Deciding to quit marijuana can be a significant and life-changing decision. Whether you’re doing it for your mental clarity, physical health, or personal growth, the detox process can be challenging—but you’re not alone.
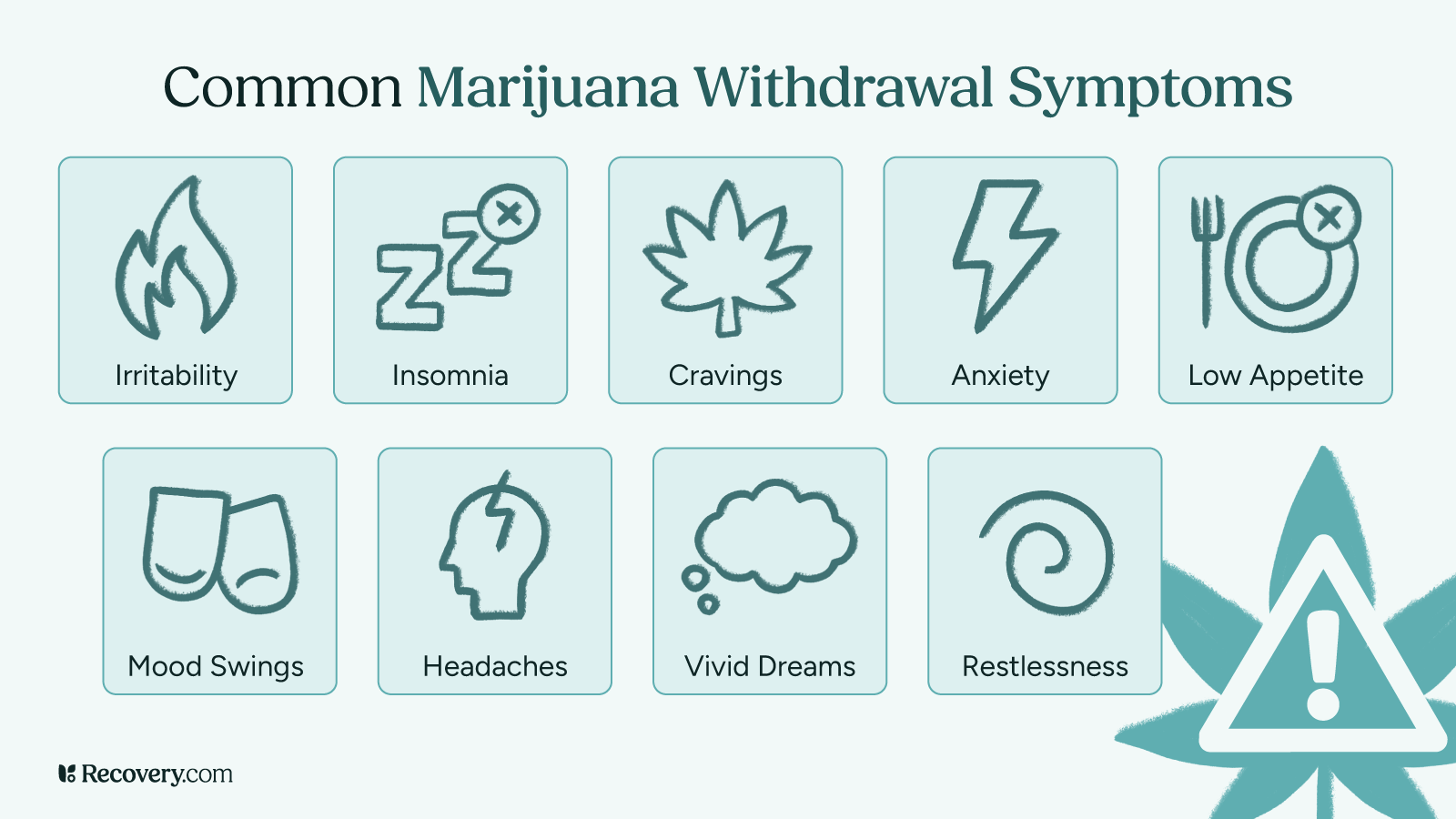
Marijuana withdrawal symptoms like irritability, insomnia, and cravings can make quitting difficult, but understanding how THC affects your body and learning about natural detox strategies can help you take control of your recovery.
What is Marijuana Detox?
