Kratom seems like a mild, harmless drug, but it affects the brain in similar ways to opioids, and withdrawals can be very uncomfortable. Many people feel sick or have intense cravings when they try to cut back or stop using kratom similar to symptoms of opioid use disorder.
Everyone’s experience with kratom withdrawal is different. Some people have mild symptoms while others struggle more. Here’s what to expect to help you mentally prepare, make the process easier, and set yourself up for success.
We’ll take a deeper look at what kratom withdrawal feels like, how long it lasts, and what you can do to help yourself feel better and improve your chances of staying sober. We’ll also talk about when it might be time to get professional support.
What Is Kratom?
Kratom (Mitragyna speciosa) is a tropical tree1 related to coffee that grows naturally in Thailand, Malaysia, Indonesia, and other parts of Southeast Asia. For centuries, local workers chewed the leaves or brewed them into tea to fight fatigue and increase productivity during long workdays. It’s gained popularity in recent years as a recreational drug.
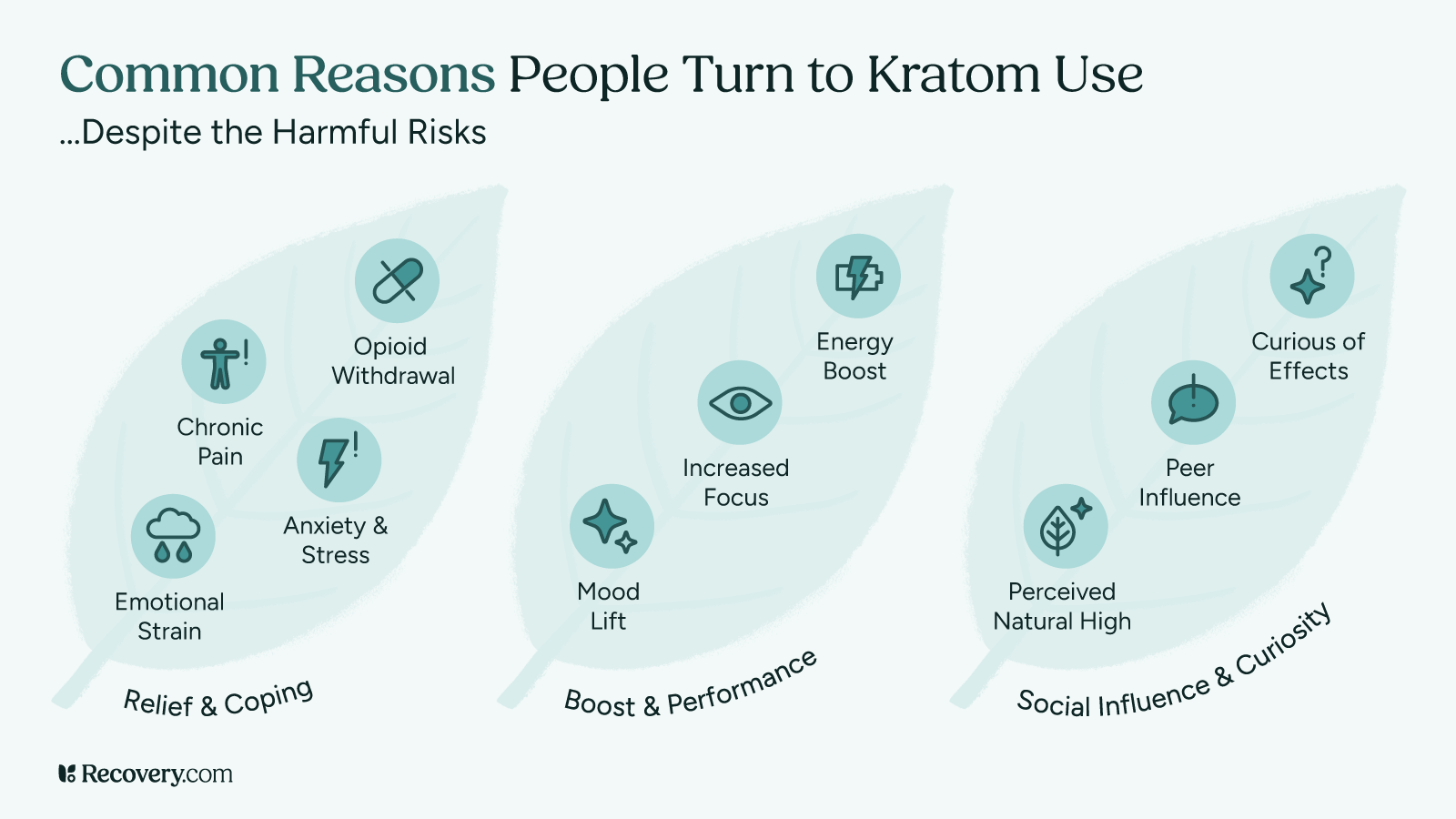
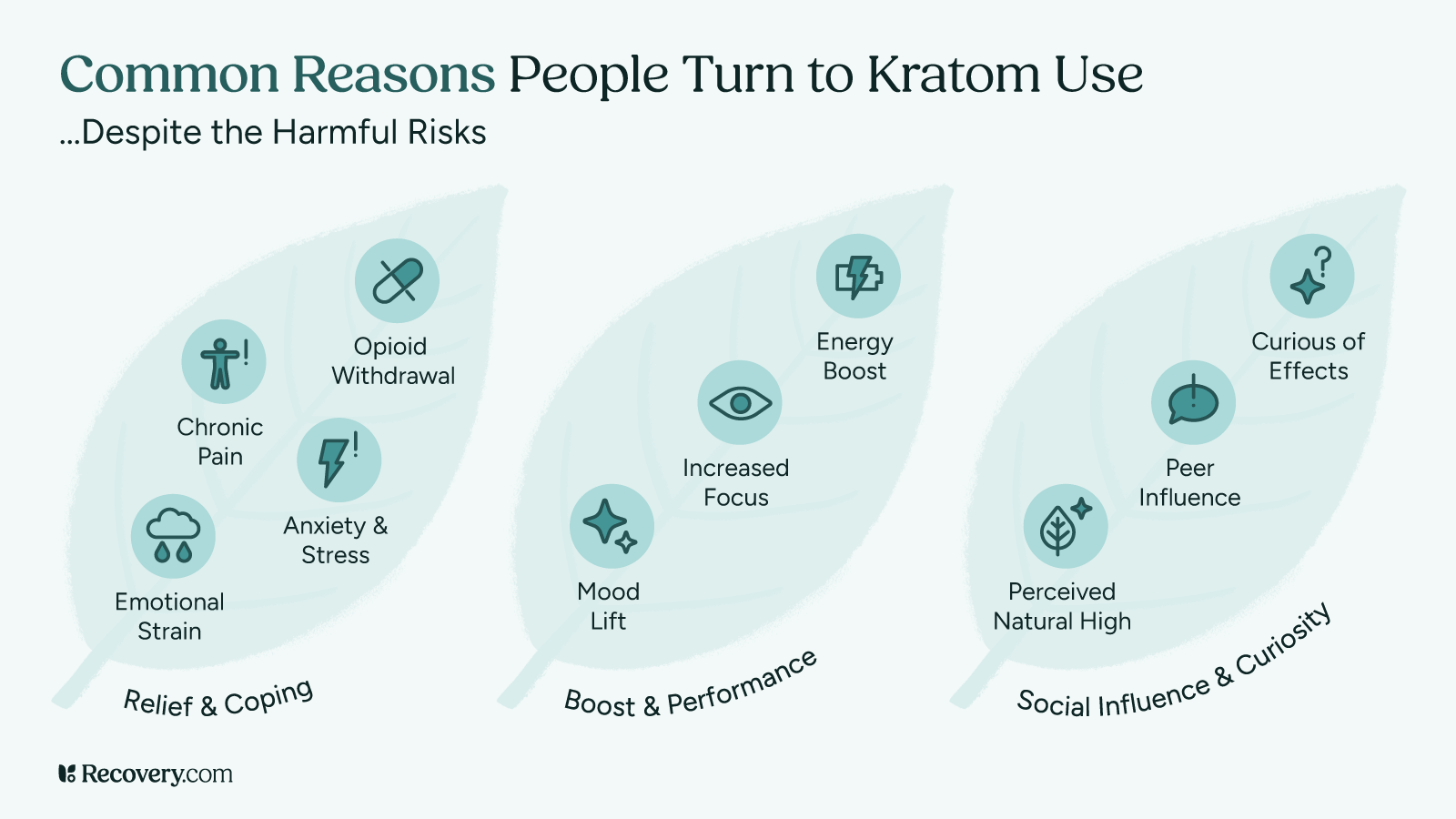
Today, people use Kratom for pain relief or to help with opioid withdrawal. While it might seem helpful at first, regular use can cause you to become physically dependent, making it hard to stop.
How Kratom Works in Your Body
When you take kratom, chemicals in the plant called alkaloids2 (mainly mitragynine and 7-hydroxymitragynine) interact with receptors in your brain. At low doses, these chemicals create mild stimulant effects, making you feel more energetic. At higher doses, the create opioid-like effects,3 producing pain relief and feelings of pleasure or relaxation.
Kratom use is complex because it affects multiple brain systems at once. It activates opioid receptors (like morphine or oxycodone would), but also impacts other systems that regulate your energy and mood. This complex pharmacology explains why kratom can be both stimulating and sedating.
Kratom is not as high-risk as some other substances, but it can have serious side effects that should be taken seriously. Per the National Institute on Drug Abuse (NIDA).
