Millions of people around the world struggle with substance use disorder: a widespread issue that affects individuals, families, and communities. This comprehensive guide to understanding substance use disorder (SUD) looks at its causes, symptoms, and the hopeful path to recovery.
What Is a Substance Use Disorder?
A substance use disorder (SUD) is a complex condition characterized by the uncontrolled use of a substance despite its harmful consequences. Here’s how the American Psychological Association defines it:1
Substance use disorder encompasses varying degrees of excessive use of a substance, including: alcohol; tobacco; opioids; caffeine; cannabis; hallucinogens; inhalants; sedative, hypnotics, or anxiolytics; stimulants (e.g., amphetamine, cocaine); and more.
It’s important to note that a substance use disorder is different from casual or moderate substance use. People with SUD often experience cravings, prioritize substance use over their responsibilities, and struggle to control their intake even when it causes obvious problems in their life.
SUD doesn’t just affect individuals—families and loved ones also suffer consequences including emotional distress, financial burden, and fractured relationships. Addiction takes a huge toll on communities at large, as the strain on healthcare systems and mental health affects our collective well-being.
Causes and Risk Factors
A variety of factors can lead someone to develop SUD:
Genetic Predisposition
People with a family history of addiction2 may be more likely to develop a substance use disorder themselves. That doesn’t mean it’s guaranteed, but it does suggest that some people’s genetic predisposition can make them more vulnerable. Certain genes, for example, affect brain chemistry in a way that influences how people respond to substances.
While genetics may be a factor, they aren’t your destiny. In fact, new research shows that neuroplasticity—your brain’s ability to change3—can be leveraged in the treatment of substance use disorders. Just as your brain “rewires” itself for addiction, it can also be rewired for recovery.
Learning that you’re more susceptible to addiction might seem scary, but it can be empowering. Being aware means you can take proactive steps to prevent it, like creating support systems and avoiding high-risk situations.
Environmental Influences
Environmental factors like childhood trauma, social pressures, and access to substances also play a role in developing SUDs.
Childhood trauma: “Adverse childhood experiences (ACEs) are widely recognized as predictors of early onset of alcohol and other drug use, problematic substance use, and addiction,” say researchers on adverse childhood experiences and addiction.4 That’s because “early exposure to abuse, neglect, and other stressors alters brain development, decreasing the individual’s ability and capacity to manage stress and emotions and increasing the likelihood of dependence on mood-altering substances.”
An adverse childhood experience, or ACE, is a traumatic experience that occurs in early life. Higher ACE scores are often linked to outcomes later in life, like addiction. To find out your score, take the ACE quiz here.
Peer pressure: In some social circles, using drugs and alcohol might be seen as cool, or a necessary part of fitting in. Being surrounded by friends who use substances normalizes this behavior and can make you feel like you have to use substances to be accepted.
Availability of substances: People with easy access to substances are more likely to try them for the first time, and to continue using them in times of stress or out of curiosity.
Access to positive outlets: Environments that lack recreational activities or other positive channels can increase the likelihood of turning to substances out of boredom or as a coping mechanism.
Psychological Factors
The relationship between mental health and substance abuse is often cyclical, as each condition feeds into the other. People struggling with mental health conditions like depression, anxiety, or trauma often turn to substances as a way to self-soothe when their emotions are too painful.
But while alcohol or drugs might offer a temporary escape, they ultimately make matters worse. Substance use disrupts brain chemistry, which worsens mental health disorders. Drug use itself can also create new mental health disorders,5 as “substance use and withdrawal from substances may lead to psychiatric syndromes or symptoms.”
Trauma, in particular, often triggers substance use. People who go through traumatic experiences are left feeling overwhelmed, isolated, and struggling to cope. Substances can become a way to dull their feelings and dissociate from painful memories. But substance abuse hinders the trauma healing process by arresting the development of real coping skills. True healing from trauma and other mental health conditions requires us to address their underlying causes.
