Alcoholism doesn’t happen overnight. For many people, it develops gradually through several stages, each with its own set of signs and challenges. Understanding these stages can help you recognize problems in yourself or your loved one and intervene before the consequences get worse.
The Disease Model: How Alcoholism Progresses
This framework for understanding alcoholism progression comes from E.M. Jellinek, the first to propose the disease model of alcohol addiction that’s now widely accepted by medical professionals. His model outlines 4 distinct stages that show how alcohol dependence develops.1
Let’s break down each stage in simple terms so you know what to watch for.
Stage 1: Pre-Alcoholic Stage
In this early stage, a person starts using alcohol not just for enjoyment, but to feel better. They might drink to relax after work or to feel more comfortable at parties. This might not seem like a problem yet, but it’s the start of using alcohol as a solution rather than a choice.
Signs you might be in the pre-alcoholic stage:
- You look forward to drinking alcohol as a way to unwind or feel comfortable
- You can handle more alcohol than before (increased tolerance)
- You sometimes drink alone
- You finish alcoholic beverages faster than others around you
- You feel a little anxious when you can’t drink
Most people in this stage still function normally in daily life. Friends or family may not notice anything unusual about your drinking habits.
This is the easiest stage to make changes. Try setting limits on your drinking, tracking how much you consume, or finding alcohol-free ways to relax and socialize.
Alcohol use doesn’t just suddenly become a problem—issues with alcohol use can build slowly over time, in ways that are easy to overlook. By understanding the stages of alcoholism, we can better identify early warning signs and intervene before more challenges and consequences occur.
— Caroline Beidler, MSW
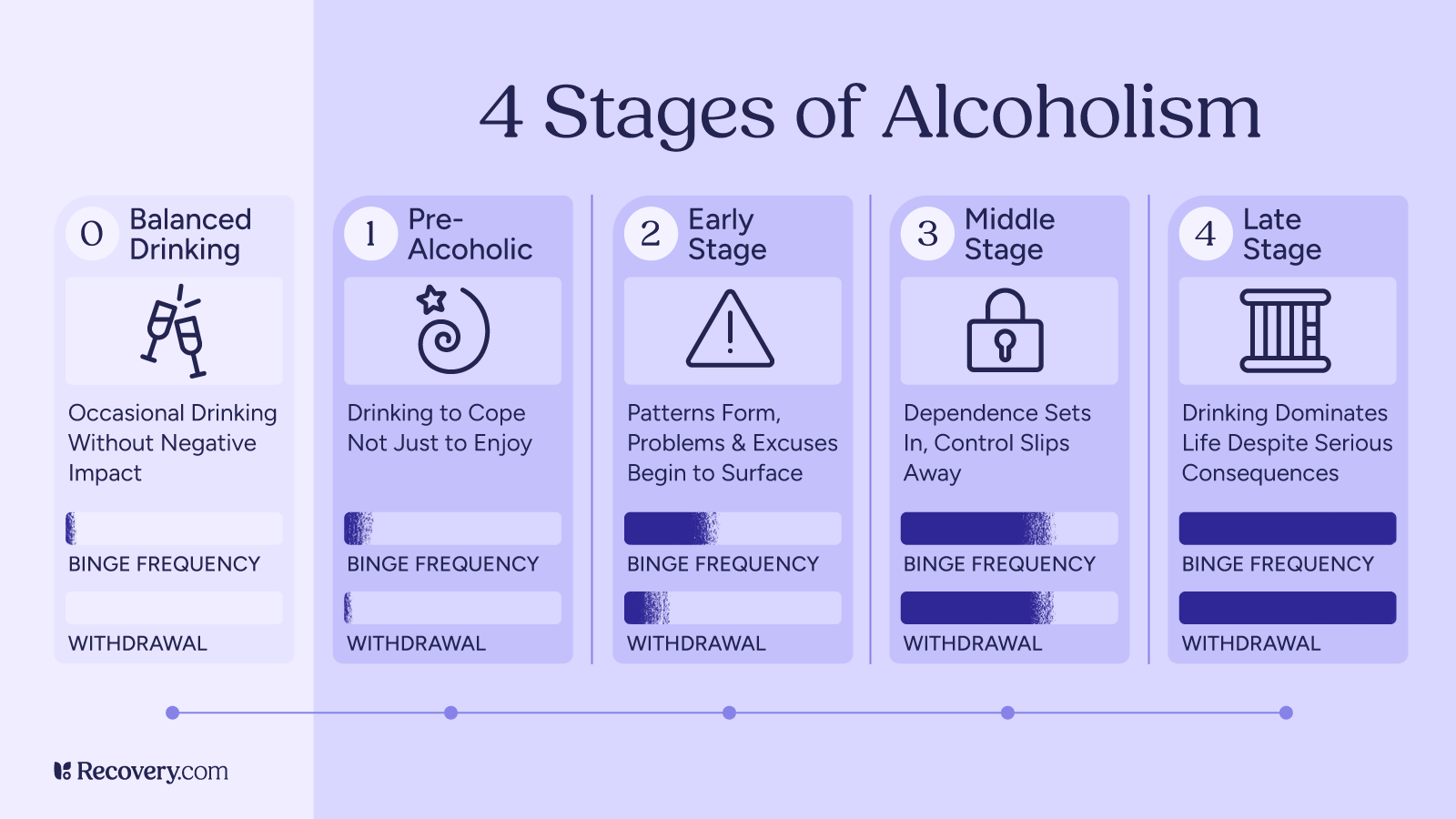
Stage 2: Early Stage
In the early stage, casual drinking shifts toward a more concerning pattern and early warning signs begin to appear. The person develops regular drinking routines, and alcohol starts causing problems.
Finding the Right Support
- You experience occasional blackouts (can’t remember what happened while drinking)
- You feel defensive when someone mentions your drinking
- You make excuses for drinking or downplay how much you consume
- Your relationships start to suffer because of alcohol
- You drink to deal with problems caused by previous drinking
During this stage, a dangerous cycle begins. Drinking causes problems, which creates stress, which leads to more drinking to cope with that stress. Getting help at this stage is still relatively easy, and the chance of successful recovery is high with proper support.
Stage 3: Middle Stage