Rare but serious effects have been reported in people who use kratom,4 including psychiatric, cardiovascular, gastrointestinal and respiratory problems.
How People Use Kratom
In the U.S. and other Western countries, people use kratom for various reasons:5
- Managing chronic pain
- Easing opioid withdrawal symptoms
- Self-medicating anxiety or depression
- Boosting energy or focus
- Recreational purposes
Kratom comes in different forms: Powder, capsules, extracts, and teas. Some people chew the leaves directly, while others mix the powder into drinks or food.
See our article on self-medicating with substances to understand if you might be using kratom to cope with underlying issues.
Kratom’s Legal Status
Kratom’s legal status is unclear in many places. The U.S. Food and Drug Administration (FDA) has issued warnings about the safety of kratom6 and has not approved it for any medical use. While kratom remains legal federally in the U.S., several states and cities have banned it.
The Drug Enforcement Administration (DEA) classifies kratom as a “Drug and Chemical of Concern.” Internationally, some countries where kratom grows naturally have made it illegal, and regulations vary widely elsewhere.
This uncertain legal status makes it hard for manufacturers to ensure kratom’s purity and safety7 for those who use it.
Kratom Dependency and Addiction
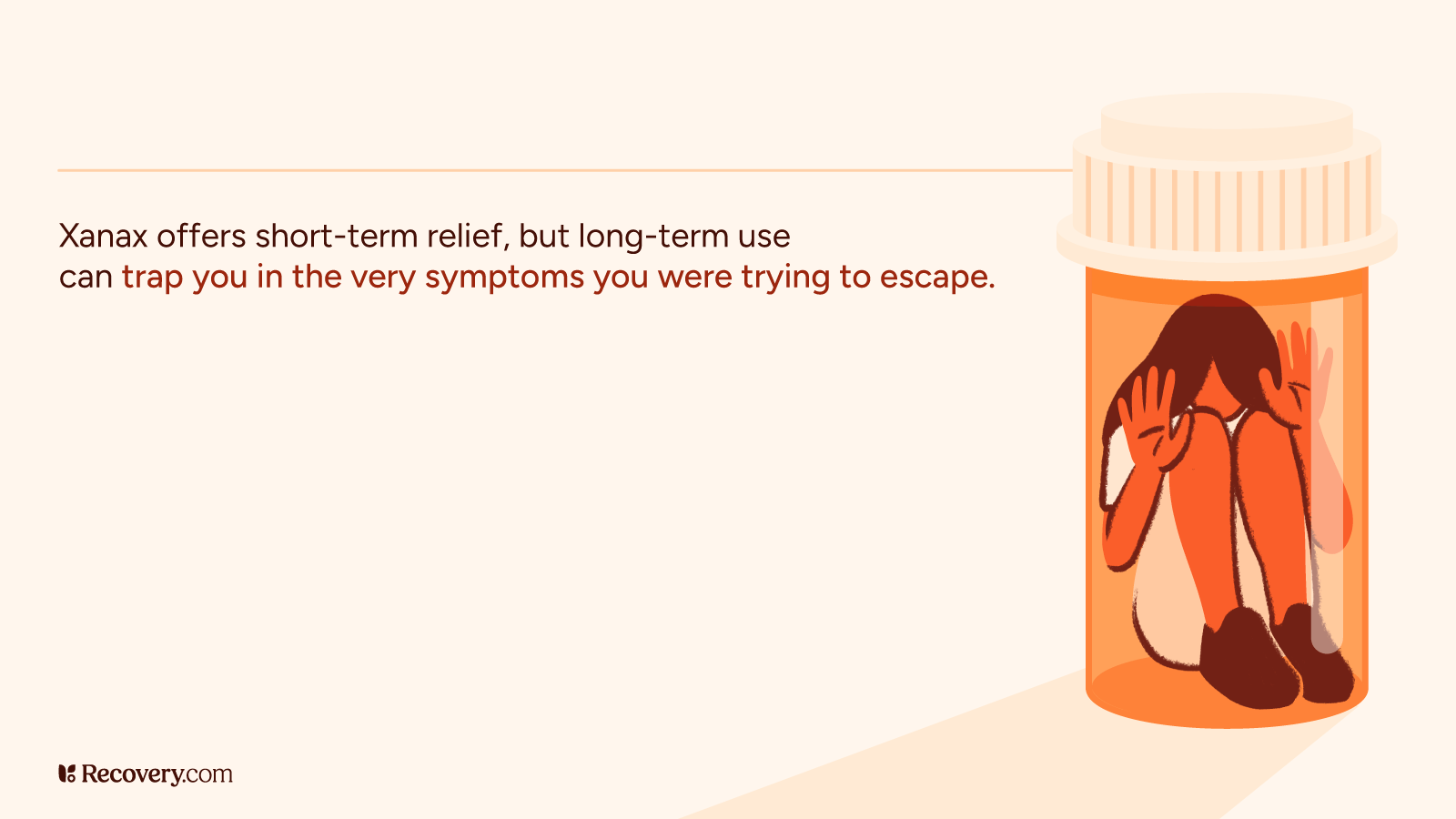
Like many substances that affect your brain, regular kratom use can cause you to become physically dependent.8 This means your body adapts to having kratom in your system and starts relying on it to function normally.
How Dependency Develops