Symptoms and Diagnosis
Substance use is often normalized, and substance abuse might not be obvious until its consequences become more serious. Here’s how SUD is detected and diagnosed:
Physical Symptoms
Substance abuse disorders cause a variety of physical symptoms:6
- Changes in appetite and sleep patterns
- Significant weight loss or gain
- Difficulty sleeping or excessive sleepiness
- Physical appearance: bloodshot eyes, tremors, or changes in skin health
Depending on the specific substance, other physical symptoms might arise. For example, opioid abuse causes constipation, while stimulant use causes rapid heartbeat and increased blood pressure.
It’s important to note that these symptoms can also be caused by other underlying conditions. However, their presence in combination with other behavioral changes can signal a problem that needs attention.
Behavioral Symptoms
SUDs also cause noticeable changes in behavior:
- Mood swings and irritability
- Lying about how much or how often you drink or do drugs
- Withdrawing and isolating from friends and family
- Stopping activities you once enjoyed
- Neglecting responsibilities like work, school, or household chores
- Declining performance or problems at work or school
- Financial or legal trouble
- Engaging in risky behaviors to get substances, or as a result of being intoxicated
Diagnostic Criteria
Healthcare professionals use an official manual called the Diagnostic and Statistical Manual of Mental Disorders, or DSM-5, to diagnose addiction and other mental health disorders. The DSM-5 criteria for substance use disorder7 focus on patterns of drug or alcohol use that cause impairment or distress:
- Using larger amounts of the substance or for a longer period than you intend to
- Repeated efforts to cut back or control substance use
- Spending a significant amount of time obtaining, using, or recovering from the effects of the substance
- Cravings or strong urges to use the substance