The middle alcoholic stage (or “crucial” stage) is when physical dependence takes hold. Your body now expects alcohol regularly, and you feel uncomfortable without it. Many people realize they have a problem at this point and try to control their drinking.
Signs of the middle stage:
- You feel withdrawal symptoms when you’re not drinking2 (shakiness, anxiety, sweating)
- You’ve tried to cut back or quit but couldn’t maintain it
- You hide your drinking from others
- You sometimes need a morning drink to steady your nerves
- You black out more often
- You feel deep shame or guilt about your drinking
- Hangovers get worse because your body’s ability to process alcohol is compromised as liver function declines
- Physical health problems start to appear
People often try ineffective methods to control their drinking, like switching from liquor to beer or limiting drinking to weekends. These attempts usually fail without adequate support.
Many people in this stage keep up appearances outwardly while struggling privately. They might hold down jobs and maintain relationships—however problematic—while denying the severity of their problem.3
Stage 4: Late Stage
The late stage (or “chronic” stage) is when alcohol abuse completely takes over and a person feels a total loss of control over their drinking. It’s no longer a choice but a powerful compulsion that directs most of their decisions and behaviors.
Signs of the late stage:
- You can’t control when or how much you drink
- You have severe withdrawals when not drinking
- You’ve abandoned activities and interests you once enjoyed
- Your work performance has significantly declined
- Relationships are severely damaged or broken
- You continue drinking despite serious physical and mental health problems
- You may have had alcohol-related legal issues like DUIs
Alcohol-related health complications4 are an increased risk at this stage. Liver damage or cirrhosis, heart problems, digestive bleeding, and changes in brain function are common. You may have visible symptoms even when you’re not drinking.
Despite how serious this stage is, recovery is still possible with professional help. Medical treatment is usually necessary, starting with medically supervised detox followed by comprehensive addiction treatment.
Things began innocently enough when I began drinking socially in high school, but quickly escalated when I realized how much more confident I felt when intoxicated. It was a bad combination that I used for many years in social settings, to numb out “bad feelings” and ultimately use alcohol as daily self-medication. I trained my brain and body to think they “needed” alcohol for any kind of stressful situation or negative emotion. This was very destructive for me and eventually I had to make a change or I didn’t know what might progress even further.