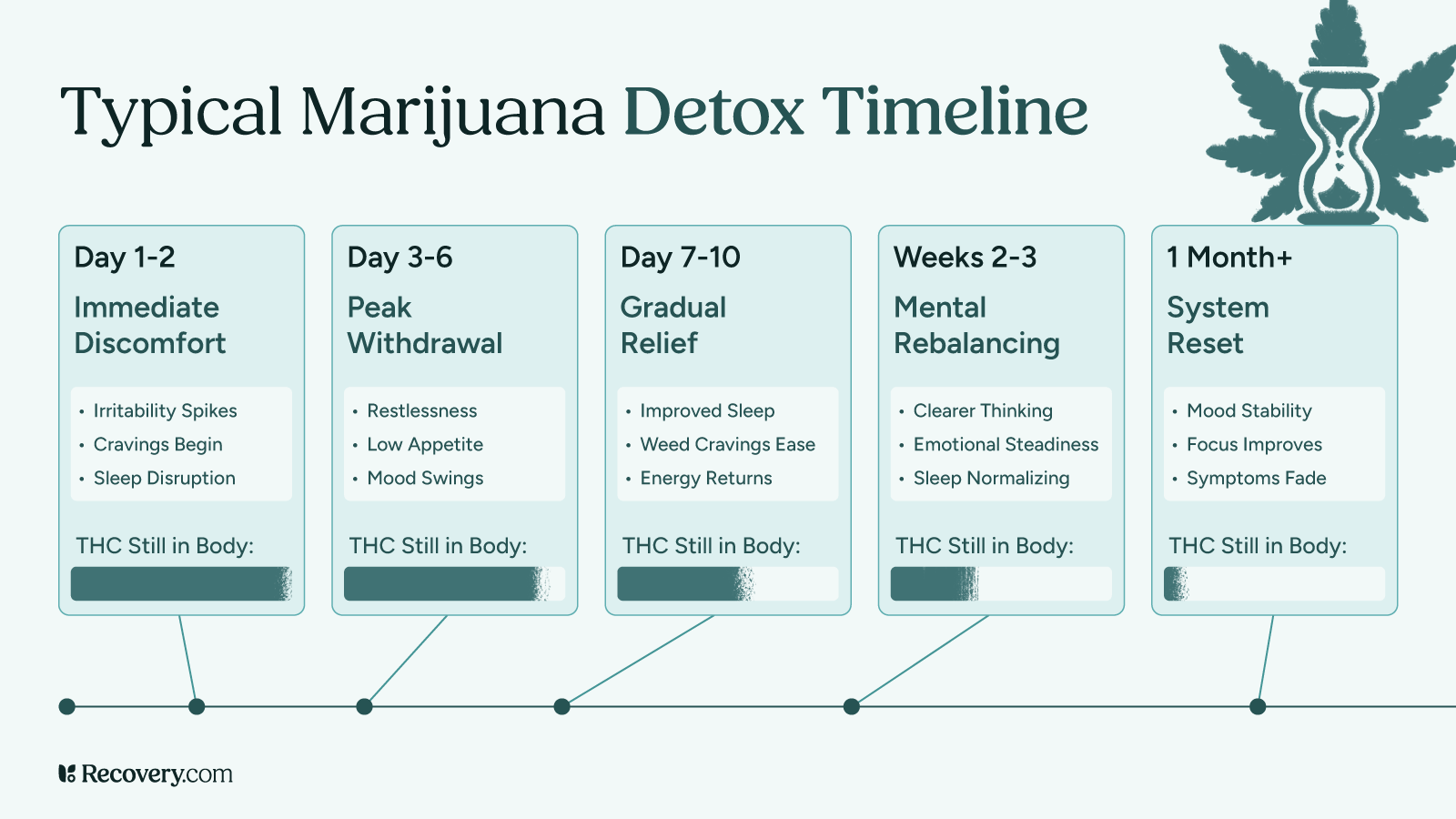
Detoxing from marijuana isn’t always as simple as stopping. Withdrawal symptoms can begin within 24-48 hours after the last use and may last up to two weeks. Imagine finally deciding to quit, only to find yourself wide awake at 3 AM, sweating and restless.1 Or feeling on edge all day, snapping at loved ones for no reason. Detoxing is a process, and it requires patience, self-compassion, support, and a solid plan. You can have compassion for yourself and your experience and know that this is a common experience for many people.2
Common Withdrawal Symptoms:
- Irritability and mood swings
- Anxiety and depression
- Insomnia3 and vivid dreams
- Decreased appetite
- Headaches and nausea
These withdrawal symptoms can range from uncomfortable to clinically significant. Despite the challenge of withdrawal, THC can successfully clear from the body, and you can feel good again without feeling like you have to use cannabis to feel “normal” or okay.
The following 6 strategies can help with natural marijuana detox and help you understand what to expect.
