If your loved one is addicted to drugs or alcohol, you can make an impact in their life by supporting their recovery journey. Being a positive support for your loved one can help them navigate the transition to treatment, and life afterwards. If the addicted person doesn’t have a strong support network, they could easily fall back to old patterns. You can be that powerful motivator.
There are resources available to help work through addiction at all stages of rehabilitation. You can start the journey by finding addiction treatment to start the healing process today.
What To Do: How to Help Someone With an Addiction
Here are 9 ways you can help a loved one who’s struggling with addiction.
1. Educate Yourself
Addiction is not necessarily “curable,” but with understanding and guidance, it is possible to successfully manage the ups and downs of it. Education is key for family and loved ones to provide the best support to those affected by addiction. Empowering yourself through knowledge helps you through the recovery process.
The Biology of Addiction
When you take drugs, they interrupt how neurotransmitters communicate in the brain1. Addiction begins when your brain produces less of its natural neurotransmitters due to high, constant drug use. You can build up a tolerance and need to take more of the substance. At first, using drugs or drinking alcohol is a choice, but it can soon spiral out of control.
Eventually, some neurotransmitter networks and areas of the brain become damaged from the constant disruption. Because of this, addiction changes your brain chemistry, so many scientists believe that it is a disease. In some ways, you can look at addiction like cancer or diabetes. It’s an ongoing disease that, luckily, can be treatable. As the Centers for Disease Control and Prevention (CDC) thoughtfully puts it, “addiction is a disease, not a character flaw2.”
2. Recognize The Signs of Relapse
Just like other diseases, relapse is always possible. So, being aware of warning signs is crucial. Everyone’s triggers are different, but common ones include stress and trauma.
If your loved one is about to relapse, you might notice them fudging the truth, keeping secrets, or lying about their whereabouts. They could also show other changes in behavior such as:
- Being withdrawn or distant
- Showing a loss of interest in activities they like
- Displaying mood swings
If you notice this, you may want to start gathering resources for help and talk to a professional.
3. Listen
Be compassionate with your loved one. Ask them questions about why they drink or use drugs. And speak without judgment. Getting them to trust you with this vulnerable information is the first step towards getting them the help they need.
3A. Be open-minded: Ask questions that can help your loved one reflect on their addiction and their progress. Don’t judge the person or their decisions. Show that you are open to different approaches and solutions.
4. Be Patient
This process can be a great opportunity to show your loved one how much you care. Being patient and empathetic throughout their recovery journey will help them through difficult times and be greatly appreciated. Let the person know that you care and understand what they are going through. Your presence and support will be invaluable to them.
5. Vocalize Your Support
Sometimes, we think actions speak louder than words, but voicing your support of this journey is so important. Just saying, “I love you, and we’re going to get through this together” can encourage your loved one during a confusing and difficult time. Here are some more supportive phrases for recovery:
1. “I’m here for you no matter what.”
2. “I’m proud of you for seeking help.”
3. “I believe in you.”
4. “I’m here to help.”
5. “You can do this.”
Words of Support and Encouragement for Your Loved One During Their Recovery Journey.
6. Set Healthy Boundaries
Prioritize yourself and your wellbeing while helping your loved one. It is a difficult process, so remember to take a break when needed. It’s okay if you are unable to be involved in every aspect of their healing. If a situation becomes heated, consider setting a boundary such as taking a break from the conversation to reflect and come back to it in a more peaceful mindset.
7. Have Realistic Expectations
Change doesn’t happen overnight. Be patient and supportive of your family member/friend’s journey of recovery. Celebrate each step of progress they make and encourage them to keep going. Don’t expect instant results, as change takes time and effort. Remind them that with perseverance, anything is possible. Be their source of hope and strength.
8. Offer resources
Suggest helpful resources or support groups that may be beneficial. Your loved one may want to look into different groups like Alcoholics/Narcotics Anonymous3, Women for Sobriety4, or SMART Recovery5. They can also explore our resource center with different articles to learn more about their condition or recovery in general.
9. Research Treatment and Recovery Resources
One of the biggest ways you can help your loved one is by getting them professional treatment. Rehab, outpatient programs, and/or therapy all teach clients the tools they need to regulate their emotions and behaviors to reinforce their sobriety.
What Not To Do:
This is a sensitive time, and there are some things you might want to avoid to keep the recovery journey on track.
1. Don’t Enable
While you want to support your loved one, there’s a fine line between support and enabling. Don’t give your loved one money or a place to stay if their predicament results from drug use. Don’t tolerate negative behavior. And don’t rescue them every time they mess up. Instead, hold them accountable and practice tough love.
2. Don’t Blame Yourself or Them
Many factors go into how addiction forms, and you could end up wasting a lot of energy trying to pinpoint the cause. Instead, you can focus on taking action and moving forward to overcome this struggle.
3. Don’t Force Them To Quit
If your loved one feels like they can’t trust you because you demand they quit, that could make matters worse. They might start sneaking around or lying about their actions. And the less you know about their addiction, the less likely you’ll know how to help.
Offer to help them, but don’t demand sobriety immediately.
4. Don’t Ignore The Problem
Pretending an issue doesn’t exist doesn’t make it go away, especially for addiction. By ignoring it, you’re enabling it. You can take concrete steps to better your loved one’s life.