— Ericka Anderson
Understanding Alcohol Addiction
Substance use is commonplace in many aspects of our daily lives. From celebrating achievements to unwinding after a stressful day, drinking is normalized in ways that can mask developing problems. This cultural acceptance can make it hard to recognize when casual drinking is crossing into problematic territory.
Health experts increasingly recognize “gray area drinking“—a space between moderate consumption and severe alcohol use disorder. In this middle ground, you might not meet the clinical criteria for addiction, but your relationship with alcohol is causing subtle problems in your health, relationships, or daily functioning.
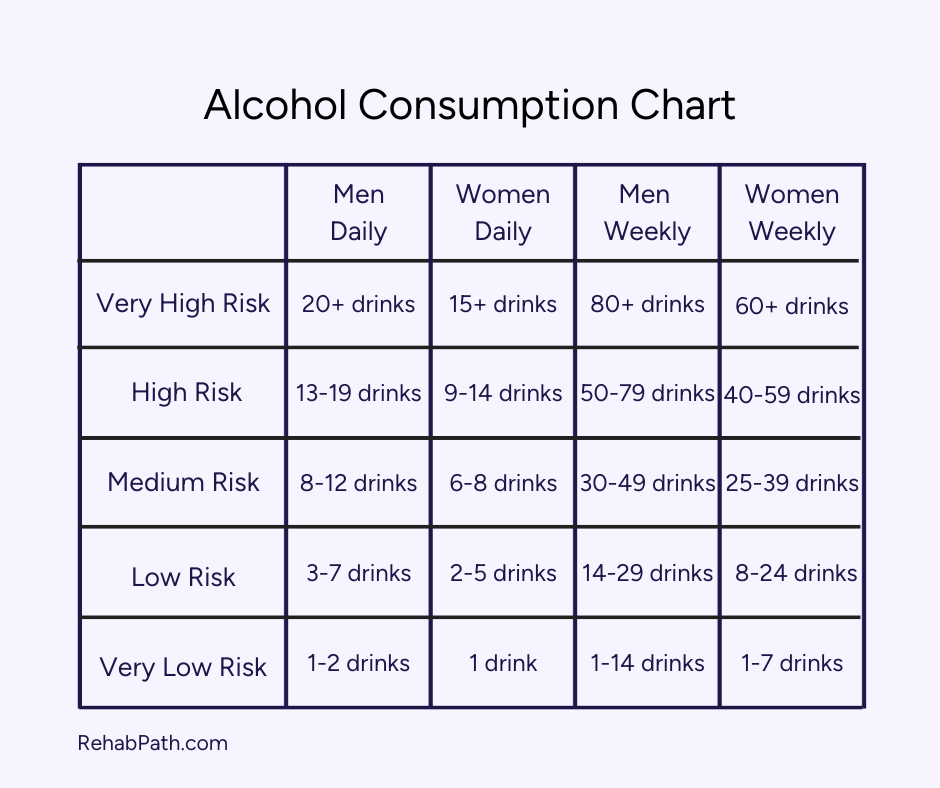
Many people exist in this gray area without realizing it: The 2023 National Survey on Drug Use and Health by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) found that 10.2% of people in the U.S had an alcohol use disorder.5 People regularly exceed the limits for moderate drinking (or even heavy drinking or binge drinking) without noticing. (According to medical guidelines, moderate drinking6 means up to 1 drink daily for women and 2 for men.)
While most people can drink moderately without causing immediate problems in their lives, research increasingly shows there is no completely “safe” amount of alcohol consumption7 when it comes to long-term health outcomes.