1. Hydration
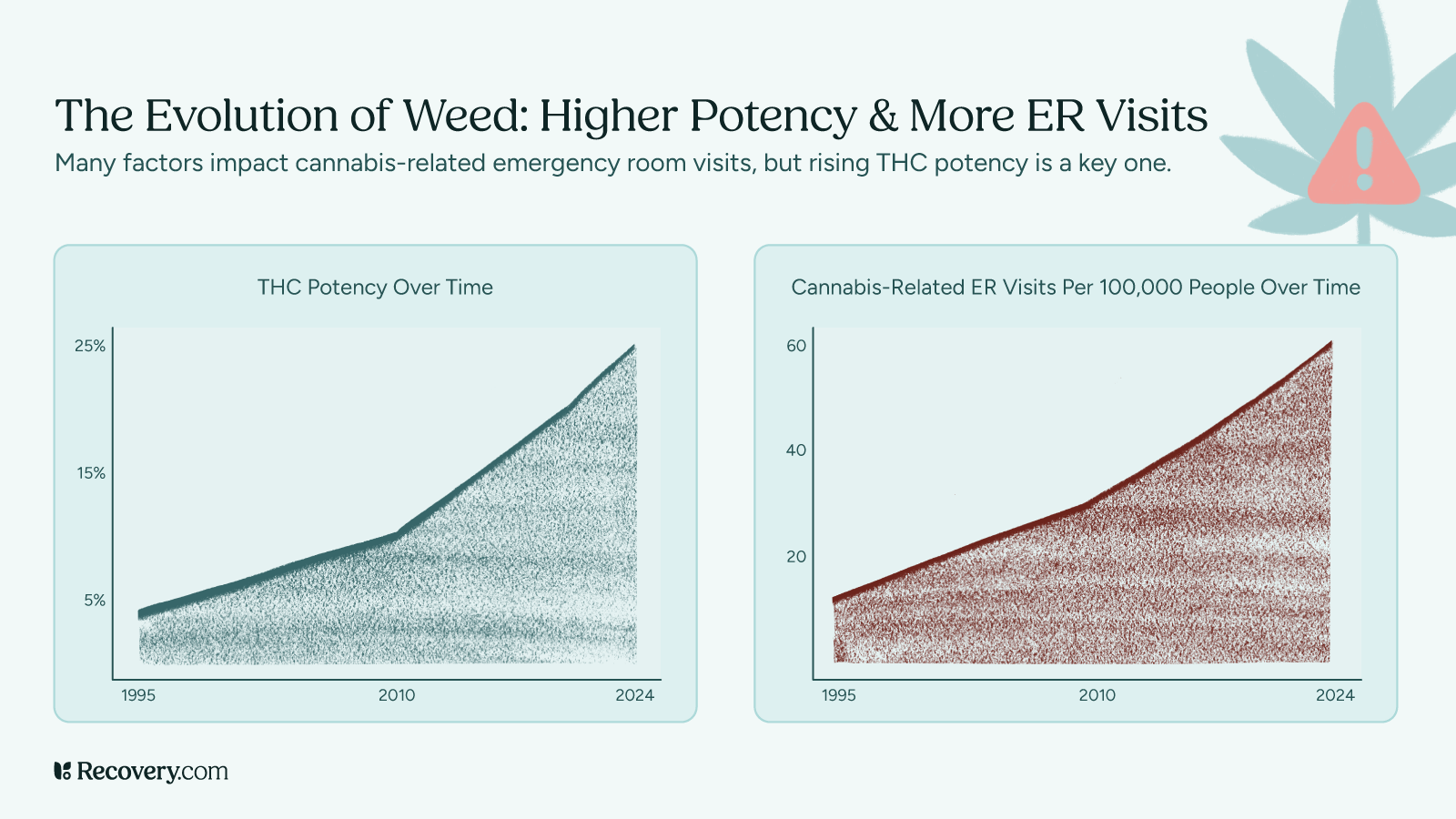
THC is fat-soluble, meaning it is stored in body fat and released slowly over time. The length of detox varies based on usage frequency, body composition, and metabolism. Again, there are differences depending on the person, the frequency of use, and the amount used.4
- Occasional users (1-2 times per month): THC is typically cleared within 3-7 days.
- Moderate users (several times a week): THC may be detectable for 1-2 weeks.
- Heavy users (daily or near daily): THC can remain in the body for several weeks to over a month.
Urine tests are the most common drug tests, but hair follicle tests can detect THC for up to 90 days. Drinking plenty of water is essential for flushing out THC metabolites.5 While most THC is excreted through feces, approximately 20% is eliminated via urine. Staying hydrated aids kidney function, allowing for more efficient metabolite excretion.
