What does cross-addiction mean? In short, it means that you have multiple addictions. But there’s a lot more to it than that.
Usually, people with cross-addiction switch out one behavior for another. Sometimes, it’s even called “addiction transfer.” For example, imagine you go to rehab for alcohol addiction, and successfully avoid drinking after the program. But once you return home, you develop a new addiction to cocaine. If something like this happens to you, you might need additional treatment.
Cross-addiction is a unique experience, and recovery can be complex. When you’re ready to plan your recovery, you can start by learning more about what it means to be cross-addicted.
How Does Cross-Addiction Happen?
Researchers are still studying the risk factors for cross-addiction.1 We need more information to fully understand its causes. But data suggests that genetics and stress can make you more vulnerable. Experts also believe that cross-addiction follows 1 of 2 patterns:
- Substituting a past addiction with similar behavior (e.g., quitting gambling and developing a sex addiction)
- Switching between addictions based on their availability, with equally severe symptoms for each one (e.g., recovering from daily heroin use and starting to do cocaine every day)
There are a few reasons this could happen during recovery. For one thing, any kind of addiction hijacks your reward system.2 It can get to the point where addictive behaviors are the only thing that makes you feel a sense of achievement. So developing a new addiction might make you briefly feel that reward again. But we need more data to know how big a role the reward system plays in this process.
How Common Is Cross-Addiction?
Because there are so many possible types of cross-addiction, it’s hard to collect broad data about this condition. But a few specific combinations are especially common:
- People with alcohol addiction are 18x more likely to abuse prescription drugs.3
- As of 2008, an estimated 1.1% of adult Americans had simultaneous alcohol and drug addictions.4 That’s about 2.5 million people.
- There may be a link between food addiction and alcohol abuse. Specifically, studies show that bariatric surgery may increase your risk of alcohol addiction.5 Bariatric surgery, sometimes called weight loss surgery, is one possible treatment for food addiction. In these procedures, surgeons shrink or bypass the stomach to control your appetite.
Some experts compare cross-addiction to relapse.6 While not identical, these issues can have a similar effect on your journey. And data shows that 40-60% of people relapse at least once during recovery.7
Common Cross-Addiction Examples
Cross-addiction can occur with any type of addiction, including substance abuse and compulsive behaviors. Learning about some common cross-addictions can help you protect against them in recovery.
Gambling
Gambling addiction is a behavioral issue. Unlike drug or alcohol addictions, it rarely includes physical symptoms. But it can still get very serious. Compulsive gambling interferes with your financial security, career, and relationships. One study found that gambling addiction often co-occurs with video game addiction.8
Sex Addiction
In moderation, sex can be an important part of your life. But when you start prioritizing sex over all else—including committed relationships, work, sleep, and your physical health—you might have a sex addiction.
While sex addiction isn’t in the DSM-5, it is diagnosed in ICD-11 as compulsive sexual behavior disorder (CSBD).9 This falls under the category of behavioral addiction, or impulse control issues. Data also shows that people with sex addiction often have additional behavioral issues. In one study, nearly 40% of people with sex addiction also had a work addiction.10
Compulsive Shopping
Shopping addiction, also called compulsive buying disorder, is another behavioral addiction. Compulsive shopping increases your risk of drug addiction,11 eating disorders, and depression. Up to 1 in 20 people may have a shopping addiction.
Prescription Medication
Data shows that people with health problems are more likely to abuse prescription drugs.12 This may be an issue of access. If you already have opioid medication in your home, for instance, it’s far easier to abuse. And what’s more, experiencing chronic pain increases your risk of cross-addiction.13 People with chronic pain may have easier access to prescription medication, especially opioids.
Data shows that opioids, marijuana, and alcohol all have similar effects on the brain.14 Addiction to any of these substances can make you vulnerable to abusing the other two.
How to Avoid Cross-Addiction?
Certain coping strategies can help you avoid cross-addiction before it becomes a problem.
Self-Awareness
Until your triggers become intuitive, you can use tools to track your feelings and behaviors. For example, some mood tracker apps let you associate emotions with activities. If you notice that the mood “anxious” usually appears just before an activity like shopping or gambling, you can bring that information to your care team. This self-awareness can help you make changes before developing a new addiction.
Educate Yourself on Cross-Addiction
Learning more about any condition can help you stay safe. If there’s a specific substance or behavior you’re concerned about, start there. Once you understand the risk factors for a type of addiction, you can get the support you need before it becomes a problem.
Group Support
A wealth of data shows that social support is essential during addiction treatment.15 That means something a little different for everyone. You might have a close relationship with friends and family, attend support groups, or live in a sober living environment. In any setting, strong relationships can help you stay grounded throughout your recovery.
