Although alcohol may be legal and normalized, it’s associated with various health risks and negative consequences. Physically, alcohol’s toxins contribute to liver disease, heart disease, and specific types of cancer1. Alcohol’s danger can go beyond disease, harming your relationships, mental health, and well-being2, as well. This stems from its psychoactive properties, which can impair judgment, coordination, and control, leading to risky behaviors and a propensity for addiction.
Alcohol impacts everything from individual health to society as a whole. Safe consumption and preventive measures can help minimize these unhealthy effects.
How Can Alcohol Affect Your Life?
Unsafe alcohol consumption can cause a ripple effect that touches nearly every facet of your life.
Alcohol can lead to strained family relationships and even domestic violence3. Children in families where alcohol use is prevalent are at a higher risk of experiencing emotional and behavioral problems4. They may also be at greater risk of developing substance use problems later in life.
Professionally, alcohol use can lead to poor performance5, absenteeism, and, ultimately, job loss. An unstable source of income can cause financial problems and volatile relationships.
Socially, alcohol can lead to behaviors that strain relationships, such as aggression6, social withdrawal, and engaging in illegal activities. It can also result in legal repercussions ranging from fines for public intoxication to more serious charges like driving under the influence (DUI), which can have long-term consequences on a person’s legal record and employment opportunities.
How Is Alcohol Unhealthy?
Alcohol is a toxin that metabolizes to an acetaldehyde7, which are highly reactive molecules that can damage DNA, proteins, and lipids. Alcohol remains in the bloodstream until it is metabolized by the liver, therefore damaging liver tissue; however, it is highly diffusible through cell membranes and is metabolized by most tissues. Thus, its toxicity affects most organs.
Regular consumption significantly increases the risk of developing chronic diseases1, such as liver cirrhosis, cardiovascular diseases, and certain forms of cancer.
Alcohol dependence, known as alcoholism, is a particularly dire health consequence that involves a preoccupation with alcohol, compulsive drinking, and high tolerance and withdrawal symptoms. This disease not only deteriorates physical health but also mental well-being, contributing to conditions such as depression and anxiety.
Short Term Effects of Alcohol
Immediately after consumption, alcohol begins to alter mind and body functions8. Physical effects can include slurred speech, impaired motor skills, and a delayed reaction time, which can be particularly dangerous when operating vehicles or machinery. Alcohol is a diuretic, meaning it increases urine production and can lead to dehydration. It can irritate the stomach lining, leading to nausea and vomiting. Additionally, drinking too much can weaken your immune system9, making the body a much easier target for disease after a single occasion of drinking.
Drinking also produces cognitive side effects, such as reduced inhibitions and poor judgment, increasing the likelihood of making decisions that can have serious repercussions. Alcohol can also affect short-term memory, and in higher amounts, it can lead to blackouts, where the drinker cannot remember what happened while under the influence.
Long Term Effects of Alcohol
Chronic alcohol use wreaks havoc on the body. The long-term effects of alcohol on the body can be severe and wide-ranging, affecting virtually every organ system. Prominently, it damages the liver, heart, brain, stomach, and kidneys.
Liver
The liver is particularly vulnerable, as it’s the primary site for alcohol metabolism. Unhealthy alcohol consumption levels can cause hepatic lesions in the liver10, leading to alcoholic fatty liver, alcoholic hepatitis, fibrosis, and, ultimately, cirrhosis. A liver with cirrhosis has permanent damage and scar tissue that can cause liver failure.
In advanced stages, liver damage from alcohol can be irreversible and may necessitate a liver transplant. Chronic alcohol consumption also increases the risk of developing liver cancer, particularly hepatocellular carcinoma, the most common type of liver cancer. This risk is especially high in individuals with alcoholic cirrhosis.
The liver is crucial to metabolizing and detoxifying all substances. Maintaining liver health is vital to prevent serious complications and health risks.
Heart
Long-term effects on the heart can suddenly manifest as severe health events with long-lasting consequences11. Alcohol misuse can lead to:
- Hypertension: Alcohol activates the central nervous system and parasympathetic nervous system12 in a way that causes blood vessel muscles to constrict, leading to high blood pressure.
- Cardiomyopathy: Alcoholic cardiomyopathy, damaging the hearts’ muscles, can be caused by the substance’s inflammatory effects.
- Arrhythmias: Chronic heavy drinking and binge drinking can lead to irregular heartbeats, known as arrhythmias. The most common type associated with alcohol is atrial fibrillation, where the upper chambers of the heart experience chaotic electrical signals, leading to an irregular heartbeat. This can increase the risk of stroke, heart failure, and other heart-related complications.
- Stroke: Excessive alcohol intake is linked to an increased risk of both ischemic and hemorrhagic strokes. Ischemic stroke occurs when a blood clot blocks or narrows an artery leading to the brain, while a hemorrhagic stroke is caused by a blood vessel in the brain bursting.