Additionally, proper hydration supports overall bodily functions and can alleviate withdrawal symptoms such as headaches and fatigue. There are detox drinks and other over-the-counter products that aim to aid in the detoxification process, though some of these products do not have research-based outcomes.
2. Exercise
Engaging in regular physical activity boosts metabolism6 and enhances mood. Aerobic exercises, such as running or cycling, increase heart rate and fat oxidation, which may aid in reducing THC stored in fat cells. Moreover, exercise stimulates overall wellness the release of endorphins, natural mood enhancers that can help combat anxiety and depression associated with withdrawal.
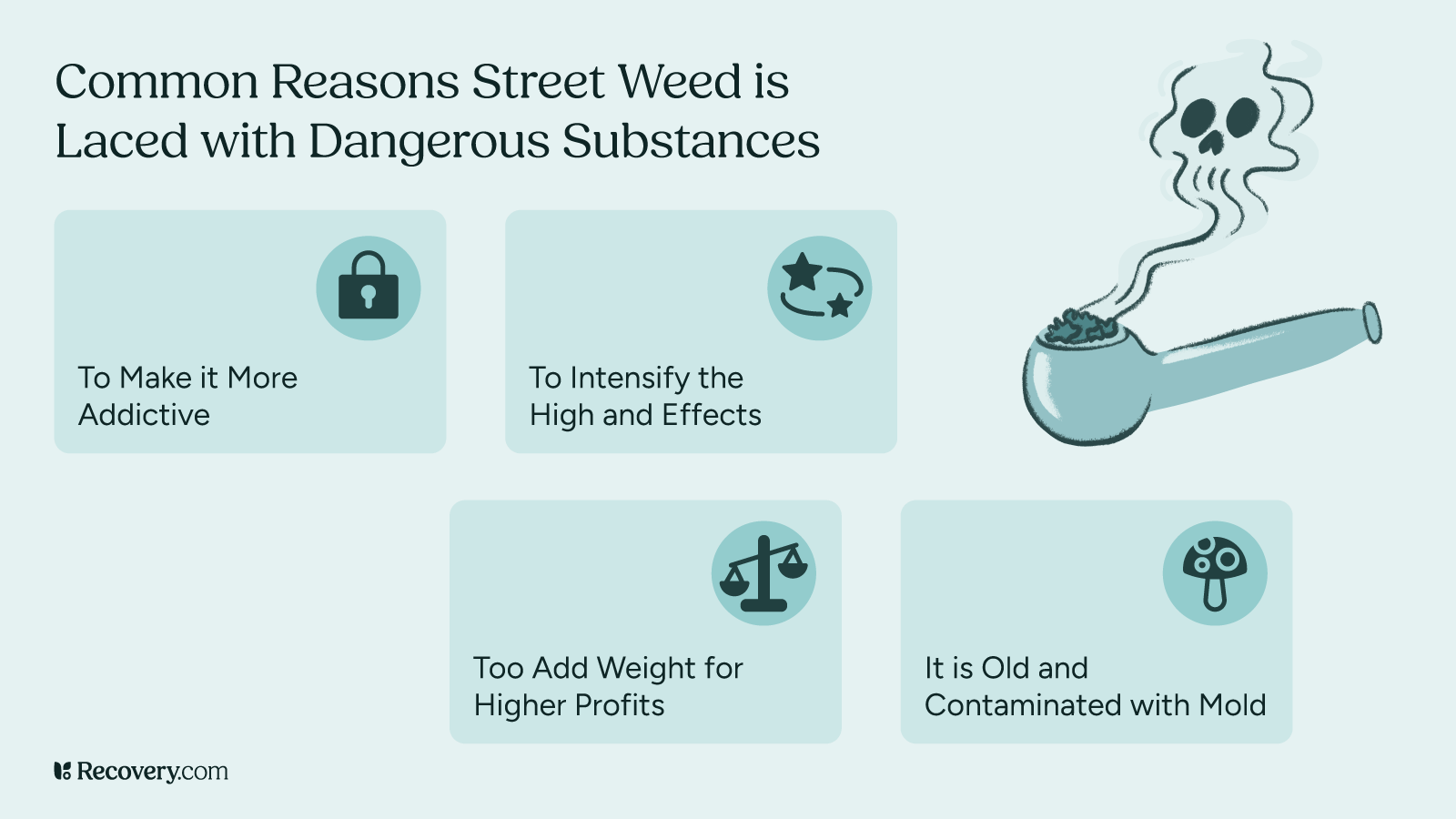
For years, there has been debate over whether marijuana is truly addictive. The reality? It depends on the person. Marijuana dependence can creep in slowly, like a friend who overstays their welcome.