Speak With a Professional
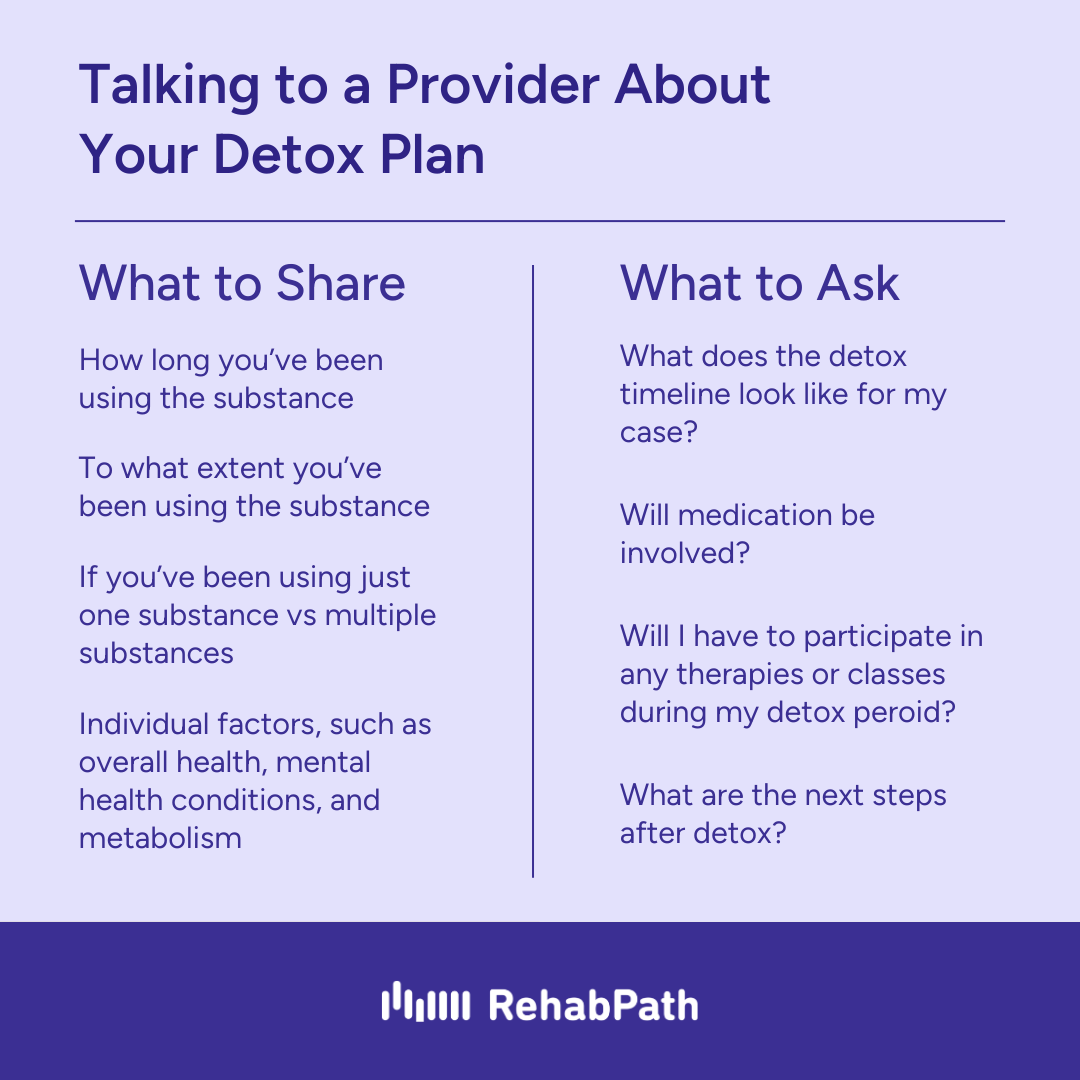
There’s no one-size-fits-all solution for cross-addiction. The right provider can help you navigate the complexities of treatment, offering advice tailored to your needs. With personalized support, you can stay on track to reach your unique goals for recovery.
How to Treat Cross-Addiction
There are nearly infinite types of cross-addiction. You could become cross-addicted to cocaine and gambling, marijuana and alcohol, or sex and video gaming. As a result, there are countless ways to heal from this condition. However, a few treatments stand out:
- Cognitive behavioral therapy (CBT)16 is one of the most popular and effective treatments for any kind of addiction. In this behavioral therapy, you’ll learn to identify triggers and respond to them in new ways. Your therapist will also teach you practical coping skills for real-world situations.
- Contingency management (CM)17 is a treatment that offers patients tangible rewards. For example, if you pass a drug test, you might receive cash or movie tickets. Data shows that CM is highly effective for people with multiple simultaneous addictions. We still need more information about its impact on cross-addiction, specifically.
- Relapse prevention (RP) and mindfulness-based relapse prevention (MBRP)18 teach coping skills and build clients’ self-confidence. Evidence suggests that these treatments protect you against abusing any substance, even ones you haven’t used before.
Find a Treatment for Cross-Addiction
On the road to recovery, cross-addiction is a relatively common hurdle. You can get back on track in a rehab program that treats addiction.