When you use kratom regularly, your brain adjusts to the chemicals it provides. Over time, your brain may produce fewer of its own, natural feel-good chemicals because it’s getting them from kratom instead. When this happens, you might need higher doses to feel the same effects of kratom (tolerance), and your body might react negatively when you don’t have it (withdrawal).
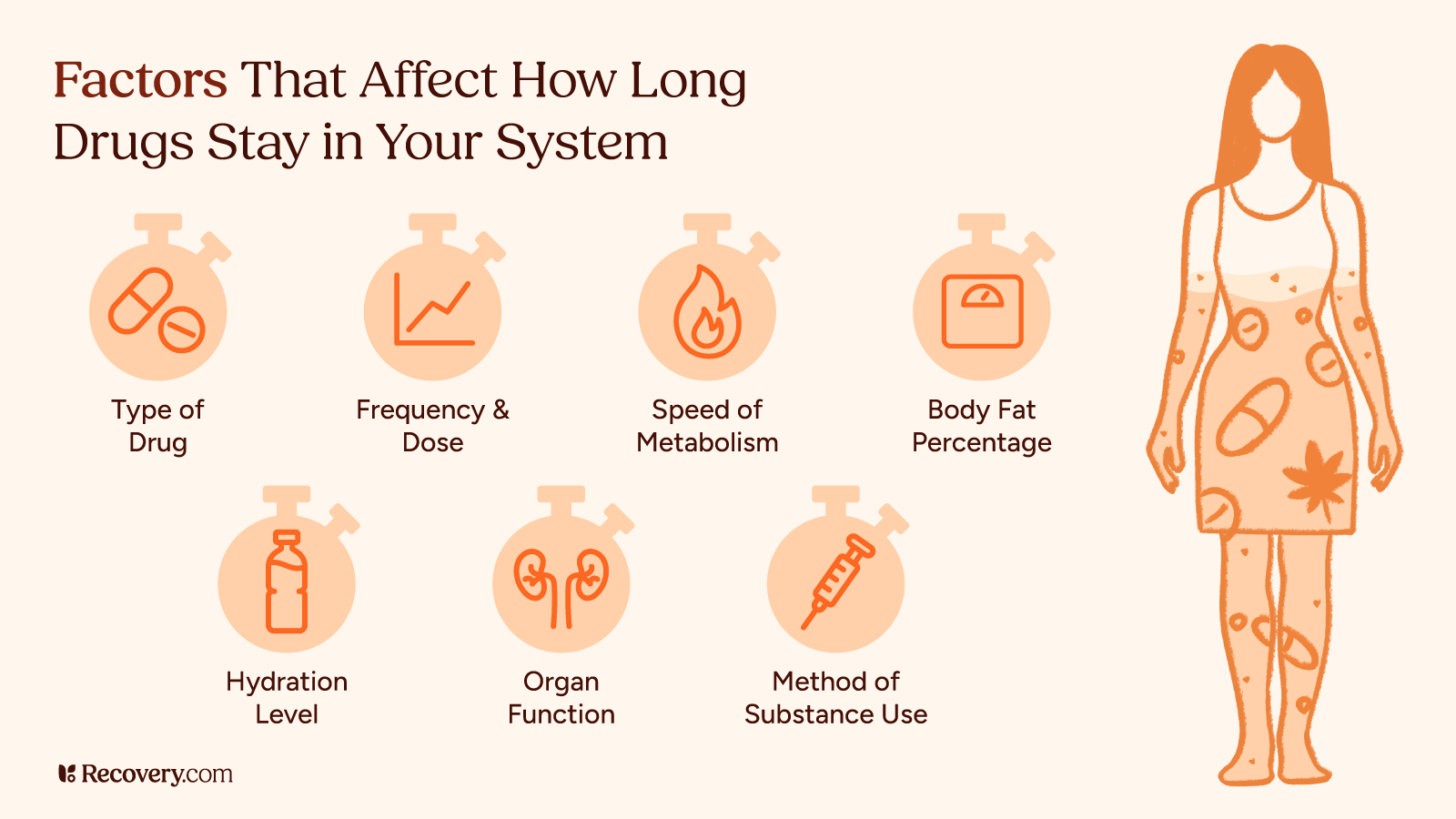
Kratom dependency9 can ramp up in as little as a few weeks of daily use, though it varies from person to person. How quickly you become physically reliant on kratom depends on:
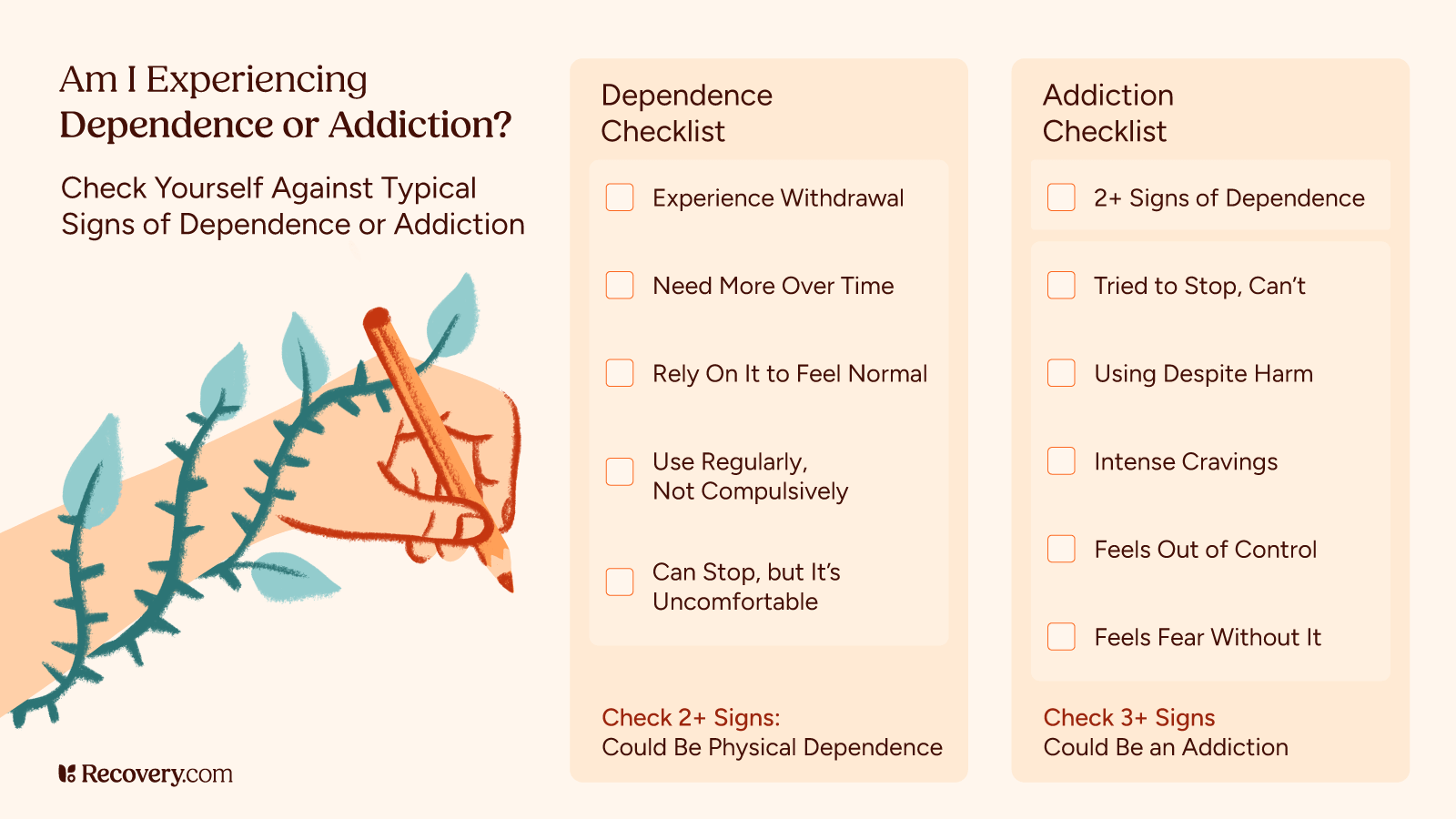
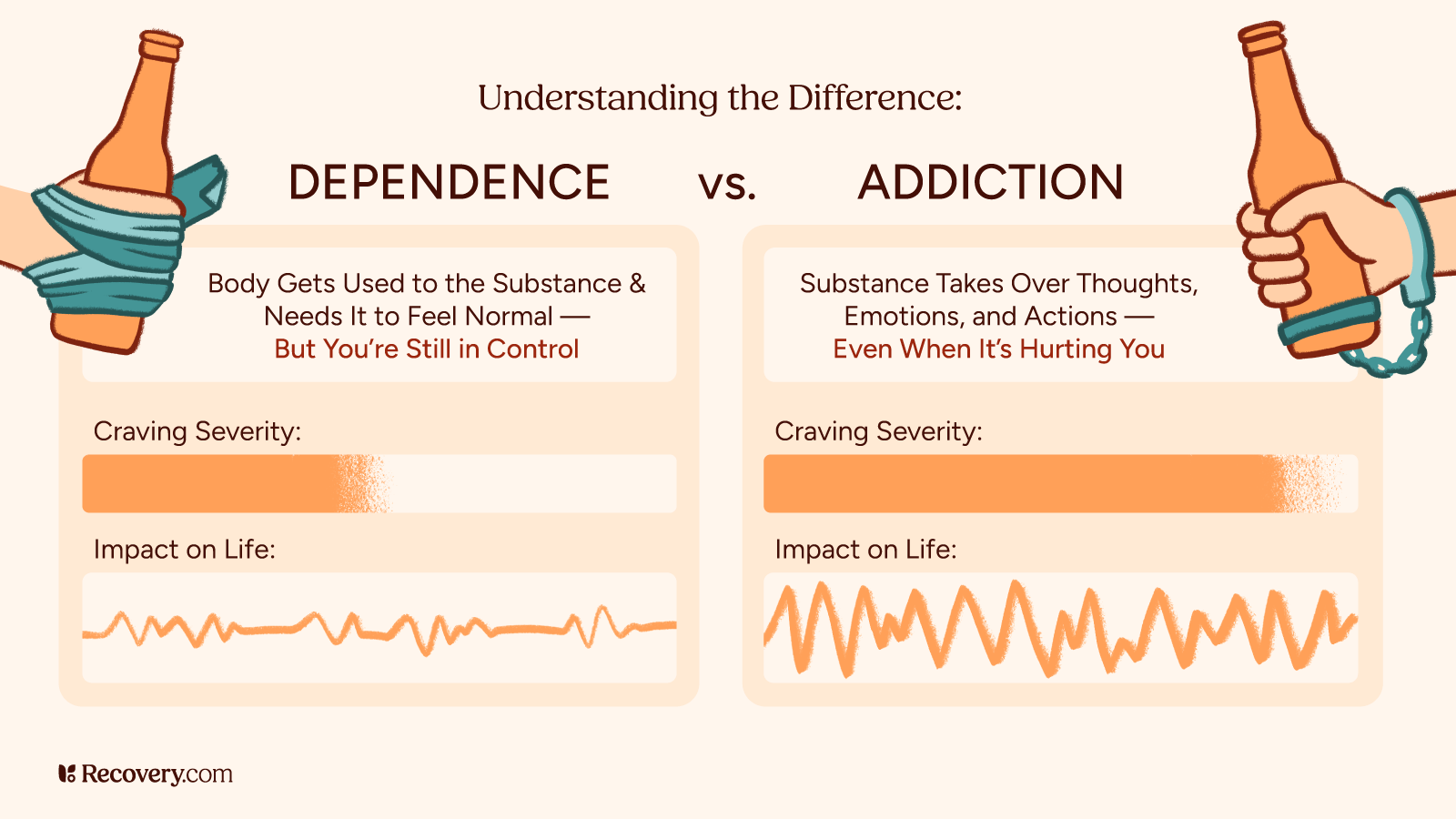
Dependency vs. Addiction
While dependency is mainly about your body’s physical reliance on kratom,10 addiction involves both physical dependency and behavioral changes. If you find yourself doing any of the following, it could be a sign that you’re developing a kratom addiction:
- Continuing to use kratom despite its negative effects on your life
- Spending a lot of time getting, taking, or recovering from kratom
- Neglecting responsibilities or missing out on important activities because of your kratom use
- Being unable to reduce or control your use of kratom
- Having strong cravings for kratom
Risk Factors for Kratom Dependency
Some factors that might make you more likely to develop dependency include:
- A history of substance abuse problems
- Using kratom to self-medicate mental health issues
- Starting to take larger doses of kratom or graduating to more highly concentrated extracts
- Taking kratom daily or throughout the day
- Using it for extended periods
- Combining it with other substances
Understanding the difference between casual use, dependency, and addiction helps you identify where you might be on this spectrum. If you notice signs of dependency or addiction, it may be time to reevaluate your relationship with kratom and start making some changes.
