Addiction is often portrayed in media as a visibly destructive force, leading to immediate chaos and collapse. But for countless individuals and families, the reality is far more subtle, insidious, and heartbreaking. The life of a “high-functioning addict” can exist in a parallel world: one where they successfully run a business, raise a family, and maintain sobriety for years, all while wrestling in private with a relentless, life-threatening disease.
This devastating duality is at the core of the story shared by Adriana Sansam on the Recoverycast podcast. In 2023, she lost her 30-year-old husband, Eric, a devoted father and business owner, to an accidental overdose. Her journey through love, addiction, resilience, and agonizing grief reveals the urgent need to dismantle the stigma surrounding substance use disorder and to understand the immense pressure and isolation felt by both the person struggling and their closest loved ones.
1. The Love Story and the Unexpected Revelation
The beginning of Adriana and Eric’s relationship was a whirlwind of connection and certainty. They met as neighbors, and for Adriana, the attraction and sense of future were immediate. “We just knew,” she said. “When you know, you know.” Their life together moved fast, anchored by a deep mutual affection.
However, the foundation of their relationship was built before Adriana fully understood the hidden chapters of Eric’s past. As she recounted, her initial exposure to hard drugs and addiction was minimal, leading to a naive, movie-like perception of what an “addict” looked like. This perception was shattered one day while innocently rummaging through a desk with Eric.
The discovery of a needle in an old instrument case prompted a serious discussion that would forever change her life. Eric confessed: he was a recovering heroin addict. Adriana’s first reaction was to laugh—she genuinely thought he was joking, as it seemed so incongruous with the man she knew. Eric, however, was serious, explaining he had been in recovery for a year or two. He had already completed treatment and was sober, making the reality feel distant and manageable at first.
The early years of their relationship, while happy, were also a period of “white-knuckling sobriety” for Eric. He continued to drink heavily, a factor Adriana later realized was a significant, unaddressed trigger. For a recovering addict, alcohol can lower inhibitions and judgment, making the decision to use the original drug of choice feel less consequential. A powerful moment highlighted this danger: after a night of heavy drinking, Eric once turned to her and said, “I’m craving. I need to go home because I’m craving drugs. And don’t let me leave.” This was a terrifying first look at the relentless struggle beneath the surface of his successful facade.
2. The Internal Demons Driving the Disease
To truly understand Eric’s addiction, one must look into the deep-seated pain and trauma that fueled his struggle. Addiction is rarely about a simple lack of willpower; it’s often a complex response to unresolved psychological and emotional distress. As Adriana explains, Eric was a loving, empathetic person who felt things deeply—a common trait among those who grapple with internal demons.
Eric’s childhood was marked by immense loss and harmful influences. His father died the day before his fifth birthday, leaving a gaping wound. Compounding this, he endured a troubled relationship with a stepfather who was also an addict and who, tragically, introduced Eric to substance use. This environment of early trauma and exposure set a dangerous stage for his future.
The four and a half years of initial sobriety were a testament to Eric’s strength, but the underlying issues were never fully silenced. The relapse came in 2020, during the unique stress landscape of the COVID-19 pandemic. This period brought a convergence of stressors that can be exacerbating factors for addiction, including:
- Financial Pressure: Eric owned and operated a moving company, which was severely impacted by COVID-related lockdowns and restrictions. He felt the intense pressure of being the sole provider for his growing family.
- Mental Health Struggles: The pandemic was a global mental health crisis. For Eric, the isolation, uncertainty, and disruption to routines were a perfect storm.
- Family Stress: Adriana was battling severe postpartum depression following the birth of their first daughter and was pregnant with their second child. This stress, while shared, weighed heavily on Eric, contributing to his feelings of inadequacy and failure.
This perfect storm culminated in Eric’s relapse while Adriana was away. The disease, which had been dormant, reasserted its presence, preying on his mental and emotional vulnerabilities.
3. Recognizing the Mask: Signs of a High-Functioning Addict
When Adriana returned from her trip, she noticed subtle differences in Eric’s behavior, though she didn’t connect them to drug use initially. The relapse of a high-functioning addict is often not signaled by a sudden dramatic breakdown, but by small, almost imperceptible shifts. Eventually, Adriana discovered heroin in his car—a devastating find that Eric initially tried to deny, but confessed to upon seeing her attempt to dispose of it.
