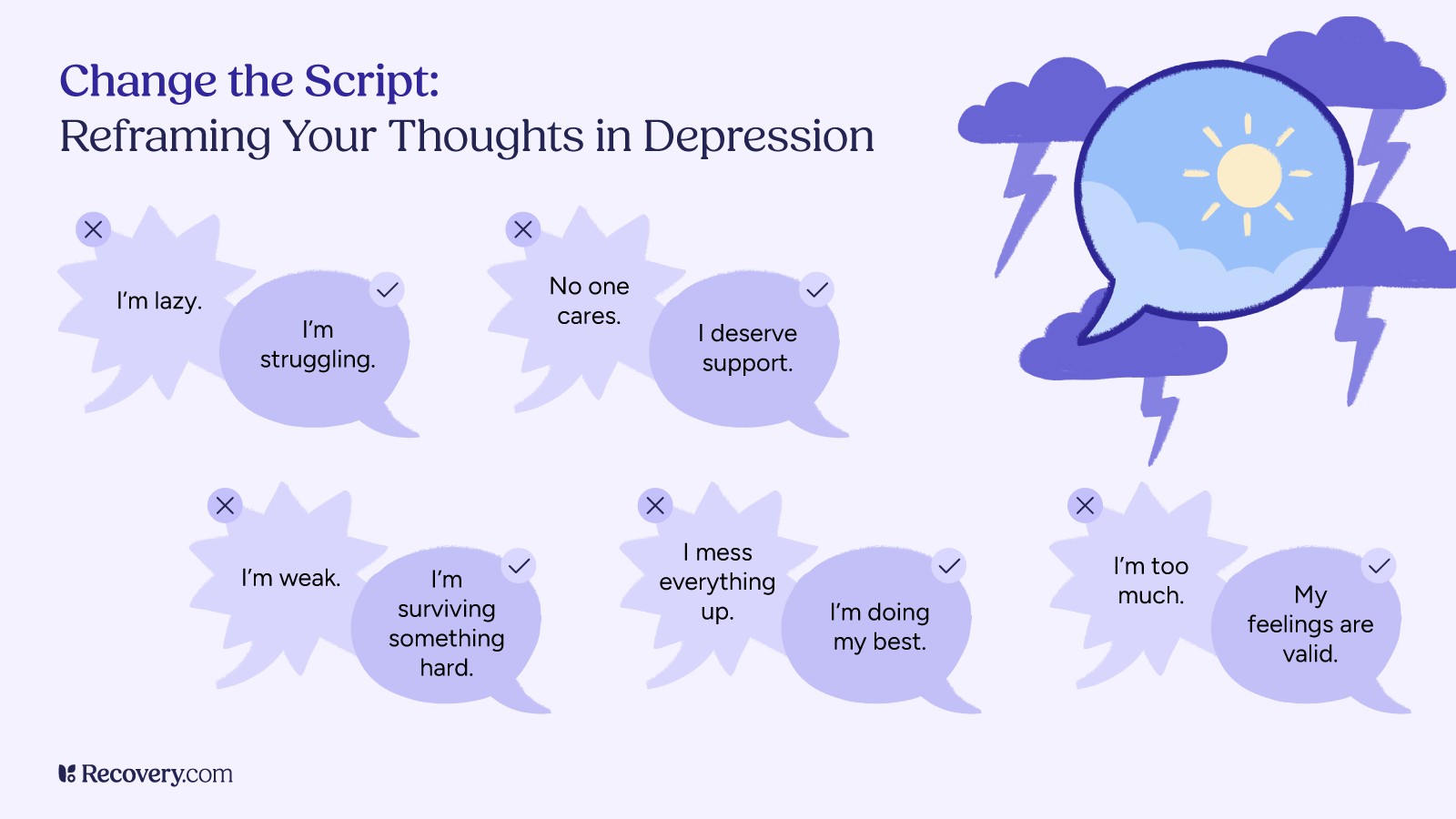
5. Recognize Depression’s Lies
Depression is more than sadness. It’s a master manipulator—a voice that whispers cruel, believable lies about your worth and your future.