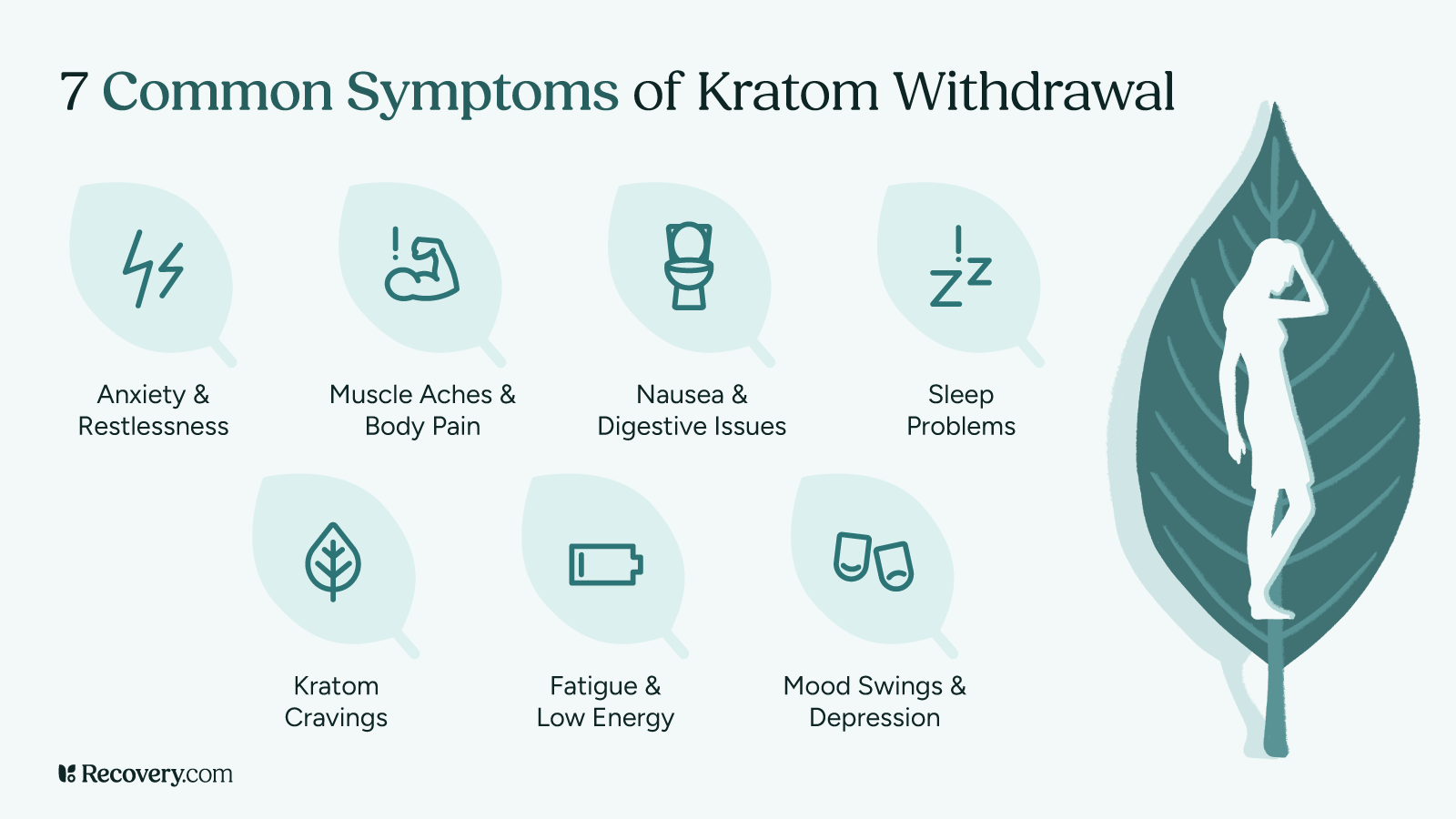
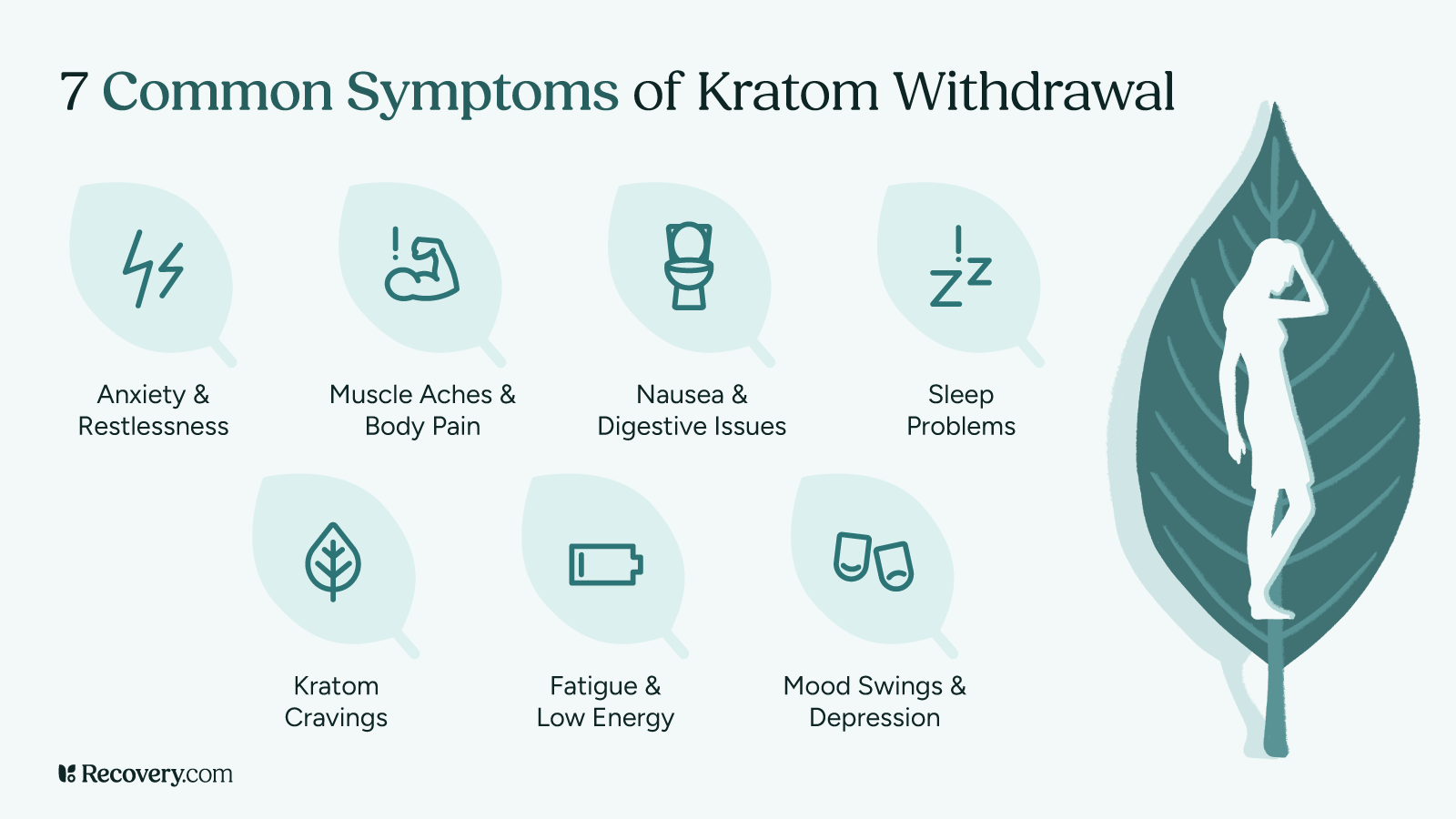
Kratom Withdrawal Symptoms
When you stop taking kratom after regular use, your body needs time to adjust to functioning without it. This adjustment period can bring on a range of uncomfortable symptoms that affect both your body and mind.
Physical Symptoms You Might Experience
Your body can react in several ways when you stop taking kratom:11
- Muscle aches and pains: Many people say they feel like they have the flu, with sore, achy muscles and joints. Moving around feels harder than usual.
- Nausea and stomach problems: Your digestive system often reacts strongly during withdrawal. You might feel queasy or sick to your stomach. Some people have vomiting, diarrhea, or loss of appetite.
- Sweating and chills: Your body’s temperature regulation can go a bit haywire. You might find yourself sweating heavily one moment and feeling cold the next. Night sweats are especially common.
- Runny nose and watery eyes: Just like with a cold, you might have a runny nose and eyes that tear up for no reason.
- Tremors or shaking: Some people notice their hands trembling or have full-body shakes during withdrawal.
- Headaches: These can be accompanied by sensitivity to light or sound.
- Fatigue and weakness: You might feel completely drained of energy, making even simple tasks feel exhausting.
Psychological Symptoms
There are also mental symptoms of kratom withdrawal:12
- Anxiety and restlessness: You may feel on edge, unable to relax, have racing thoughts, or feel a sense of worry that’s hard to shake.
- Mood swings: You might be on an emotional roller coaster, feeling irritable, angry, or sad for no clear reason.
- Depression: Some people have a persistent low mood, lack of motivation, or feelings of hopelessness during withdrawal.
- Cravings: You might find yourself thinking about kratom often and having strong urges to take it again.
- Brain fog: Many people report having difficulty focusing or thinking clearly during withdrawal.
A Closer Look at Kratom Withdrawal Insomnia
Sleep problems deserve special attention because they can make everything else feel worse. During kratom withdrawal, you might:
- Have trouble falling asleep, even though you’re exhausted
- Wake up throughout the night
- Have vivid, disturbing dreams
- Feel like you haven’t truly rested even after sleeping
Kratom withdrawal insomnia generally peaks during the first week but can linger for several weeks. Getting even small amounts of quality sleep can make a big difference in how you feel.
Sleep struggles during withdrawal? Learn more about managing withdrawal insomnia and get tips for better rest during recovery.
What Makes Withdrawal Better or Worse?
Several factors affect how intense your withdrawal symptoms will be:
- How much kratom you used: Generally, higher doses lead to more intense withdrawal.