For loved ones of high-functioning individuals, recognizing the signs can be incredibly difficult because the core responsibilities of life are still being met. Eric successfully hid his addiction from even his closest family members, including Adriana’s parents, whom he lived with for a year and a half.
Tell-Tale Signs of Hidden Addiction:
- Excessive Time Away from Home: Eric’s work trips became longer, and he invented reasons to be out for extended periods. This distance provided an opportunity to use away from his family.
- Increased Frequency of Normal Trips: Eric became “a gas station guy,” multiplying his short trips out. Adriana later realized this was a cover for when he would go get high.
- Sudden “Sweetness” or Over-Compensation: Eric began offering to go out and get Adriana her favorite coffee, a gesture that seemed loving but was actually a mechanism to get her to let him leave the house. “I didn’t catch on until later is, oh, you wanna get me a coffee so you can go get high?”
- Emotional Withdrawal and Embarrassment: He would isolate himself while using, often going to work to get high. As Adriana noted, this was out of embarrassment—an attempt to shield his family from witnessing his struggle.
This ability to manage a business and maintain the facade of a “really good husband, really good father” is what makes high-functioning addiction so frighteningly dangerous. It allows the disease to progress out of sight until it’s too late.
4. The Unconventional Path to Support: ‘I’m Not Against You’
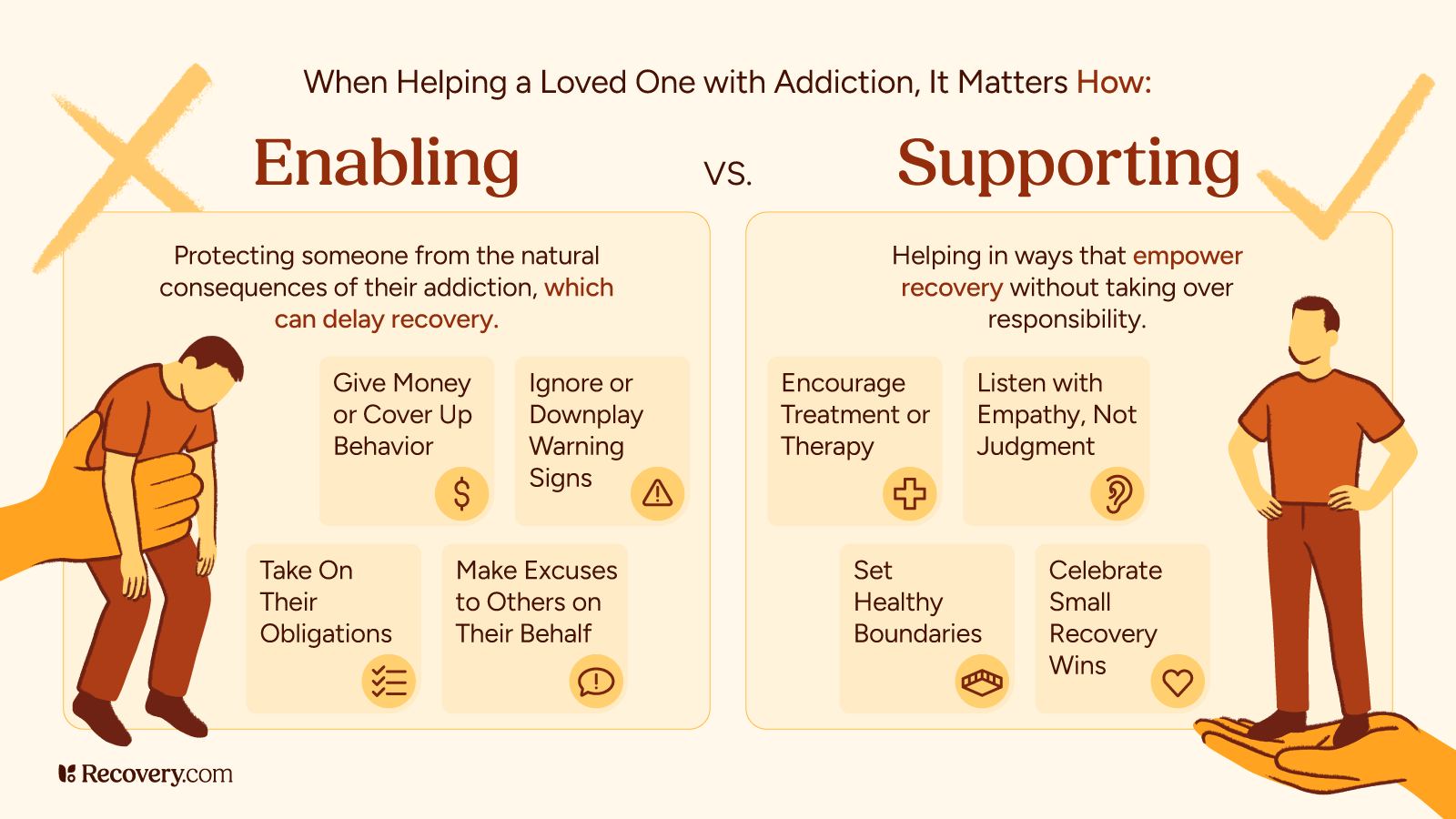
When faced with Eric’s relapse, Adriana’s initial reaction was pain and confusion: “Why are you doing this to me? Why do you hate me?” This mindset is common for partners, stemming from the deeply ingrained belief that love should be enough to overcome the addiction.