Brain
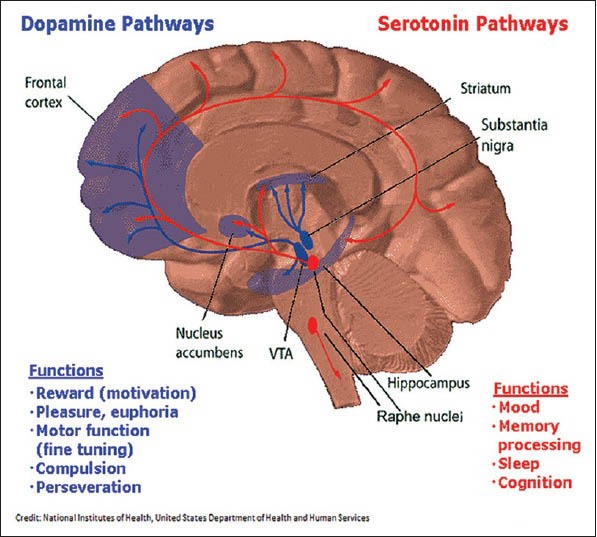
Alcohol can lead to neurodegeneration13, or neuron destruction, and permanent brain damage. As heavy drinking alters neurons and their pathways, the brain’s neural networks cannot properly communicate and function with itself and the body. Without healthy networks, brain health can severely decline, resulting in problems with cognition, memory, and coordination.
Chronic abuse can also increase the risk of developing mental health disorders14, including depression and anxiety. Alcohol can act as self-medication for uncomfortable emotions associated with these mental disorders, leading to dependency. Chemical changes in the brain from alcohol, such as the disruption of neurotransmitters crucial in maintaining good mental health, also contribute to and worsen existing symptoms.
Stomach
Both acute and chronic alcohol consumption can interfere with stomach functioning15. For example, alcohol—even in relatively small amounts—can alter gastric acid secretion, injure gastric muscles, and interfere with gastric and intestinal motility (how easily food travels through the system). Therefore, alcohol’s toxic and inflammatory effects can not only hinder digestion, but also cause long-term issues such as gastritis (irritated and inflamed stomach lining) and ulcers.
Kidneys
Drinking can compromise the kidneys’ ability to regulate the volume and composition of fluid and electrolytes in the body16. In addition to their role in regulating the body’s fluid composition, the kidneys produce hormones that influence a host of physiological processes, including blood pressure regulation, red blood cell production, and calcium metabolism. Alcohol’s toxic effects can completely alter how kidney cells function.