- Continued use despite causing problems in relationships, work, or school
- Neglecting important social or recreational activities due to substance use
- Using the substance in risky situations, like driving under the influence
- Continued use despite causing or worsening physical or mental health problems
- Tolerance: needing more of the substance to achieve the same effect
- Withdrawal symptoms when you try to stop or reduce use
The presence of several of these behaviors might indicate an SUD. For an accurate diagnosis, it’s important to obtain a professional substance abuse evaluation.
Treatment Options for Substance Abuse Disorder
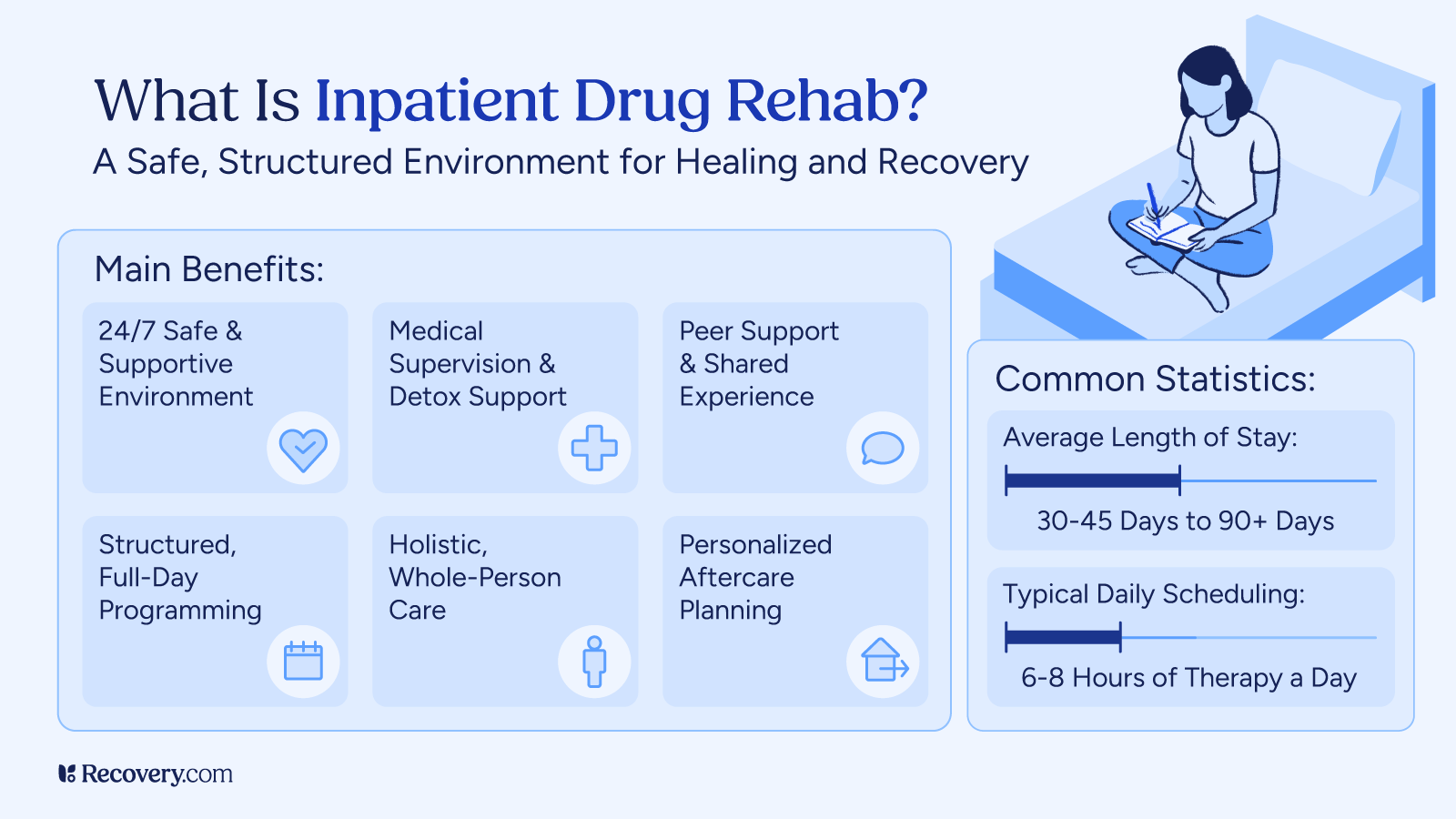
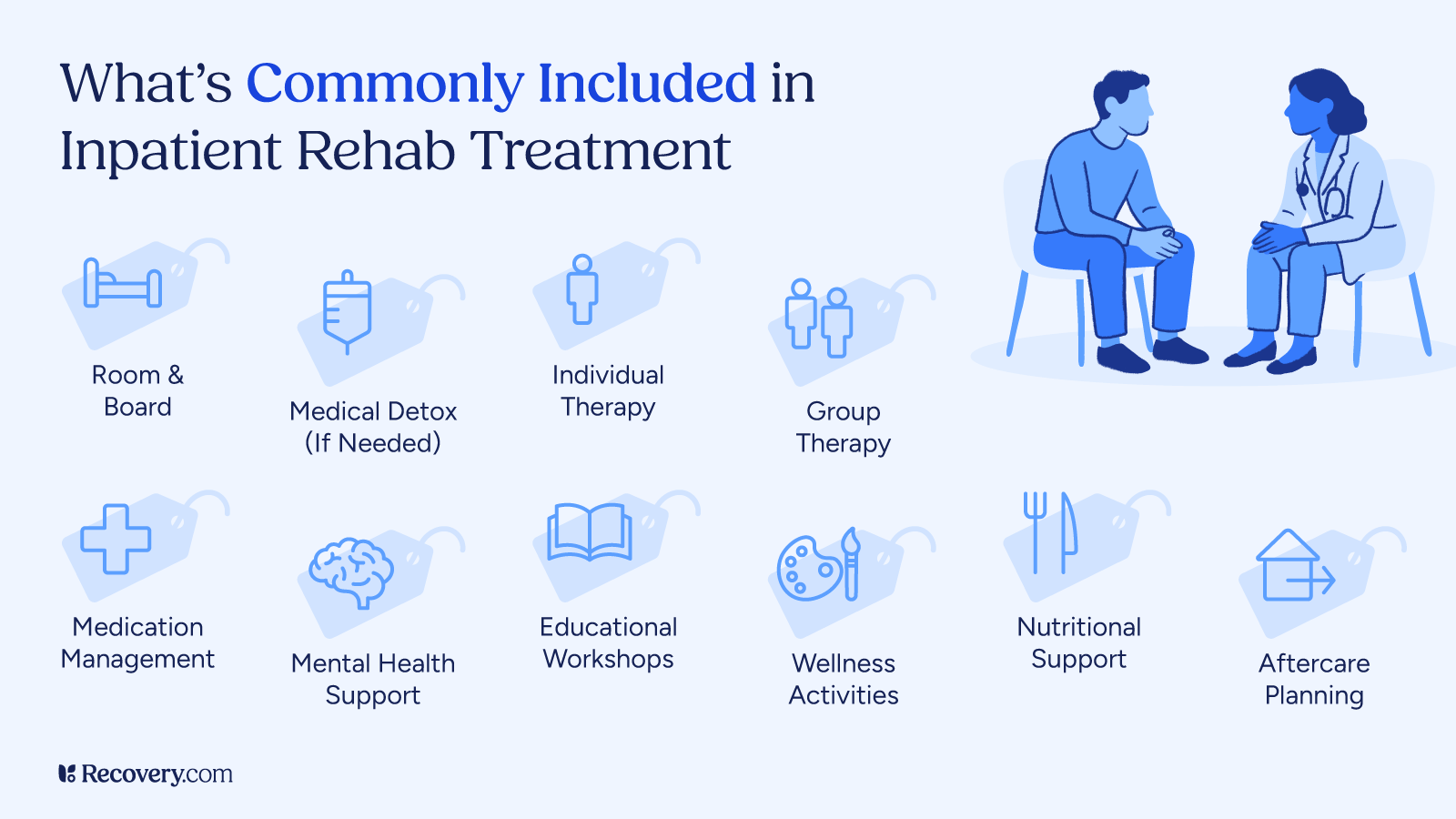
The continuum of care for treating SUD includes, but isn’t limited to:
Detox
For people who want to get sober but are physically dependent on substances, the first step is often medically supervised detox. This involves safely managing withdrawal symptoms, getting your body back in balance, and preparing for addiction treatment. Withdrawal symptoms can vary greatly, ranging from mild discomfort to life-threatening situations, depending on the amount and type of substance you used.
During detox, medical professionals closely monitor and manage your withdrawal symptoms in a safe, controlled environment. This might include providing medication to ease discomfort, ensuring proper hydration and nutrition, and offering emotional support. Depending on the facility, your detox program may also offer psychological counseling or help with transitioning into a residential addiction treatment program. Detoxing in a medically supervised environment helps prevent complications and ensures your safety during the withdrawal phase.
Detox is an important first step, but it’s only the beginning of treatment for substance abuse. After detox, attending a rehab with a comprehensive treatment plan can prepare you for a life in lasting recovery.