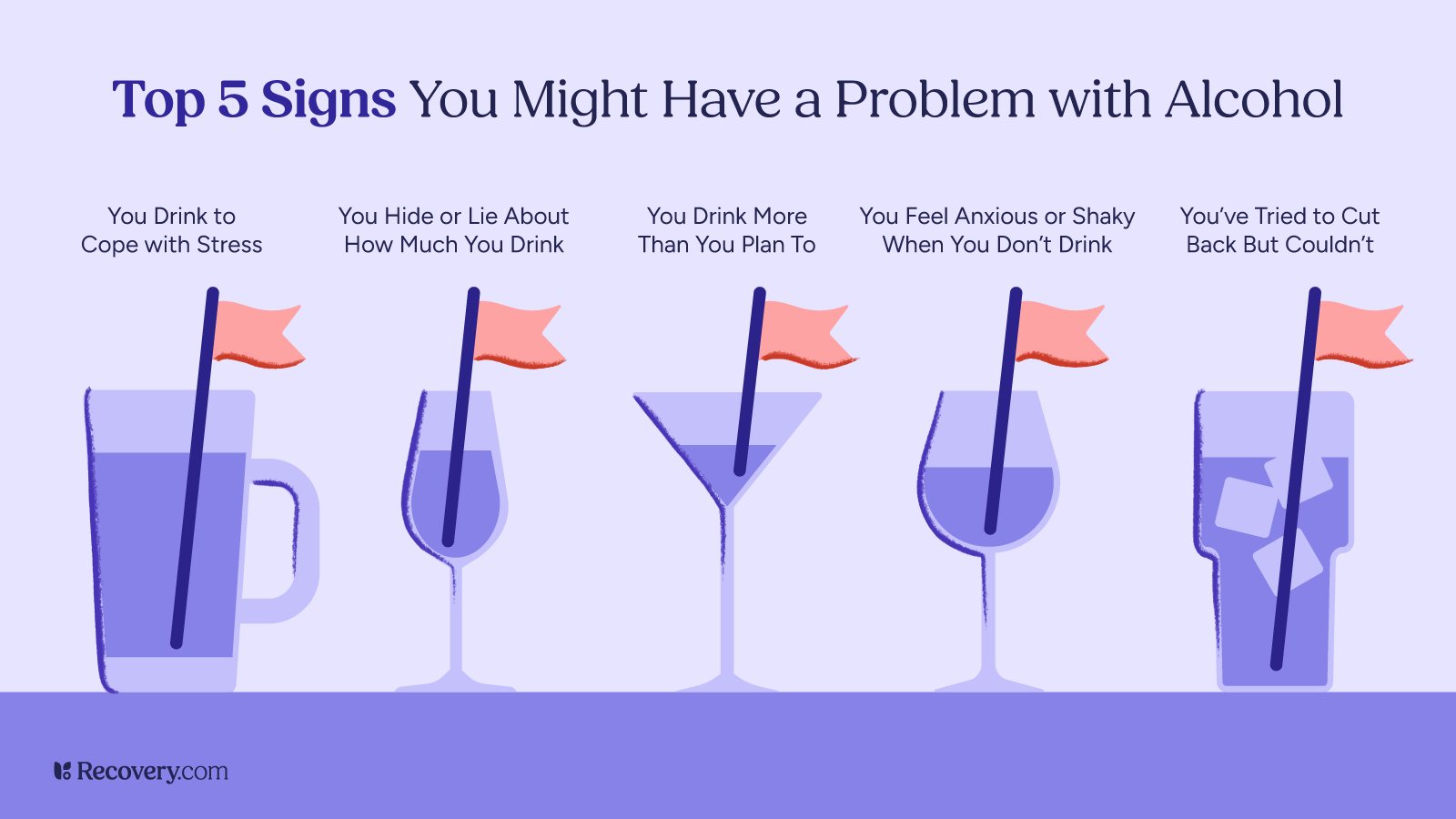
Consider these warning signs about your drinking habits:
- Do you often drink more or for longer than planned?
- Have you found it hard to stop or cut back, despite wanting to?
- Do you find yourself preoccupied with thoughts of drinking?
- Have you noticed yourself prioritizing drinking over activities or hobbies you used to enjoy?
- Are your relationships with family or friends being affected by your alcohol misuse?
- Do you sometimes take risks while drinking, like driving or having unsafe sex?
- Do you need more drinks to feel the same effects of alcohol?
- When you stop drinking, do you have any physical discomfort like shakiness, trouble sleeping, or nausea?
If you answered yes to more than one of these questions, it could indicate problem drinking.8 Recognizing these patterns doesn’t necessarily mean you have a diagnosable addiction, but they are important signs that your relationship with alcohol could benefit from some attention and possibly professional help.