Some people are more vulnerable to marijuana misuse.7 Those who begin use in adolescence are four to seven times more likely to develop a marijuana use disorder8 compared to those who start at a later age. Exercise can be a key part of managing marijuana withdrawal.
From a clinical perspective, what are challenging components of marijuana detox?
From a clinical perspective, marijuana detox can be challenging due to the gradual onset and variable intensity of withdrawal symptoms. These symptoms can include appetite changes, irritability, anxiety, and insomnia; they may not appear immediately and can last for days to weeks. This can make engagement in early treatment difficult. Additionally, psychological dependence and normalization of use in social settings can create barriers to motivation and sustained abstinence.
Andrew Schreier, ICS, CSAC, LPC, ICGC-II, BACC
3. Nutrition
A nutrient-rich diet supports brain function and reduces cravings. Foods rich in omega-3 fatty acids, such as walnuts, have been linked to improved cognitive performance. A balanced diet stabilizes blood sugar levels, preventing mood swings and reducing the likelihood of turning to marijuana to cope with stress or negative emotions.
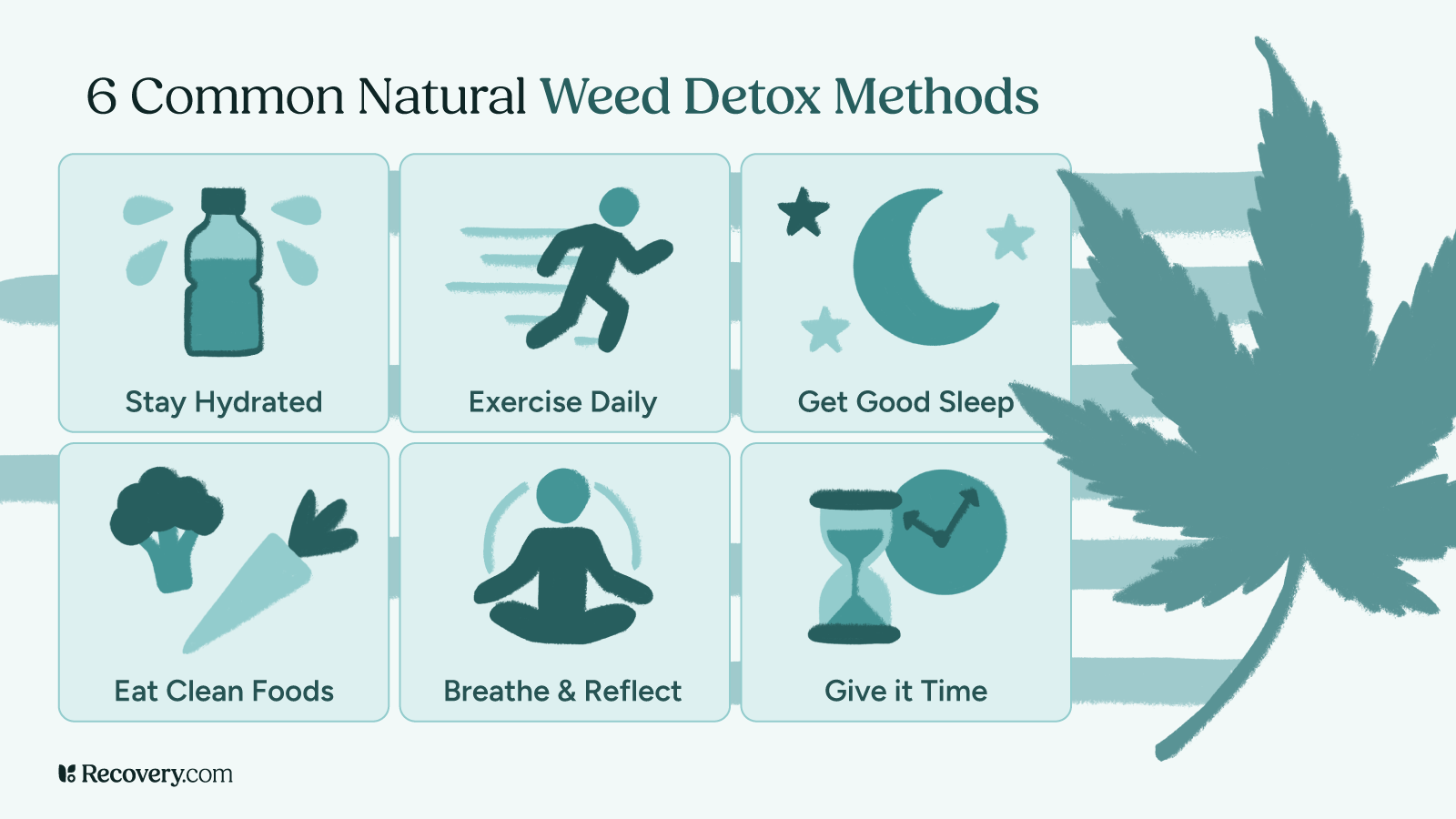
Research suggests that highly palatable foods, drug use, and addictive substances can create imbalances in the brain’s reward system.9 You can naturally reverse these effects by having a balanced diet with high-nutrient foods.