Therapy and Counseling
While detox treats the symptoms of substance abuse, to achieve lasting recovery, we need to treat its causes. That’s where therapy comes in. Addiction treatment programs use a wide range of therapies to treat substance use disorders, usually based on a treatment plan designed for your needs.
Cognitive behavioral therapy (CBT) helps patients identify and change negative thought patterns and behaviors that contribute to substance use. This can help you learn coping skills for managing triggers, or interrupt thoughts that normally cause you to use.
Dialectical behavior therapy (DBT) focuses on developing healthy emotional regulation skills. This can be especially helpful for people who tend to have very intense emotions that trigger substance use. DBT teaches skills like mindfulness and distress tolerance to deal with challenging feelings in a healthy way.
Family therapy teaches family members how addiction works and how best to support you, including boundary setting and healthy communication. Involving your family in your recovery can be a transformative experience. If you don’t have supportive relationships with your biological family, that’s okay—this also applies to chosen family.
Keep in mind that different therapeutic approaches work for different people. It may take more than one try to find one that’s a good fit for you.
Medication-Assisted Treatment (MAT)
Medication-assisted treatment (MAT) uses prescription medication to manage withdrawal symptoms and cravings. It’s most commonly used to treat dependency on highly physically addictive substances like opioids and alcohol. In MAT, medication is administered under the guidance of a qualified medical professional.
MAT works best in combination with behavioral therapies that address the mental health impacts of addiction. It’s not for everyone, but it makes recovery possible for many substance-dependent people.