However, as she researched and talked openly with Eric, her perspective shifted from one of personal offense to one of team-based support. Eric played a crucial role in this transition, helping her understand that his actions were not a malicious choice against her, but a symptom of his disease.
The shift in their approach was profound:
- Disappointment vs. Abandonment: Adriana learned to separate her disappointment in the relapse from her commitment to Eric. She was honest about her anger but firm in her stance: “I am on your team.”
- The Power of Staying: Eric often told Adriana to leave him, believing she deserved better, but she consistently refused. Her unwavering presence became a lifeline. Addiction often pushes people away out of shame and a desire to protect loved ones from the inevitable pain. Her refusal to be pushed away countered his deep-seated trauma.
- The Desire for Help: Unlike many who fight the idea of sobriety, Eric always wanted to be clean. He would often call Adriana in distress immediately after using, begging her to come home and throw away his stash for him because he lacked the willpower to do it himself. This shows the addict’s true desire fighting against the compulsion of the disease.
Adriana’s “crazy” actions—the constant checking, location sharing, and accountability—were born out of love and fear, not malice. They were a form of survival. Eric himself later validated her vigilance: “If you weren’t as crazy as you were, I would’ve been dead a very long time ago.”
This validation was essential, highlighting that for a high-functioning addict, extreme accountability from a loved one can sometimes be the only thing keeping them tethered to life.
5. The Isolation of Shame and Stigma
Perhaps the most tragic aspect of their journey was the profound isolation Adriana endured. For years, she kept Eric’s addiction a complete secret from her family, friends, and community. This silence was driven by Eric’s fear of judgment and the pervasive stigma attached to substance use disorder.
This wall of secrecy forced Adriana into “survival mode,” making her feel like a “crazy wife” to the outside world because they couldn’t see the real threat she was fighting. The emotional burden of monitoring, fearing, and keeping silent while living with two small children took a severe toll on her mental health.
The silence broke devastatingly on the day Eric died. In her frantic call to the hotel, yelling that her husband was an addict and needed help, her parents finally heard the truth. This moment underscores a horrifying reality: stigma kills. The fear of being judged prevented Eric from seeking consistent, community-based support, and it prevented Adriana from accessing her own support network, such as Al-Anon, which provides crucial resources for the family members of addicts.
6. The Inevitable Tragedy and the Ongoing Fight Against Stigma
Eric’s death occurred on a work trip in March 2023. Though he was not in a period of active, sustained addiction at the time—Adriana had been drug-testing him and could tell by his behavior—the nature of his death pointed back to the disease. For Eric, the work trips were a time away from accountability, and tragically, a moment of isolation was a moment of vulnerability.
His death revealed a further layer of societal judgment. When Adriana shares how her husband died, she is often met with instant judgment from those who view addiction through the narrow, stereotyped lens of popular culture. They cannot reconcile the image of a loving father and successful businessman with an accidental overdose.
This experience highlights the critical need to view addiction as a chronic disease, not a moral failing. The countless thousands of accidental overdoses are not happening to “nobodies”—they are happening to people like Eric: neighbors, fathers, business owners, and loving partners. This is why conversations like Adriana’s are vital. They humanize the disease and fight the pervasive stigma that keeps people silent and isolated, often with fatal consequences.