- How long you’ve been using it: Longer-term use typically means more pronounced withdrawal.
- Your overall well-being: Being in good health otherwise can make withdrawal more manageable.
- Support system: Having people who understand what you’re going through can make a huge difference.
- Previous withdrawal experiences: If you’ve gone through withdrawal before, your body might react more strongly the next time (this is called the kindling effect).13
As you go through this process, it’s good to keep in mind that withdrawal symptoms are temporary. They’re your body’s way of healing and finding a new balance without kratom. While they are uncomfortable, they’re not dangerous for most people and will improve with time.
Kratom Withdrawal Timeline
If you’re planning to stop using kratom, having a roadmap of what to expect can help you prepare mentally. While everyone’s experience differs, most kratom users follow a somewhat predictable timeline of symptoms.
When Do Withdrawal Symptoms Start?
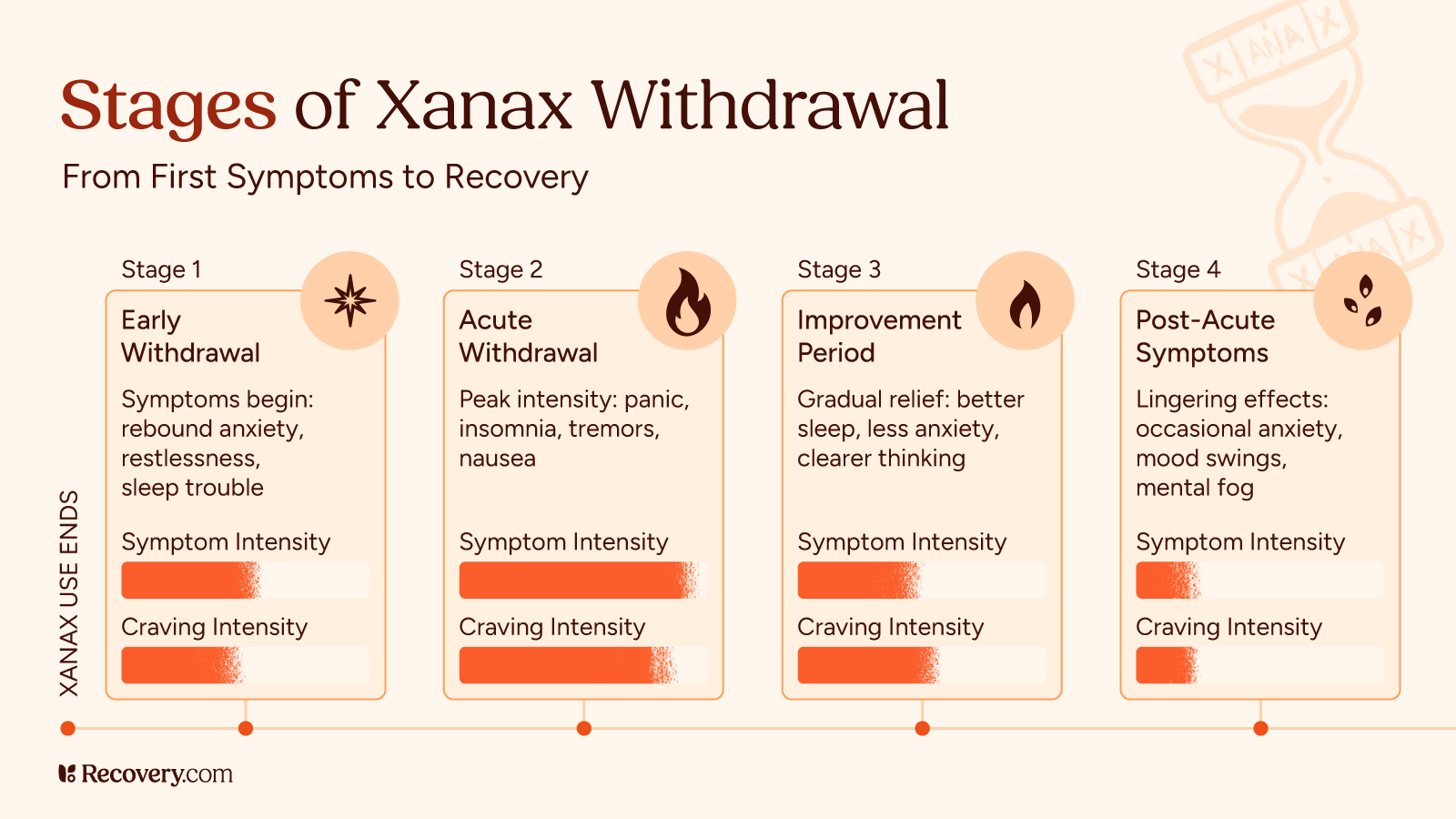
For most people, kratom withdrawal begins within 12-24 hours14 after your last dose. If you’ve been using very high doses or potent extracts, you might notice symptoms starting even sooner—sometimes within just 6 to 12 hours.
The onset often feels like a growing sense of discomfort, restlessness, or anxiety. You might notice minor physical symptoms like yawning, watery eyes, or a runny nose before more intense symptoms kick in.
Early Acute Phase (Days 1-3)
The first few days are typically the most challenging:
- Day 1: You’ll have anxiety, restlessness, and physical discomfort. Sleep might be difficult, and you may have strong cravings for kratom.
- Days 2-3: Physical symptoms usually intensify during this period. Muscle aches, sweating, nausea, and digestive issues peak. A lot of people describe this stage as feeling like a bad flu.
During this phase, remind yourself that what you’re experiencing is normal and temporary. The discomfort means your body is beginning to adjust to functioning without kratom.
Peak Symptoms (Days 2-5)
For most people, withdrawal symptoms reach their worst point somewhere between days 2 and 5. This is when the combination of physical discomfort and psychological symptoms can feel overwhelming.
The good news is that once you get through this peak period, your body starts to heal, and symptoms gradually become less intense. Many people find that reaching this turning point gives them the motivation to continue.
Subacute Phase (Days 6-14)
After the peak, you’ll enter the subacute phase:
- Most severe physical symptoms (like nausea, vomiting, and body aches) start to fade
- Sleep gradually improves, though it may still be disrupted
- Mood symptoms like anxiety and depression may linger
- Energy levels slowly begin to return
By the end of the second week, most people find that they’re functioning reasonably well, though not entirely back to normal.
Post-Acute Withdrawal Syndrome (PAWS)
Some people have lingering symptoms for weeks or even months after quitting substances. This is known as post-acute withdrawal syndrome,15 or PAWS. These symptoms are usually milder than acute withdrawal but can still affect your quality of life:
- Periodic mood swings
- Anxiety or depression that comes and goes
- Trouble with motivation or concentration
- Sleep disturbances
- Occasional cravings for kratom
PAWS symptoms typically come in waves: You might feel fine for several days, then have a few hard days before improving again. Each wave tends to be less intense than the one before.
Remember that healing isn’t a linear process. Having good and bad days during recovery is completely normal. With time, these waves become less frequent and less intense as your brain chemistry rebalances.
Are you having lingering symptoms after the initial withdrawal phase? Learn about post-acute withdrawal syndrome (PAWS) and how to manage these longer-term recovery challenges.
Managing Kratom Withdrawal at Home
Many people successfully navigate kratom withdrawal from the comfort of their own homes. With the right approach and preparation, you can make this challenging process more manageable.
1. Is Home Detox Right for You?
Home detox might be appropriate if:
- You’ve been using moderate amounts of kratom
- You don’t have other serious health conditions
- You have a support person who can check on you
- You don’t have a history of severe withdrawal
- You’re not using other substances like alcohol or opiates
However, home detox isn’t right for everyone. Your safety comes first. Here’s how to know when it’s time to seek professional help:
2. When to Seek Professional Help
Watch for these warning signs that indicate you may need medical support:
- Severe depression or thoughts of harming yourself
- Extreme dehydration from vomiting or diarrhea
- Racing heartbeat, chest pain, or difficulty breathing
- Seizures or hallucinations
- Inability to keep any food or water down for more than 24 hours
- Withdrawing from multiple substances at once
If you experience any of these, do not hesitate to reach out to a healthcare provider.
3. Tapering: A Gentler Approach
Instead of stopping kratom cold turkey, some people find that gradually reducing their dose helps minimize withdrawal symptoms. Here’s a simple tapering approach:
- Start by measuring your current daily amount accurately
- Reduce your total daily amount by about 10-15% every 2-3 days
- Space out your doses evenly throughout the day
- Go slower with reductions if withdrawal symptoms become too uncomfortable
- Keep a log to track your progress
Tapering off of kratom takes longer than quitting cold turkey, but it’s often much more comfortable. Be patient with yourself—a gradual taper over several weeks is typically easier on your body than a rapid one.