Lori: I always wanted somebody to fix me. I’m like, why can’t somebody fix me? Why can’t meds fix me, why can’t a counselor? Why can’t I be fixed? And they said, you don’t need to be fixed because you’re not broken. You’re just stuck.
Depression lies when it tells you:
- “You are worthless.”
- “You will always feel this way.”
- “Nothing will ever help.”
As Terry gently reminds listeners:
Terry: Of course, every message you’re getting is ‘Nothing will change and you’re not worth it,’ but that’s the lie.
To counter these lies:
- Speak your truth out loud
- Challenge the negative thoughts, even when they feel convincing
- Surround yourself with people who remind you of your value
6. Honor Your Past Without Letting It Define You
Lori shared how easy it was to live in the story of her past—believing that the failures and pain behind her were proof that nothing could change.
But one small shift in thinking changed everything:
Lori: Your past is very important… but now what? How do you get through the rest of your life?
Acknowledging where you’ve been is vital. But staying stuck there keeps you from moving forward. Healing invites us to carry the lessons, not the weight.
Ways to let go of the past’s grip:
- Mindfulness practices that anchor you in the present
- Forgiveness work (especially self-forgiveness)
- Compassionate self-reflection instead of harsh judgment
7. Lighten Your Load: From Backpack Person to Screen Door Person
One of the most memorable metaphors Lori shares is the idea of being a “backpack person” versus a “screen door person.”
Lori: I was a huge backpack person. Everything that happened to me—and to others—I put it in my backpack and carried it. It just got so heavy.
When we carry every hurt, every disappointment, and every responsibility like stones in a backpack, the load becomes unbearable. Lori learned to let go of that weight, choosing instead to let life’s experiences “blow through” like air through a screen door:
Lori: I don’t need to cling to it. I don’t need to judge it. I don’t need to carry it.
Visualize this:
- Notice what you’re packing into your backpack
- Ask yourself what you can let go of today
- Picture yourself as a screen door—allowing life to flow through without trapping it inside
8. Redefine Your Worth: You Don’t Have to Earn It
A major shift for Lori came when she realized how much of her pain was tied to contingent self-worth—the belief that her value had to be earned through success, perfection, or selflessness.
But in treatment, she heard a truth that helped her begin to break free from that cycle:
Lori: My worth is a set point. It’s not changeable.
Your worth is not up for debate. It is not based on your productivity, your weight, your income, or how many people you please. It is inherent. It is constant. It is yours.
Daily reminders:
- “I am worthy as I am.”
- “My worth does not fluctuate.”
- “I do not have to earn the right to take up space.”
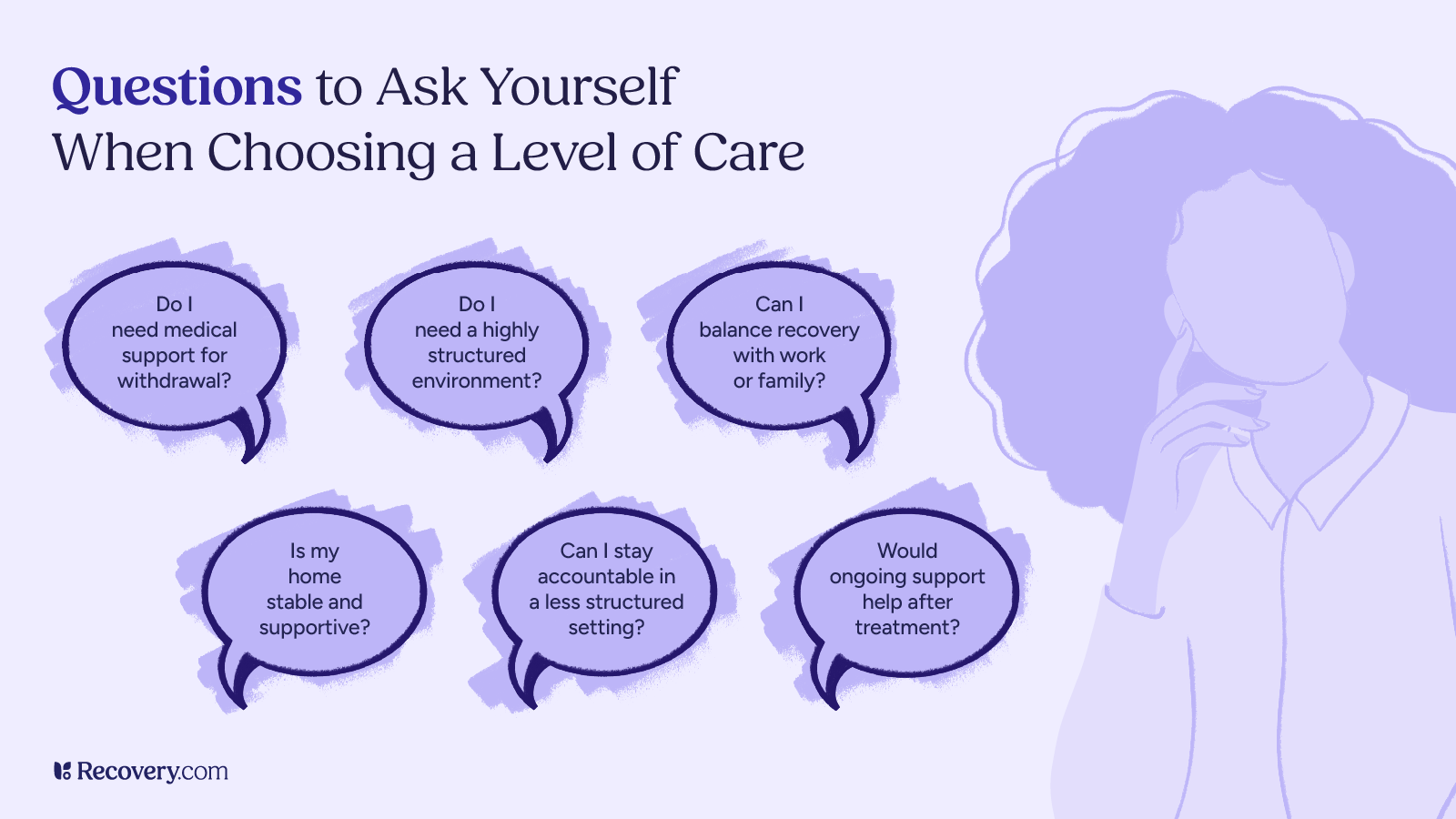
9. Stay Open-Minded About What Might Help
Lori’s healing journey didn’t look like what she expected. In fact, some of the tools that made a difference were things she might have dismissed before.
As Terry observed:
Terry: There may be gourd painting, and it’d be real easy to be like, ‘Oh, hell no.’ But the act of doing that shifted something.
The truth is, we never know what might open a door, spark a shift, or offer relief. Sometimes, what seems silly or “not for me” turns out to be the thing that helps the most.
Stay open to:
- Creative outlets
- Mindfulness exercises
- Group experiences you’ve never tried before
Remember Anita’s words of wisdom: “Never say never.”
10. Trust That Slow Progress Is Still Progress
Healing is not linear. There are no straight lines in this journey, and there is no timeline you “should” be on.
Lori: It took a lot of years—my whole lifetime—to get to where I was. I can’t just spin on a dime and everything’s different now.
But even with that reality, Lori noticed something beautiful: the dread that once met her every morning had begun to soften.
Lori: I don’t go to bed at night fearing having to wake up the next morning. I don’t wake up feeling severely disappointed because I wish I hadn’t. I’m slowly doing better, and I’m not in any rush to get better or be happy—but I’m noticing more contentment in my days. And that’s enough for now.
Let this be your encouragement:
- Slow is okay
- Small is meaningful
- “Enough for now” is still enough
Final Thoughts: You Are Worthy of Hope and Healing
Lori’s story is a powerful reminder that even when depression feels like it has stripped away every ounce of hope, there are still paths forward—even if they are small, even if they are slow, even if you haven’t found them yet.
Terry: Depression is too dark a road to walk alone.
Please remember: you are not alone. You are not broken. You are worthy of support, compassion, and hope.
Healing may not happen overnight. But with each small step, each gentle shift, and each courageous act of staying open to the possibility of something new, you are moving forward.
And sometimes, that’s the bravest thing we can do.