Recovery and Management
Developing a Long-Term Management Plan
When you’ve spent years in addiction, recovery doesn’t happen overnight. A personalized, long-term management plan that tackles both the psychological and physical aspects of healing can set you up for success in recovery. This plan is a collaboration between you and your treatment team, and should evolve with you as you progress through your healing journey.
Psychological aspects of recovery are often addressed via various forms of talk therapy, which can take place in invidual or group settings. This helps you identify and address unresolved trauma and other driving forces behind your addiction. It also teaches practical skills for maintaining sobriety, like managing cravings, avoiding triggers, and regulating your emotions.
The physical aspects of recovery are equally important. Nutritional therapies help you restore your body to health after being depleted by substance use. Movement therapies and exercise promote mood-boosting endorphins and positive brain change. And improving your sleep hygiene ensures your body has time to rest and repair, setting you up for better mental well-being.
Relapse Prevention
Recovery from addiction is a marathon, not a sprint. Relapse is a real possibility—especially in early recovery—but you can take steps to minimize the risk. This starts with identifying triggers. These can be internal, like emotional stress, or external, like certain people, places, or situations. Once you’re able to recognize triggers, you can learn how to manage them.
Staying actively involved in support groups8 is another powerful relapse prevention strategy. Support groups are a safe space to connect with others who genuinely understand what you’re going through. Sharing experiences, offering encouragement, and holding each other accountable can help you stay strong and avoid the isolation that increases the risk of relapse.
If you do relapse, it doesn’t negate the progress you made. Think of it as a learning experience and an opportunity to recommit to recovery. With motivation and a strong support system, you can learn from setbacks and get back on track toward a substance-free life.
Support Systems
Managing substance abuse disorder is rarely a solo endeavor. A strong support system is a foundation for long-term success. This network can include family members, friends, and peer support groups.
- Family members can educate themselves about addiction, learn healthy ways of supporting, and communicate effectively to create an environment that’s conducive to healing.
- Friends who appreciate your challenges and celebrate your successes can make a world of difference. Having fun and spending quality time together is a vital and often overlooked aspect of recovery.
- Peer support groups like AA and NA are a great source of connection. Hearing the experiences of others who have walked a similar path and found success in recovery can inspire your own journey. These groups also have built-in systems for mentorship, accountability, and sober community.
Support is valuable in all its forms. These networks give us the strength to stay on track and build resilience as we traverse the ups and downs of recovery.
Overcoming Stigma
Substance abuse disorder is often shrouded in stigma, a negative perception that creates shame and discourages people from seeking help. This societal barrier has real consequences that affect access to treatment, support, and ultimately, recovery.
Thankfully, as mental health conversations are being held more openly, stigma is being reduced.9 But there’s still work to be done. Normalizing discussions about substance use disorder, increasing addiction education, and viewing people struggling with addiction as real, complex humans rather than 2-dimensional stereotypes all work to dismantle stigma.
Addiction is a disorder, not a moral failing. By holding open conversations, we can create a world where people struggling with SUD feel empowered to speak up, seek help, and access the resources they need. That means more people can openly lead fulfilling lives in long-term sobriety.
Recovery is a powerful healing experience that you deserve to feel proud of.
Resources and Help
If you’re concerned about your substance use, the good news is that there are plenty of resources available to help:
- SAMHSA’s National Helpline: The Substance Abuse and Mental Health Services Administration’s addiction resource hotline is available 24/7 at 1-800-662-HELP (4357). Trained specialists can provide confidential information and treatment referral services in English and Spanish.
- The National Institute on Drug Abuse (NIDA) offers research-based information on addiction, as well as links to reputable resources for finding treatment.
- Support groups: Peer support groups like Alcoholics Anonymous (AA), Al-Anon, and SMART Recovery offer free meetings, both in-person and online, for people struggling with addiction and their families.