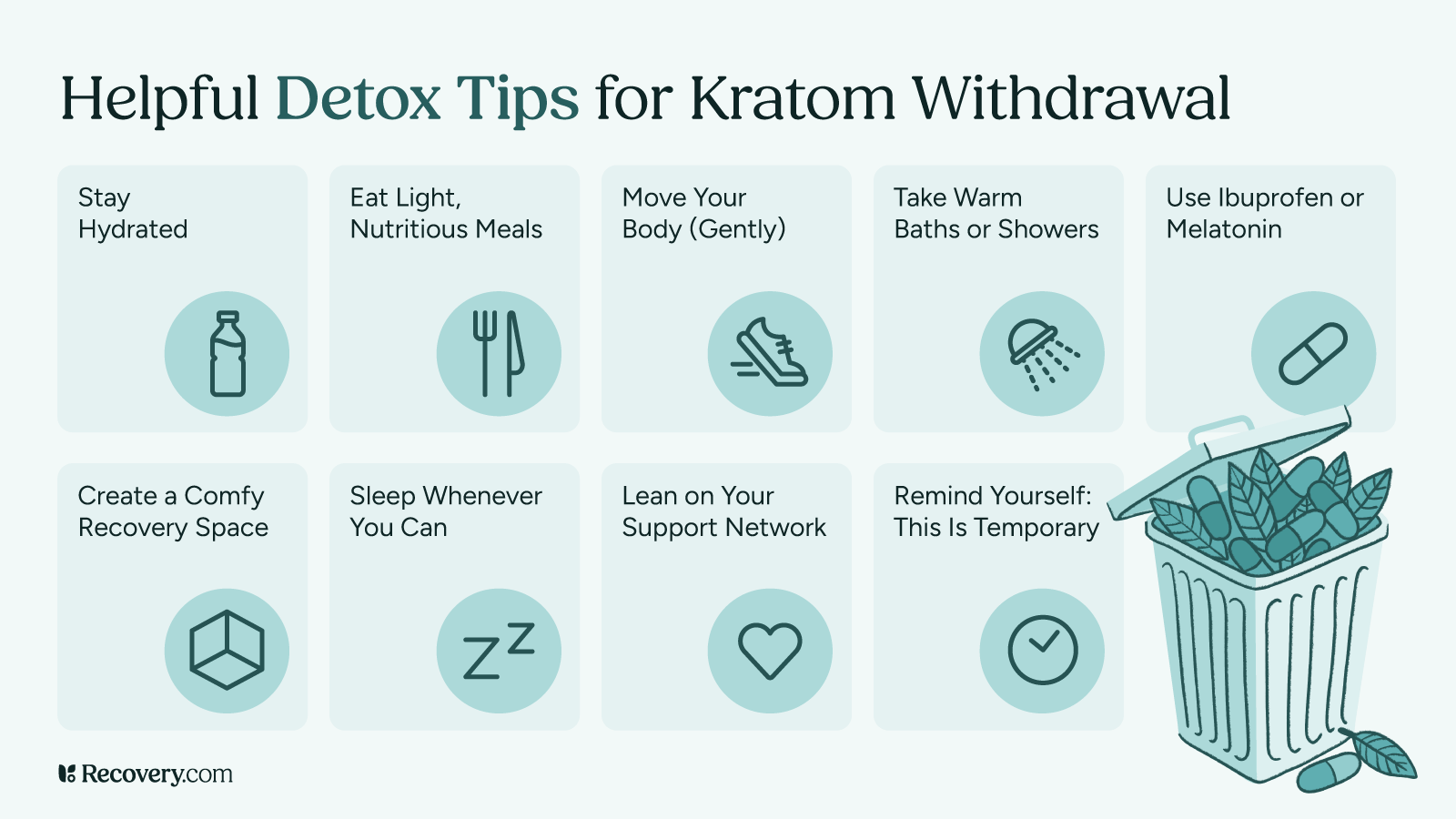
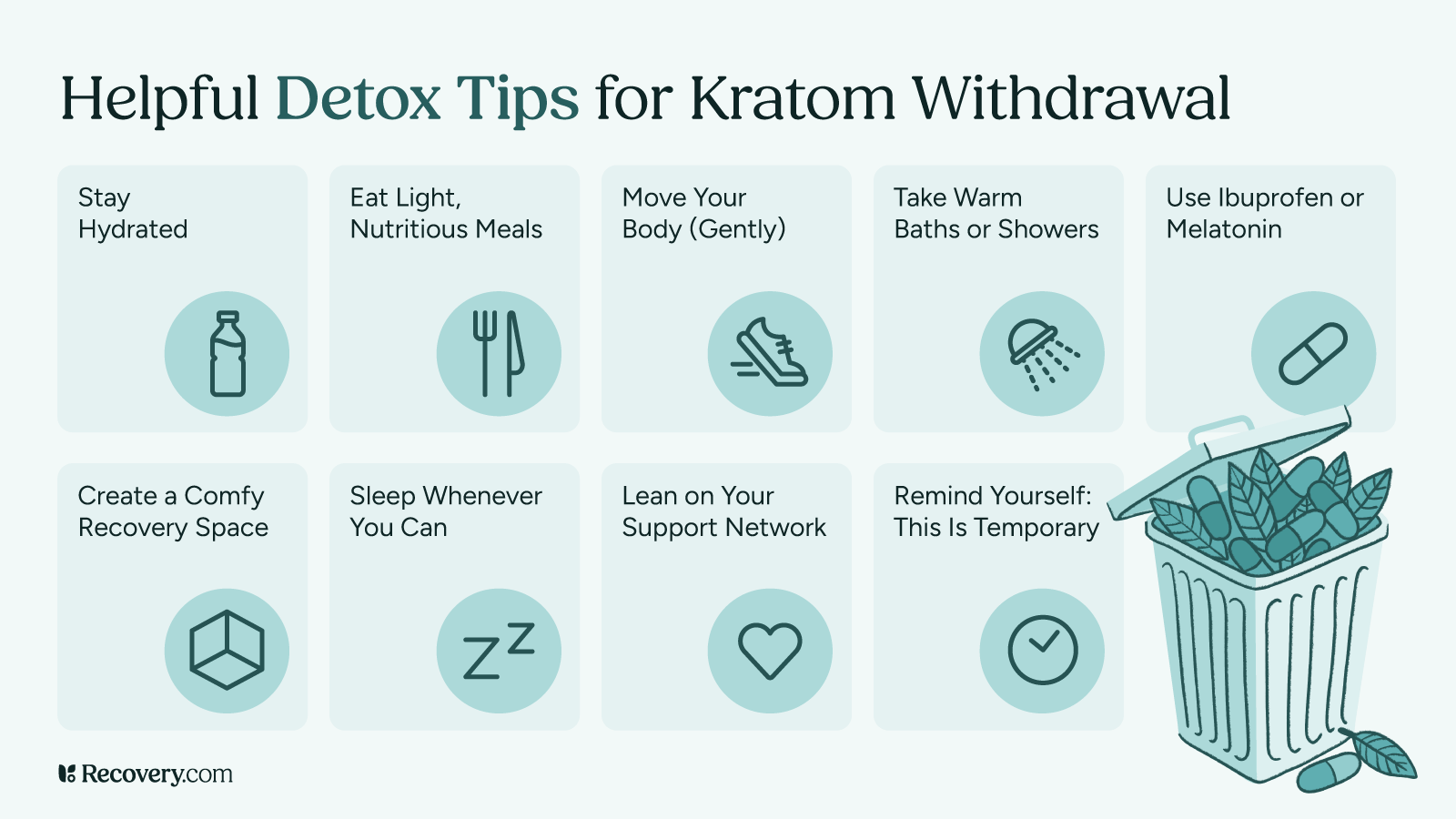
4. Self-Care Strategies That Help
These simple kratom withdrawal remedies16 can make a big difference in how you feel:
- Stay hydrated: Drink plenty of water and fluids to replace hydration lost through sweating or digestive issues.
- Nourish your body: Even if you don’t feel hungry, try to eat small, nutritious meals. Foods rich in magnesium (like nuts) and potassium (like bananas) may help with muscle cramps.
- Move your body (gently): Light exercise like walking or stretching can release natural endorphins that improve your mood and help with sleep.
- Warm showers or baths: The warmth can temporarily relieve muscle aches and help you relax.
- Create a comfortable recovery space: Clean sheets, comfortable clothes, and a quiet environment can help ease your mind.
5. Helpful Over-the-Counter Options
While these aren’t cures for withdrawal, they may help manage specific symptoms:
- For aches and pains: Non-prescription pain relievers like acetaminophen or ibuprofen (always follow package directions)
- For diarrhea: Over-the-counter anti-diarrheal products
- For nausea: Ginger tea, ginger candies, or motion sickness remedies
- For sleep: Melatonin, valerian root tea, or magnesium supplements before bedtime
*Note that these are general suggestions, not medical advice. Check with your doctor first if you’re unsure about taking any medication or supplement, especially if you have other health conditions or take prescription medications.
Professional Treatment Options
Sometimes, getting expert help makes the difference between struggling through withdrawal and finding a smoother path to recovery. Professional drug addiction treatment provides structure, medical supervision, and tools to address not just your kratom use, but also what led you to addiction in the first place.
6. Medical Detox Programs
Medical detox programs are safe settings where healthcare professionals monitor your withdrawal symptoms and provide relief. These programs typically last 3-7 days and focus on helping you get through the acute withdrawal phase comfortably. Because the discomfort of withdrawal causes many people to start using again, supervised detoxification can improve your chances of recovery success.
Other benefits of professional kratom detox include:
- 24/7 medical supervision
- Medications to ease specific symptoms
- Prevention of complications
- Emotional support during a challenging time
Many insurance plans cover detox services, especially if your provider determines it’s medically necessary.
7. Helpful Approaches in Treatment
Effective treatment programs typically include:
Medications: While there’s no FDA-approved medication specifically for kratom withdrawal, providers may prescribe medications to target specific symptoms, like clonidine for anxiety or trazodone for sleep problems.