4. Sleep Hygiene
Establishing a healthy sleep routine is crucial for regulating mood and energy levels. Poor sleep can exacerbate irritability, stress, and other physical symptoms, making it challenging to maintain abstinence. Practicing good sleep hygiene—such as maintaining a consistent sleep schedule, creating a restful environment, and avoiding caffeine before bedtime—can improve sleep quality.
Research indicates that improving sleep quality10 significantly benefits mental health, reducing depression and anxiety, some of the most troubling withdrawal symptoms.
5. Support Groups
Engaging with support groups and addiction treatment can provide motivation and accountability. Some support groups follow a 12-step program, similar to Alcoholics Anonymous, offering a community of individuals sharing experiences and coping strategies. Participation in such groups fosters a sense of belonging and reduces feelings of isolation, which can be pivotal during the detox process.
In recent years, older adults have increasingly turned to marijuana or cannabis use, including the use of edibles or gummies, leading to a growing need for support in managing cannabis use disorder, often alongside other substance use issues.
Treatment for marijuana addiction or marijuana detox can also provide the peer support needed to abstain from or lessen drug use.
6. Therapy
Professional counseling, particularly Cognitive Behavioral Therapy (CBT), addresses underlying mental health concerns and triggers associated with marijuana use and weed detox.
CBT helps individuals identify and modify negative thought patterns and behaviors, equipping them with coping strategies to manage cravings and prevent relapse. Research shows that CBT is effective in reducing cannabis use severity and improving overall psychological well-being.
Incorporating these natural strategies can facilitate marijuana detoxification and support long-term recovery. A holistic approach that addresses both physical and psychological dependence is essential. Consulting healthcare professionals can provide personalized guidance tailored to individual needs.
Several risk factors contribute to the development of cannabis use disorder, including:
- Mental health disorders such as anxiety or depression
- Family history of substance use
- Peer pressure and social influences
- Loneliness or social isolation
- Lack of family involvement and support
- Easy access to marijuana
- Use of other substances like opioids
By understanding these risk factors, individuals can seek preventative measures and professional support to mitigate the long-term effects of cannabis dependence.
Dependence occurs when the brain adapts to regular THC exposure, leading to withdrawal symptoms when use ceases. Research11 estimates that about 3 in 10 cannabis users (roughly 30%) develop cannabis use disorder or addiction. This risk is notably higher for those who use cannabis frequently or begin using it when they are young.
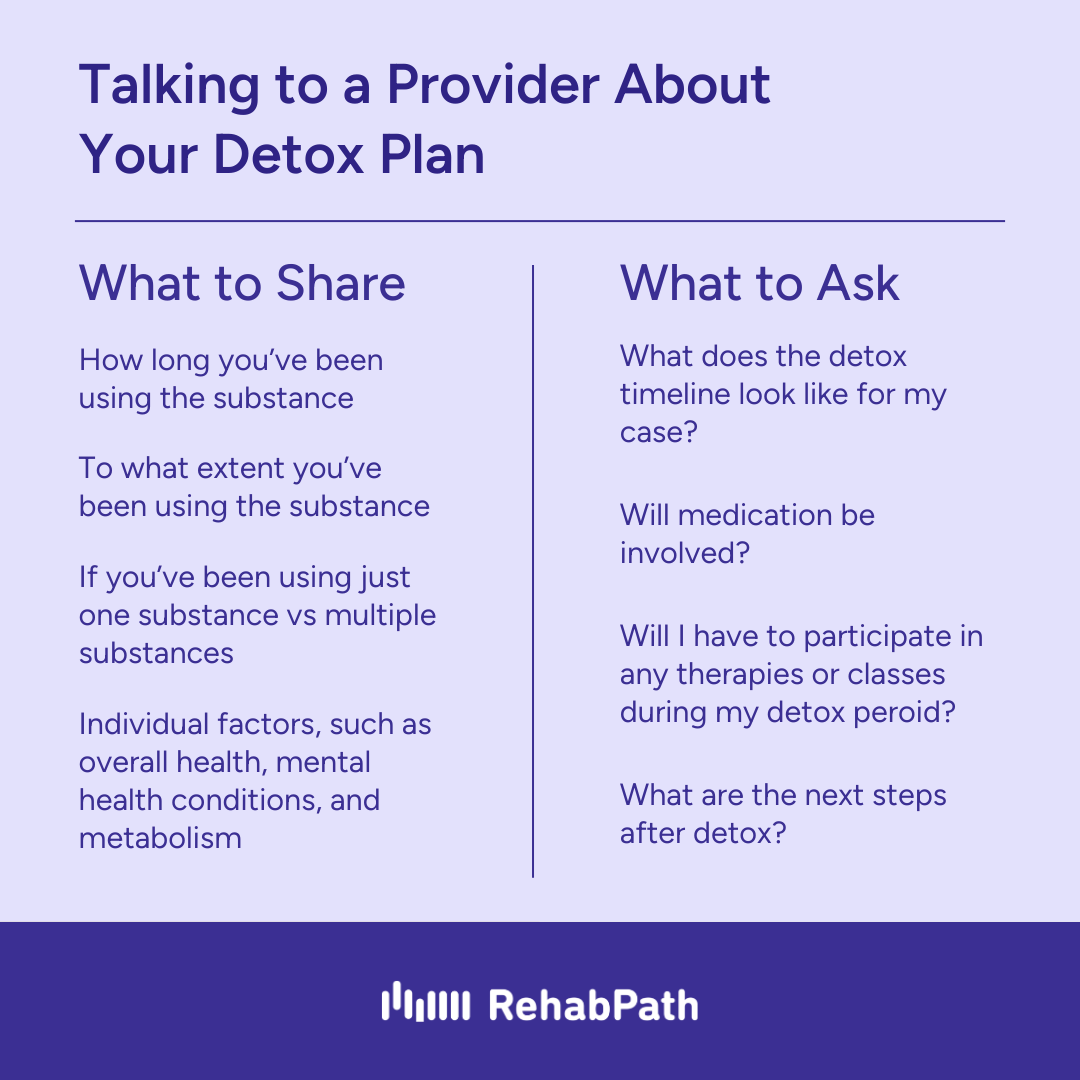
Are there treatment options for marijuana dependence?
Cannabis is one of the most widely used substances in the United States. While many people may not attend a residential treatment setting for Cannabis, some people may find benefit in attending individual sessions for cannabis treatment or intensive outpatient treatment. Cognitive behavioral therapies are evidence-based for the treatment of cannabis use. In addition to treatment, many individuals have found freedom from chaotic cannabis use by attending 12-step recovery meetings, Dharma recovery, SMART recovery, White Bison, Refuge Recovery, and other self-help groups.
Tanya Kraege LCSW, CSAC, CCAR RC, WI CPS | Ventus Rex
Can You Use Medications for Marijuana Detox?
While no FDA-approved medications exist specifically for marijuana detox, some medications can help manage withdrawal symptoms:
- Benzodiazepines (e.g., Valium, Xanax) for severe anxiety and sleep disturbances.
- Selective serotonin reuptake inhibitors (SSRIs) (e.g., Prozac, Zoloft) for mood regulation.
- Over-the-counter pain relievers for headaches and discomfort.
- Melatonin or other sleep aids or supplements to improve sleep quality.
These medications should only be used under medical supervision to prevent dependence or adverse effects. Seeking medical advice can help determine the best treatment options for detox and withdrawal management.