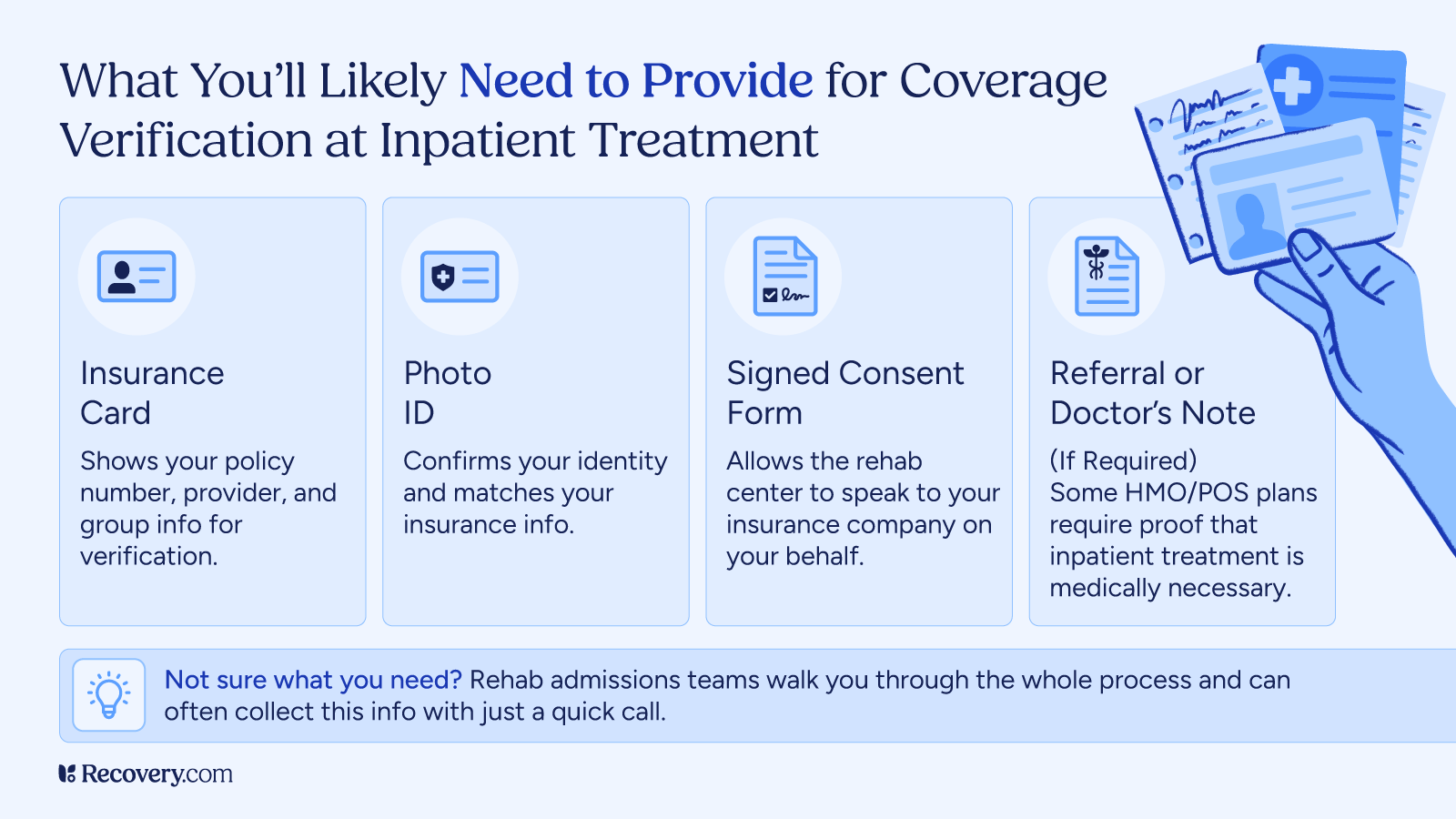
- Addiction treatment centers: Use an independent treatment finder or contact your insurance provider to find treatment centers in your area. Many treatment centers offer various programs, including inpatient and outpatient options, to meet individual needs.
Seeking help is a sign of strength. It’s the first step toward a new life that’s aligned with who you truly are.
Recovery Is a Path to Healing and Wholeness
Substance abuse disorder is a complex condition, but it is treatable. Understanding the causes, symptoms, and treatment options available can help you take the first steps toward recovery with confidence.
Search for addiction treatment centers by location, conditions treated, insurance accepted, and more, and speak to an admissions advisor directly today.