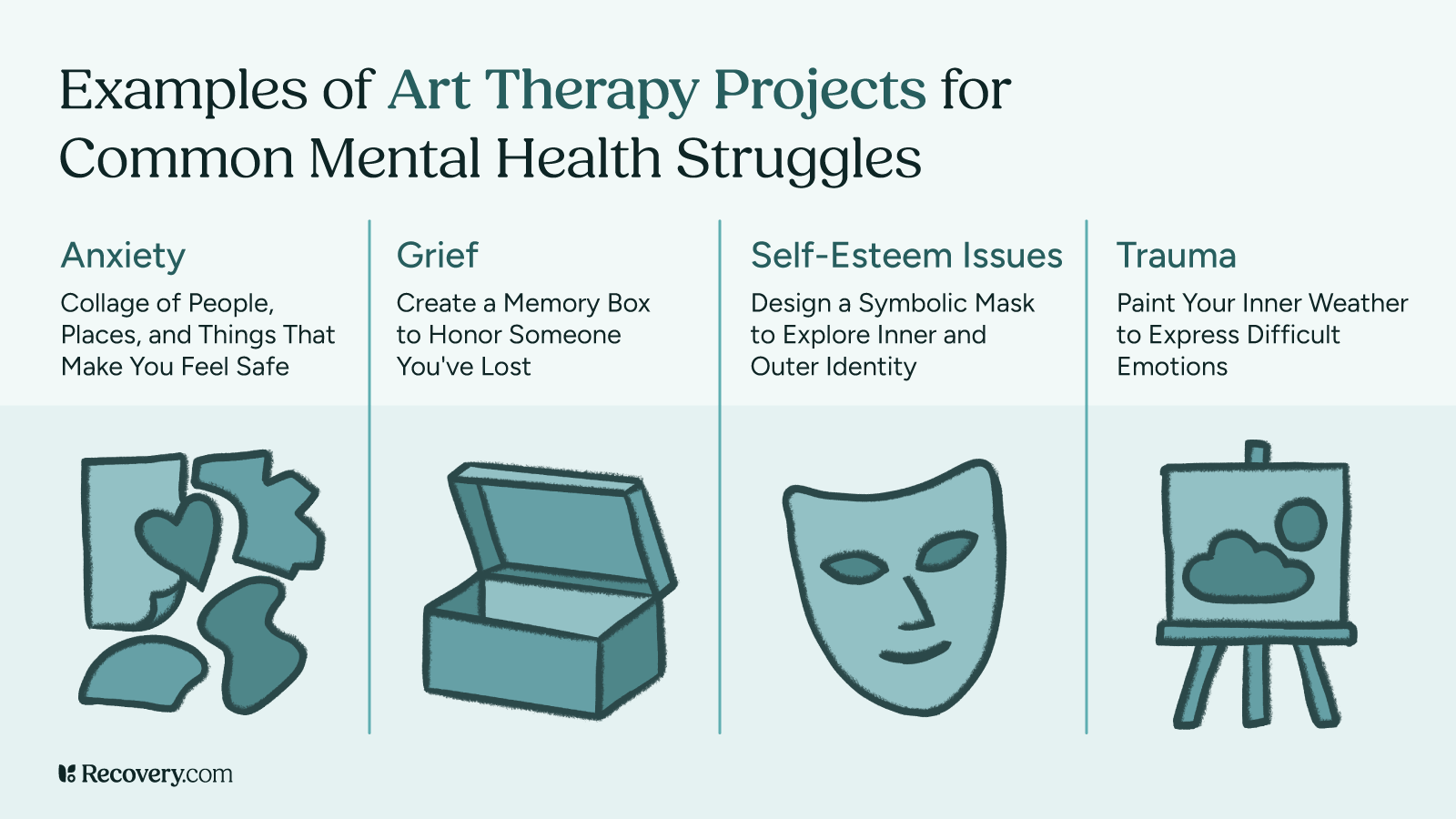
Talk therapy: Interventions like cognitive behavioral therapy (CBT) help you identify and change patterns that led to kratom use, plus develop healthier coping skills.
Group support: Connecting with others who understand what you’re going through can be incredibly healing. Many programs include group therapy or facilitate attendance at support groups.
Addressing co-occurring issues: If you’ve been using kratom to self-medicate anxiety, depression, pain, or trauma, treatment will include addressing these underlying concerns.
Discover effective ways to reclaim your life from pain through specialized rehab programs in our article on managing chronic pain.
Choosing Between Inpatient and Outpatient Care
After detox (or sometimes instead of it), you might consider:
Inpatient or residential rehab: You live at the facility for a set period, usually 28-90 days. This option provides the most structure and removes you from environments that might trigger kratom use.
Intensive outpatient programs (IOPs): You attend treatment several days a week for a few hours each day while living at home. This allows you to maintain work or family responsibilities while getting substantial support.
The right level of care depends on your specific situation, including the severity of your kratom use, your support system at home, and any other challenges you’re facing.
8. Building Long-Term Recovery Support
Recovery continues long after formal treatment ends. Many programs help you develop a continuing care plan that might include:
- Ongoing therapy sessions
- Support group meetings
- Wellness practices like meditation or exercise
- Regular check-ins with a recovery coach
- Medication management if needed
Remember that seeking professional help isn’t a sign of weakness—it’s a proactive commitment to your health. Many people who go through formal treatment of some kind find that the structure and support give them a helpful foundation to create lasting change.
Preventing Relapse
After you’ve gone through the challenge of kratom withdrawal, the next order of business is to stay kratom-free. Relapse prevention isn’t just about willpower —it’s about understanding your triggers and building healthy strategies to navigate life’s ups and downs.
Recognizing Your Personal Triggers
Most people have specific situations, feelings, or environments that make them want to use kratom again. Common triggers include:
- Stress and difficult emotions: Feeling overwhelmed, anxious, angry, or sad
- Physical discomfort or pain, especially if you used kratom for pain management
- Social situations: Being around others who use kratom or in places where you used it
- Boredom or lack of structure: Having too much unoccupied time
- Celebrating or rewarding yourself: Thinking “just this once” won’t hurt
Learning to identify your personal triggers is the first step in reducing your risk of relapse. When you notice a trigger, pause and remind yourself that the urge to use will pass, even if it feels intense in the moment.
Building Your Support Network
Recovery thrives in connection. Consider building support through these avenues:
- Friends and family: Let trusted loved ones know what you’re going through and how they can help
- Support groups: Consider SMART Recovery, Narcotics Anonymous (NA), or online forums focused on kratom recovery
- Behavioral health professionals: A therapist or counselor who understands substance use disorders
- Recovery apps: Many free apps offer tools for tracking your progress and connecting with others
Having people you can reach out to when cravings hit can make all the difference in preventing a momentary urge from becoming a relapse.
Practicing Healthy Coping Strategies
Life is hard at times and we need healthy ways of managing it! A large part of recovery is learning and practicing more helpful ways of dealing with challenges:
- Physical activity: Exercise naturally boosts your mood and energy levels
- Mindfulness practices: Meditation, deep breathing, or yoga can help manage stress
- Creative outlets: Music, art, writing, or other creative pursuits
- New hobbies: Activities that engage your mind and bring satisfaction
- Helping others: Volunteering or supporting someone else’s recovery
The more tools you have in your toolkit, the better equipped you’ll be to handle difficult times. The key is to get those resources in place before those moments arrive.
Building a Recovery-Friendly Lifestyle
Small daily habits can strengthen your recovery:
- Regular sleep schedule: Aim for 7-9 hours of quality sleep each night.
- Balanced nutrition: Eat regular meals that support brain and body health.
- Limit caffeine and sugar: These can mimic anxiety symptoms and trigger cravings.
- Practice self-compassion: Recovery isn’t perfect—learn from setbacks rather than beating yourself up.
- Celebrate milestones: Acknowledge your progress, whether it’s days, weeks, or months kratom-free.
Recovery is a process, not an event. Each day you make choices that support your health is a success, and even if you experience a setback, you haven’t lost the progress you’ve made.
Learn how proper nutrition can fuel your recovery journey in our article on nutrition for addiction and mental health healing.
Moving on From Kratom
Recovery from kratom dependency is a journey that takes time, patience, and sometimes a helping hand. While the withdrawal process has its challenges, remember that thousands of people have successfully navigated this path before you!
If you’re struggling with kratom addiction or withdrawal, you don’t have to go through it alone. Professional care can mean the difference between a difficult, uncertain recovery and one with proper guidance and support.
Treatment specialists understand what you’re going through and can help you with tools, medication, and strategies that significantly improve your chances of success.
Ready to take the next step? Search for a treatment provider today. Many treatment centers offer free, confidential assessments to help determine what level of care might be right for you. You’ll thank yourself for having the courage to ask for help when you needed it.
FAQs
Q: What is kratom addiction?
A: Kratom addiction occurs when regular use leads to dependence, causing physical or psychological cravings and withdrawal symptoms when not taken.
Q: How long do kratom withdrawals last?
A: Withdrawal symptoms typically begin within 6–12 hours after the last dose and can last from 3 to 10 days, depending on frequency and amount used.
Q: How long does kratom withdrawal insomnia last?
A: Insomnia during kratom withdrawal can last from a few days up to a week. Sleep patterns may gradually improve as the body adjusts.
Q: What are the withdrawal symptoms of Ketum?
A: Ketum (another name for kratom) withdrawal symptoms may include anxiety, irritability, muscle aches, insomnia, sweating, nausea, and cravings.