Find a Treatment Program For Addiction
So your loved one admits they need help, now what?
Doing some research to find the best kind of treatment for their needs is a great start.
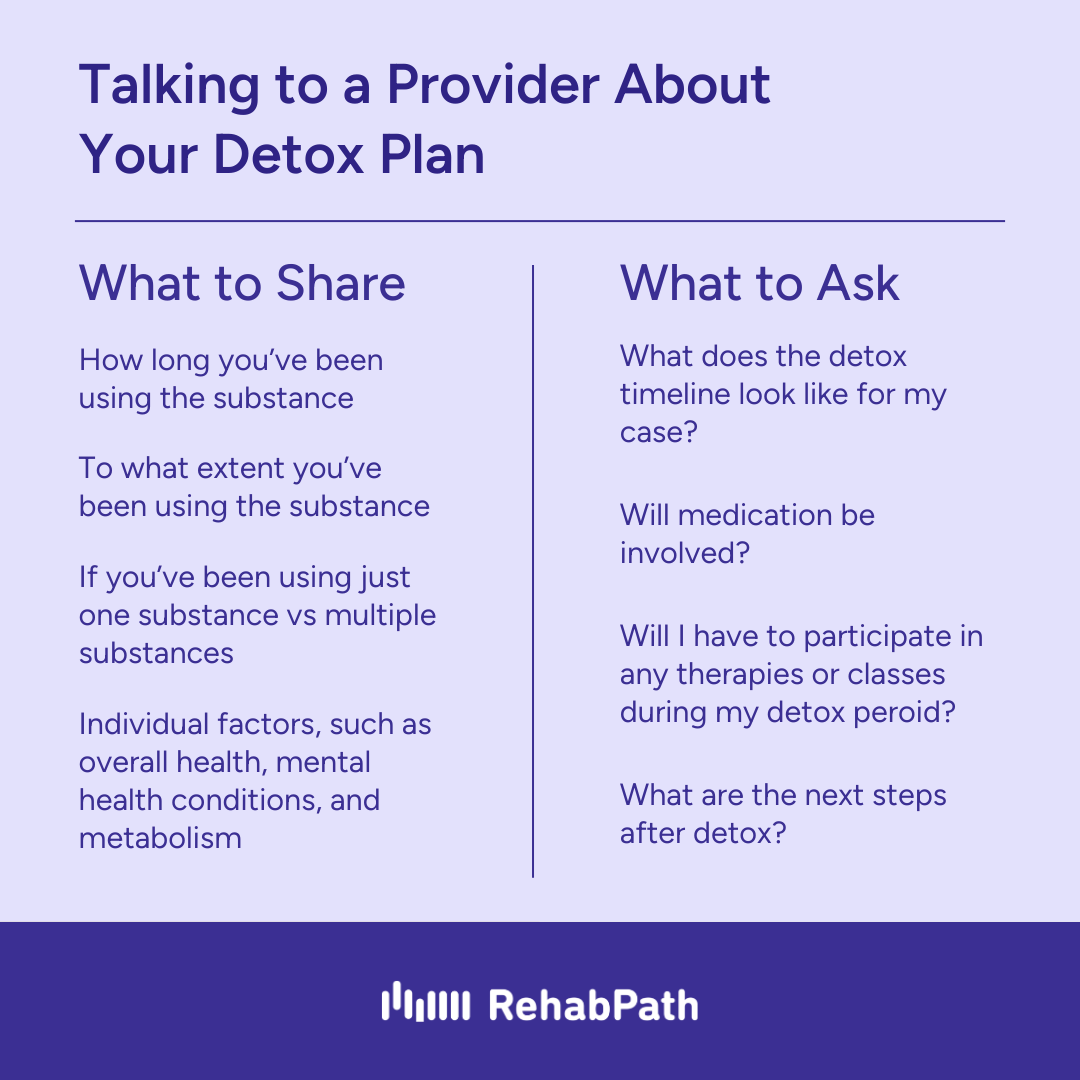
A good, and often necessary, first step in the healing journey is detox. Medically monitored detox safely rids your body of drugs and alcohol and can help you feel clear minded and ready to tackle treatment.
Many people then need residential rehab to overcome their addiction. Residential care can help them replace their unhealthy coping mechanism, substances, with positive habits. They’ll learn new techniques with therapies like cognitive behavioral therapy (CBT) to be well equipped to face the uncomfortable feelings that come with addiction recovery. And they’ll likely engage in holistic activities like yoga for well-rounded healing.
If you’re a family member, you may want to look into a program that offers family therapy. Usually, you’ll work with a therapist and your loved one. Or, they might offer a family weekend for on-site visits. Another key component of family therapy is addiction education. You’ll learn more about the addiction and recovery process, so post-treatment your loved one will have a healthy environment to come home to.
Post-residential care, sober living homes offer more flexibility while providing a comfortable place for your loved one to focus on their sobriety. They’ll likely attend an outpatient program, go to work or school, and grow with other peers in recovery. This is especially great for those who need a stable environment to heal in.
Recovery starts with a single step. You can make an impact in your loved one’s life by reaching out to addiction treatment centers.