7. Finding Hope and Voice: Moving Just for Today
Adriana’s resilience in the face of this incomprehensible loss is a testament to her strength. She now channels her experience into her podcast, Just for Today, a phrase she found in Eric’s recovery journal. It is a philosophy that embraces the idea of coping with the immense weight of grief and the past by focusing only on the present moment.
For those struggling with addiction or supporting a loved one, Adriana’s story offers crucial lessons:
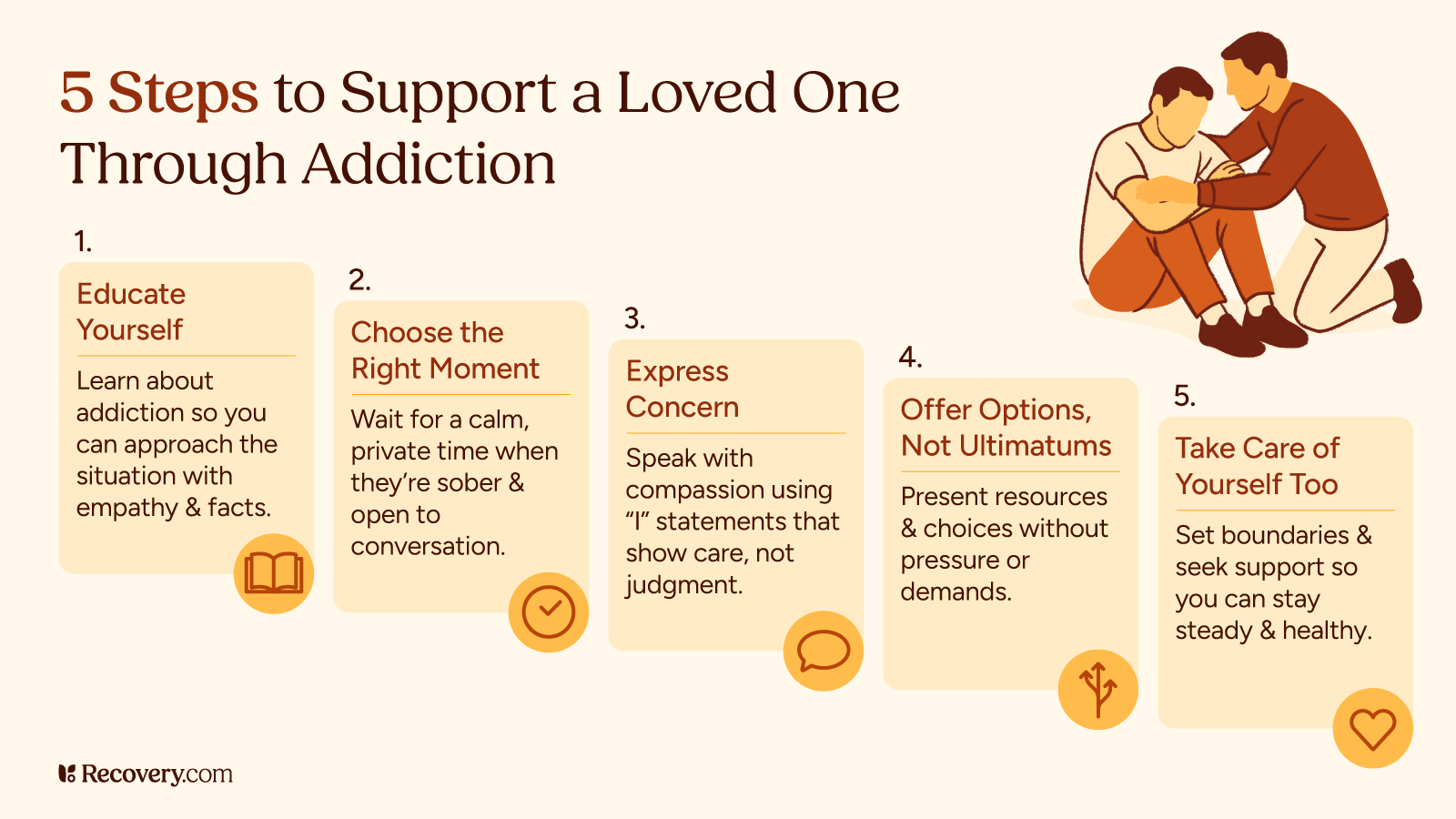
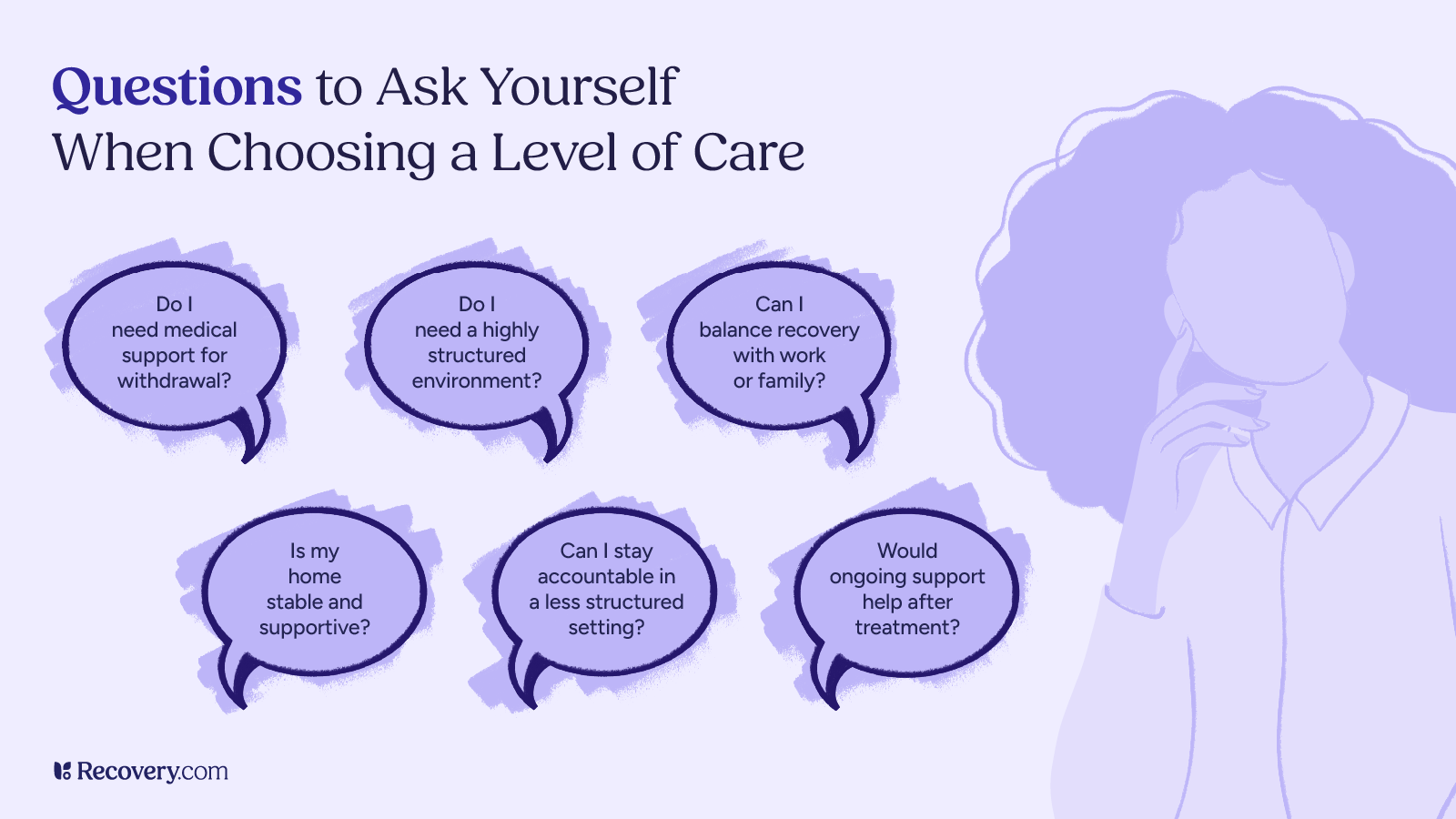
- Acknowledge the Disease: Recognize that addiction is a chronic, relapsing disease, not a lack of love or moral character. This shift in perspective is the first step toward effective support and reducing your own feelings of disappointment or guilt.