Recovery Is Possible at Any Stage
No matter which stage of alcoholism you may be experiencing, recovery is always possible. Many people have found their way to healthier, happier lives after struggling with alcohol, and you can too.
Alcohol treatment options include:
- Medical detox to safely manage alcohol withdrawal and cravings
- Inpatient alcohol rehab for structured, intensive care
- Outpatient programs that allow you to live at home while attending intensive therapy
- Sober living homes that provide a supportive, alcohol-free environment as you transition to independent living
- Continuing care: Ongoing counseling, support groups like AA or SMART Recovery, and social support
These resources can help you start the process:
- Your primary care doctor (who can refer you to addiction specialists)
- The Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline: 1-800-662-HELP (4357)
- Local Alcoholics Anonymous (AA) or other support group meetings
Wondering what might work best for you? Check out our complete guide to finding an addiction treatment program for an easy-to-use breakdown of programs, costs, and how to choose the right fit for your needs.
Recovery is not only possible, it is probable when we have the right supports and treatment.
— Caroline Beidler, MSW
A Note on the Modern Understanding of Alcohol Use Disorder
While Jellinek’s stages offer a helpful framework for understanding how alcohol problems typically progress, modern medicine has evolved toward a more nuanced approach. The current Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR) views alcohol problems as existing on a spectrum9 rather than in distinct stages.
Today, healthcare professionals diagnose alcohol use disorder (AUD) as mild, moderate, or severe based on how many criteria a person meets out of 11 possible symptoms. This spectrum approach recognizes that alcohol problems can develop in different ways for different people. Some individuals may experience certain symptoms but not others, and the progression isn’t always linear. Both models offer valuable perspectives for understanding how casual drinking can develop into more serious problems over time.
Find the Right Support for Your Journey
If you’re concerned about your relationship with alcohol, reaching out for professional guidance is a great first step. Whether your goal is to reduce harm from drinking or stop entirely, an addiction specialist can point you in the right direction and help you stay on track.
Our addiction treatment finder helps you explore options that match your specific needs, connecting you with qualified treatment providers who can support your path to a healthier life.
FAQs
Q: What are the 4 stages of alcoholism?
A: The 4 stages of alcoholism in Jellinek’s disease model are:
- Pre-alcoholic stage, where drinking is used to cope with stress
- Early stage, where patterns form and blackouts may begin
- Middle stage, where physical dependence develops with withdrawal symptoms
- Late stage, where excessive drinking becomes compulsive and health complications become serious
Q: How does alcohol addiction progress through different stages?
A: Alcohol addiction typically begins with using alcohol to cope with problems (pre-alcoholic stage). It progresses to regular patterns of drinking that cause life problems (early stage), then to physical dependence with withdrawal symptoms (middle stage), and finally to compulsive drinking despite serious consequences (late stage).
Q: What are the early signs of alcohol dependence?
A: Early signs of alcohol dependence include:
- Needing more drinks to feel the same effect (increased tolerance)
- Looking forward to drinking as your main way to relax
- Drinking alone more frequently
- Feeling anxious when you can’t drink
- Occasional blackouts
- Becoming defensive when others mention your drinking
Q: How can I identify the different stages of alcoholism?
A: You can identify the stages of alcoholism by looking for specific signs:
- Pre-alcoholic stage shows increased tolerance and drinking to cope
- Early stage includes blackouts and making excuses for drinking
- Middle stage involves withdrawal symptoms and failed attempts to quit
- Late stage is marked by compulsive drinking, severe health conditions, and an inability to control consumption
Q: What is late-stage alcoholism and what are the effects?
A: Late-stage alcoholism involves compulsive drinking where a person loses control over their alcohol consumption. Side effects include severe withdrawal symptoms, abandoned interests and activities, declining work performance, broken relationships, serious health complications (liver damage, heart problems, brain damage), and alcohol-related legal issues.
Q: Where can I find help for alcohol addiction?
A: Help for alcohol addiction is available through your primary care doctor, local support groups, and specialized treatment centers. Recovery.com is here to help. Options range from medical detox and inpatient programs to outpatient care and harm reduction approaches like setting drinking limits or creating alcohol-free days.