Harming these systems can lead to an increased risk of kidney stones and kidney disease. Over time, an imbalance of water, hormone levels, and bodily waste can negatively impact overall health.
Immune System
High amounts of alcohol consumption can leave the body susceptible to infections and slower recovery from illness16.
Alcohol can damage the protective epithelial cells lining the gut, skin, and lungs, reducing the body’s first line of defense against pathogens. This damage can increase the likelihood of bacterial infections and bacteria entering the bloodstream from the gut.
Alcohol consumption can also reduce the production and function of lymphocytes, including T-cells and B-cells, weakening the body’s ability to develop long-term immunity and produce antibodies in response to infections.
Chronic alcohol use can lead to prolonged inflammation, which can itself cause tissue damage and lead to a variety of chronic diseases.
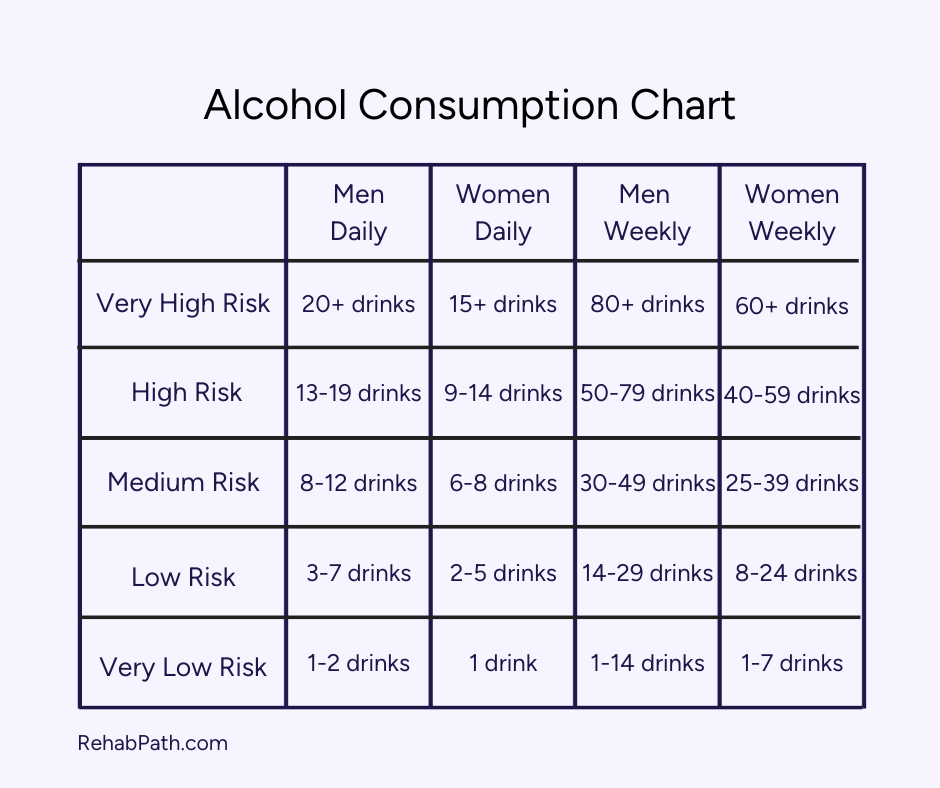
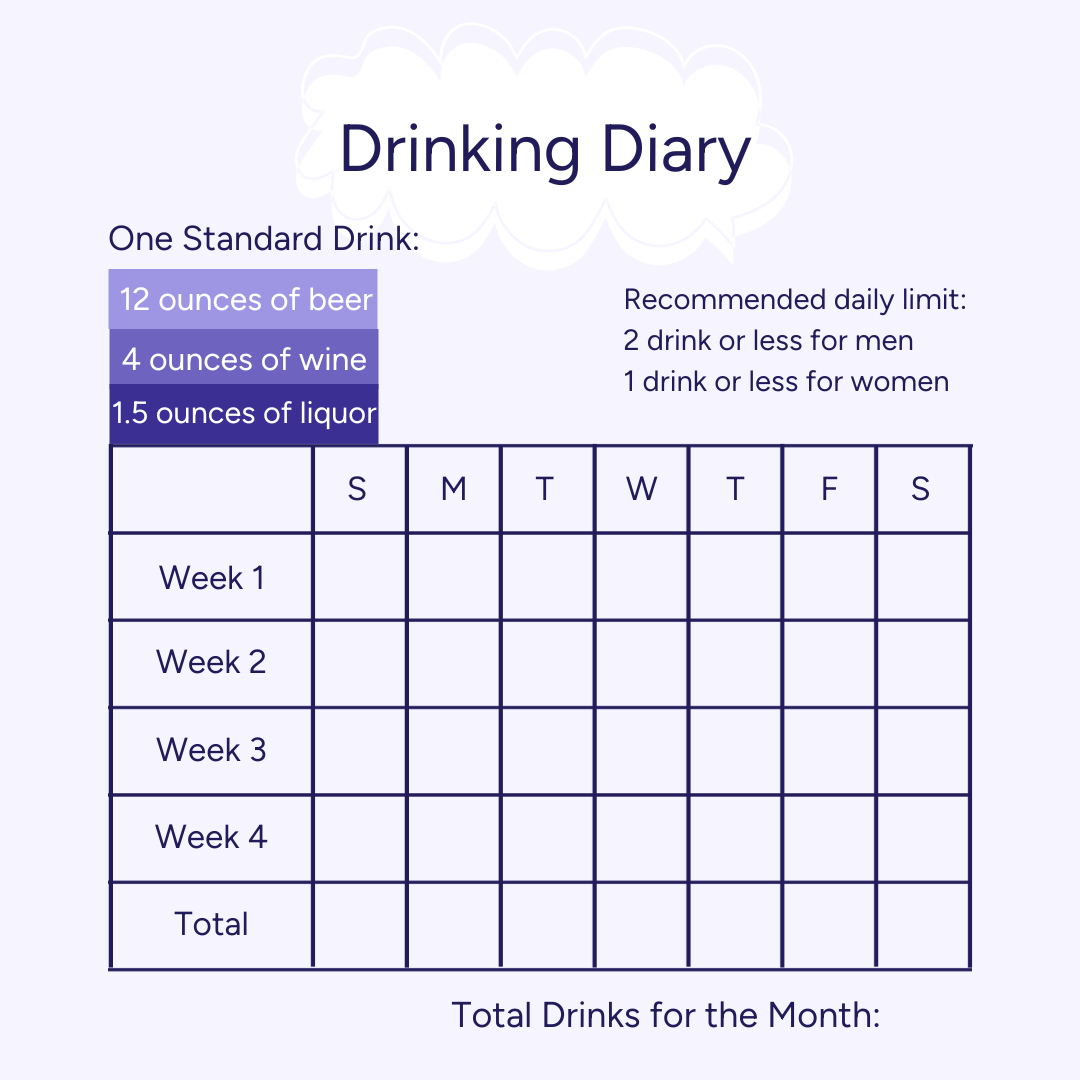
Is There a Safe Amount of Alcohol?
While moderate alcohol consumption might fit into a healthy lifestyle for some, defining ‘safe’ levels of consumption is complex. Guidelines can vary significantly, taking into account factors such as gender, age, medical history, and medications.
The idea of a universally ‘safe’ amount of alcohol is increasingly scrutinized, and the best recommendation often comes from someone’s healthcare providers. The most effective way to avoid negative health consequences is to not drink at all.
Find Treatment For Alcohol
If you’re experiencing the damaging effects of alcohol, you can choose to break the cycle. Professional support is available, designed to help people with struggles exactly like yours. Getting help can place you on the path to a fulfilling, sober life.
Explore alcohol addiction treatment centers to learn about their programs, pricing, insurance coverage, and more.