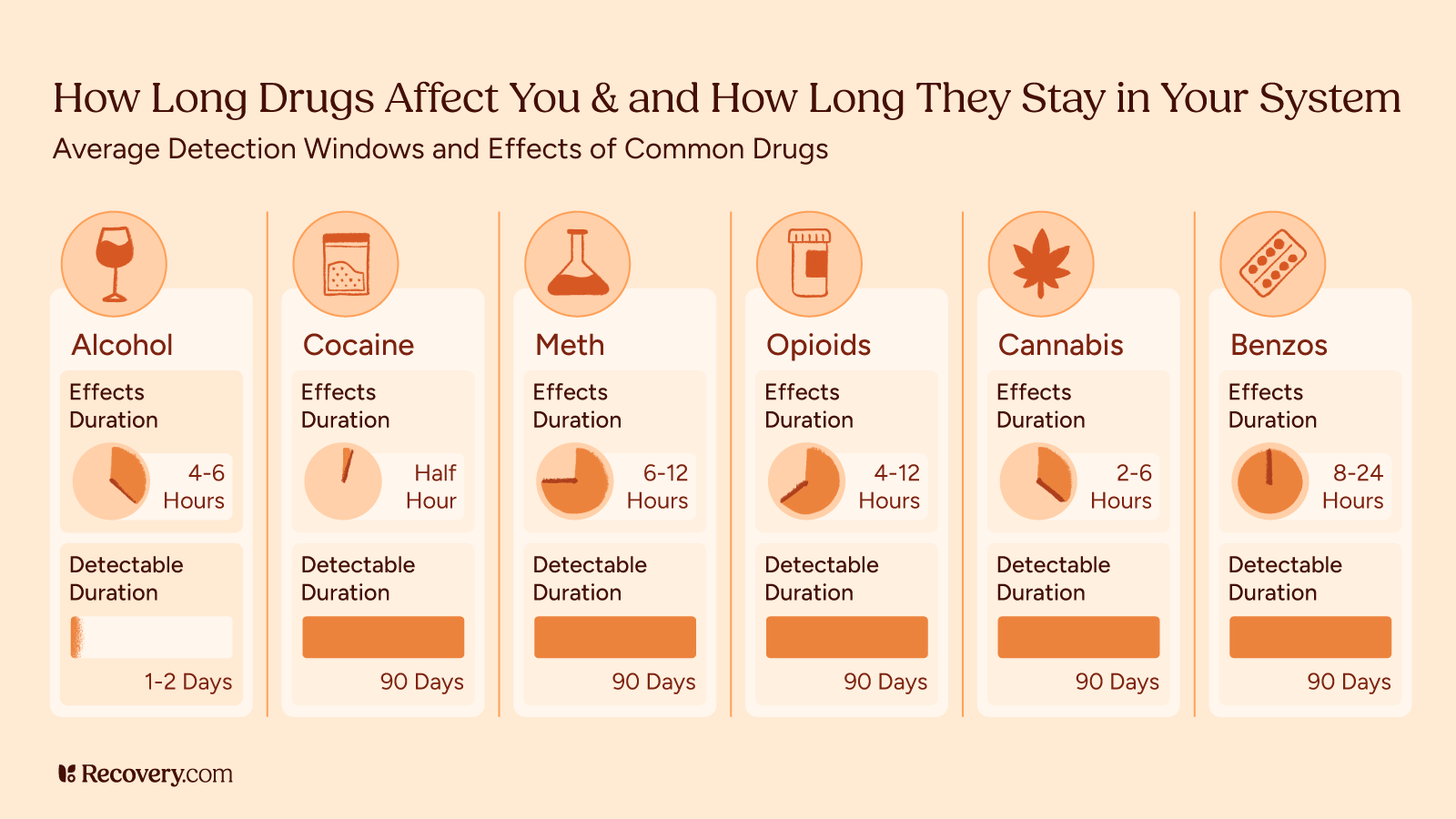
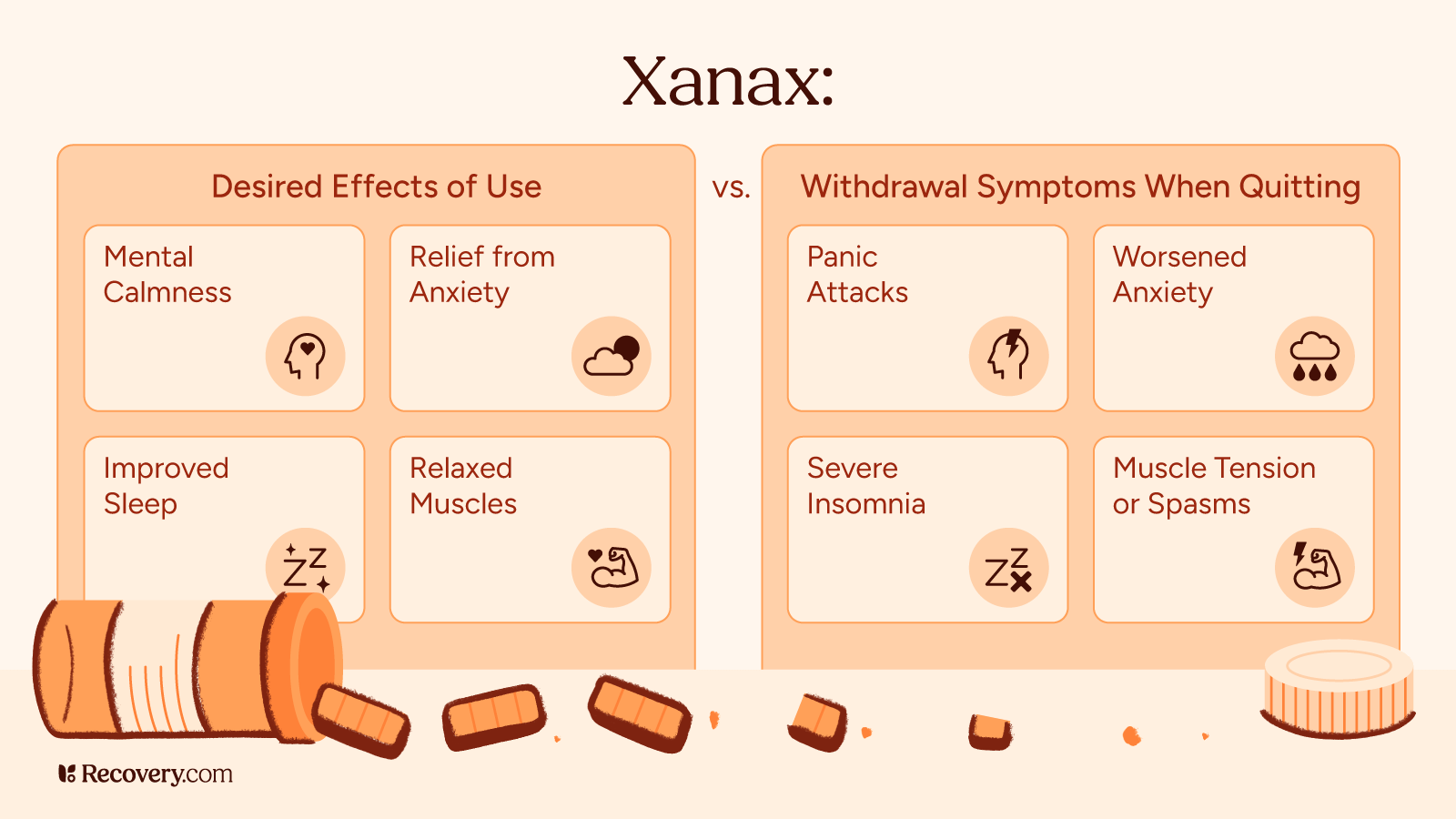
Q: What drug has the worst withdrawal symptoms?
A: Opioids, alcohol, and benzodiazepines are often considered to have the most severe withdrawal symptoms, sometimes requiring medical detox. Kratom withdrawal is usually milder but still uncomfortable.
Q: What are kratom withdrawal symptoms?
A: Common symptoms include anxiety, restlessness, muscle aches, insomnia, nausea, diarrhea, and emotional distress.
Q: Should I detox from kratom at home?
A: Detoxing at home may be possible for mild cases, but medical supervision is recommended if symptoms are severe or if there are co-occurring mental health conditions.
Q: Does kratom affect blood pressure?
A: Yes, kratom can affect blood pressure. It may cause either elevated or lowered blood pressure depending on dosage and individual response.
Q: What is kratom used for?
A: Kratom is often used for pain relief, mood enhancement, increased energy, and in some cases, self-management of opioid withdrawal—though it is not FDA-approved for medical use.
Q: Are you covered for addiction treatment?
A: Coverage depends on your health insurance provider and plan. Many policies include behavioral health services. Contact your insurer to confirm benefits for substance use treatment.
Q: How is kratom addiction treated?
A: Treatment may involve tapering off use, behavioral therapy, support groups, and in some cases, medications to manage symptoms or co-occurring conditions.
Q: What are effective ways to manage kratom withdrawal symptoms?
A: Staying hydrated, using over-the-counter medications for symptom relief, maintaining a sleep routine, and seeking counseling or medical support can help manage withdrawal.
Q: How can I manage kratom withdrawal symptoms effectively?
A: Similar to above—gradual tapering, professional support, proper nutrition, and self-care strategies can reduce discomfort during withdrawal.
Q: What are the stages of kratom withdrawal?
A: Withdrawal typically progresses through early symptoms (6–12 hours), peak discomfort (2–4 days), and gradual resolution (5–10 days), though timelines vary by individual.