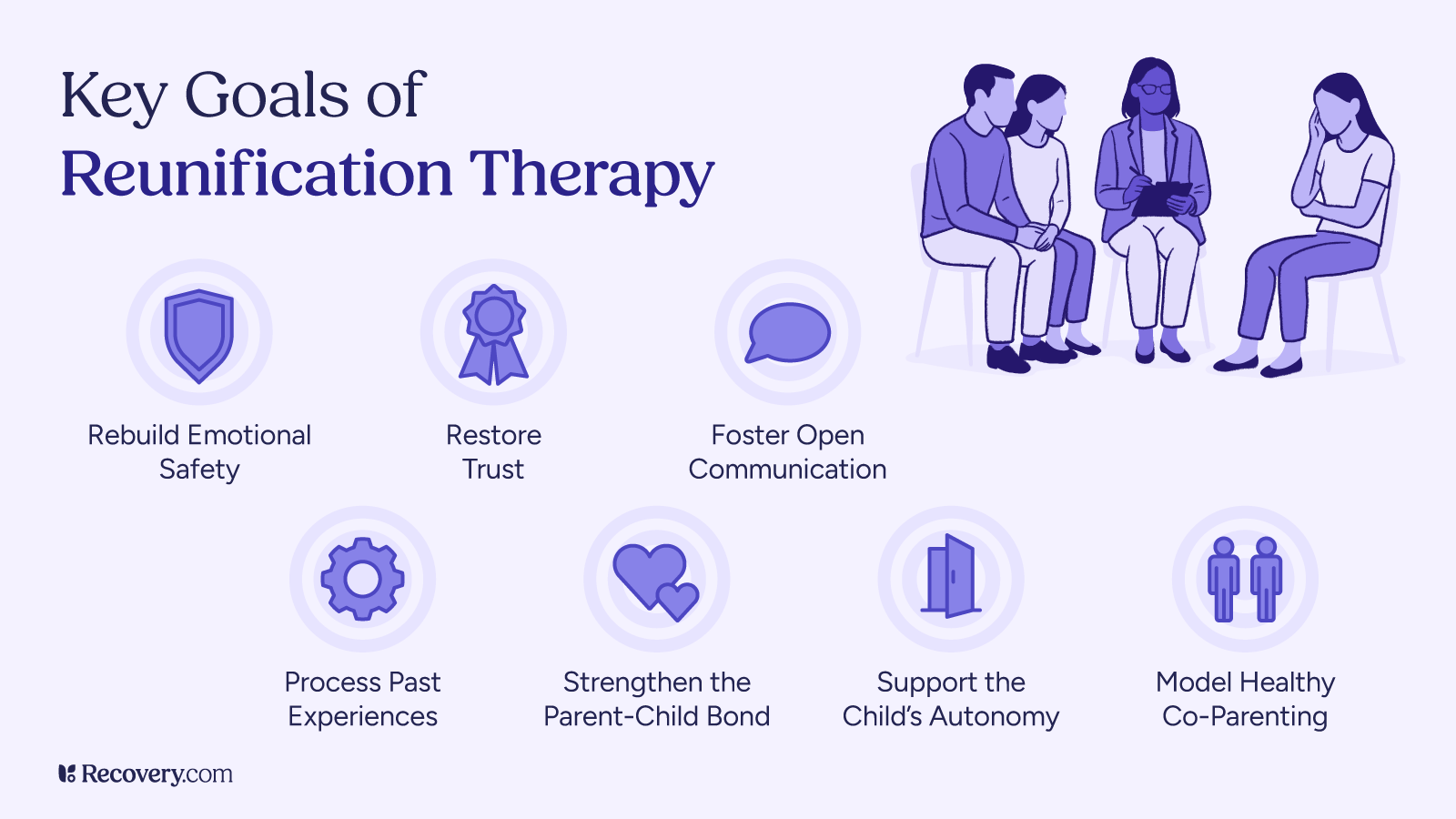
- Seek Your Own Support: Family and friends need support just as much as the person using. Organizations like Al-Anon or individual therapy can help loved ones process their grief, fear, and anger. Resources for families can be found at Recovery.com’s resource center.
- Embrace Accountability (With Love): For high-functioning individuals, a strong support system that provides consistent, non-judgmental accountability can be life-saving.
- Talk About It: Break the cycle of secrecy. Sharing Eric’s story is Adriana’s way of ensuring his life—and his struggle—serves a greater purpose: saving others by normalizing the conversation.
Eric’s life, filled with love, success, and profound internal pain, is a powerful reminder that addiction wears many masks. By confronting the stigma head-on and understanding the complex reality of the high-functioning addict, we can better support those who are struggling just for today and perhaps prevent future tragedies.