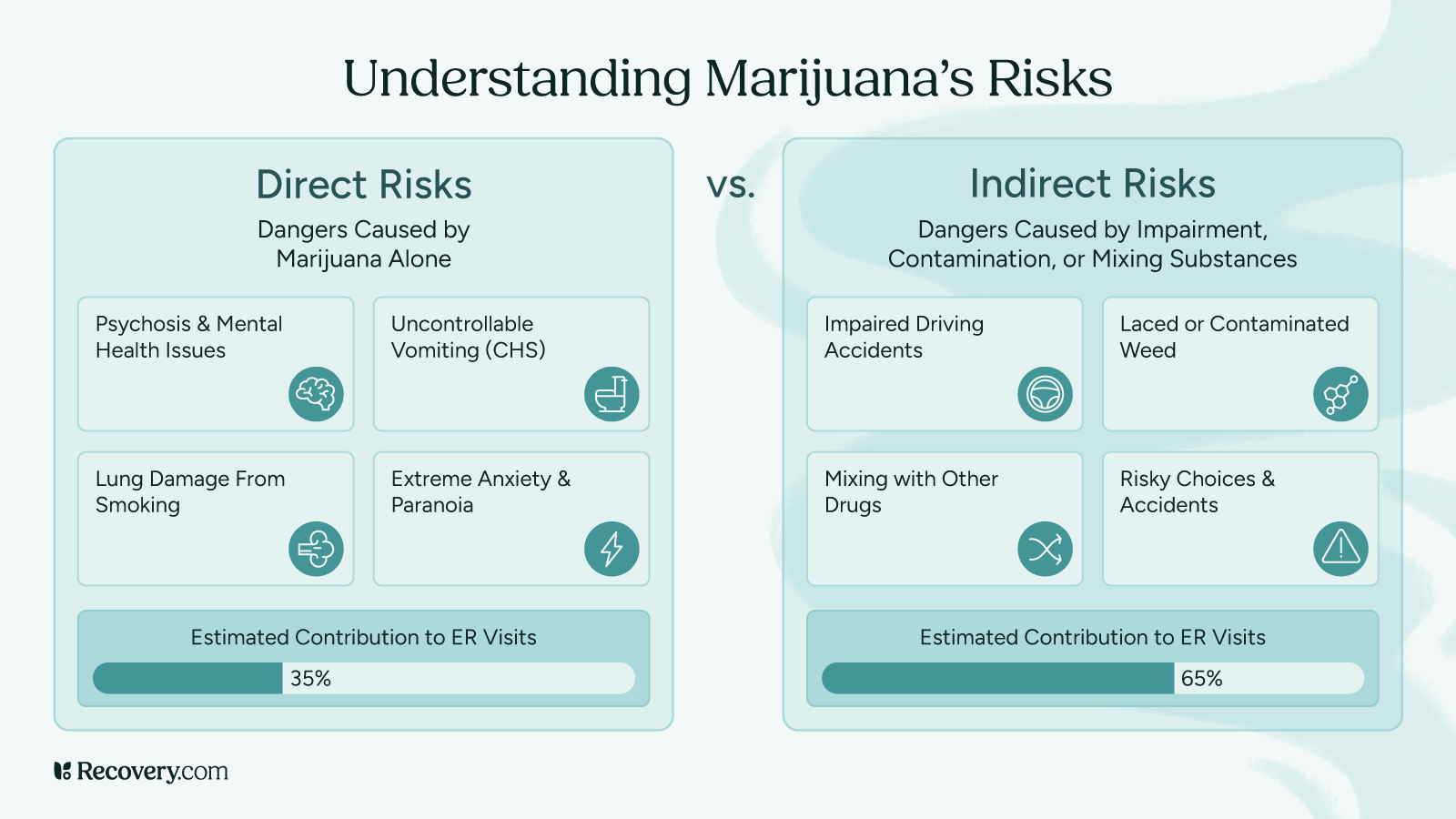
Are There Risks of Detoxing from Marijuana on Your Own?
Quitting cold turkey or relying solely on natural remedies may seem straightforward, but withdrawal symptoms can be more intense than expected. While cannabis is legal in many places, it remains addictive and potentially harmful. Detoxing without proper support from medical professionals can be challenging and pose risks.
Potential Risks of Self-Detox:
- Increased anxiety and depression
- Higher likelihood of relapse due to cravings
- Poor sleep quality and fatigue affecting daily life
- Difficulty managing withdrawal symptoms without support
Seeking medical supervision through an addiction treatment program, detox programs, or a detox center, can improve success rates and provide necessary support during detoxification.
What advice would you give to someone considering quitting marijuana who is worried about withdrawal symptoms or relapse?
I would advise anyone seeking recovery from any substance to get adequate support. This can take different forms, but possible elements would include therapy with an addiction expert, self-help groups for community, and even Intensive Outpatient Treatment, and in cases of chronic addictions, inpatient treatment. I also encourage users to know that investing in recovery brings amazing benefits!
Tim Lineaweaver, LMHC
Where Can I Find Help for Marijuana Addiction?
If you or a loved one is struggling with marijuana dependence, professional help is available. There are a wide range of treatment options include:
- Inpatient programs: Intensive, supervised detox and therapy for severe cases.
- Outpatient programs: Flexible treatment that allows individuals to maintain daily responsibilities.
- Behavioral therapy: Cognitive-behavioral therapy (CBT) helps individuals identify triggers and develop coping strategies.
- 12-step programs: Support networks like Marijuana Anonymous12 offer peer encouragement and structure.
Understanding the marijuana detox process helps individuals take proactive steps toward recovery and well-being. Whether detoxing at home or seeking professional treatment, support, patience, and self-care are key. If you or someone you know is struggling with marijuana use, professional support can make a significant difference.
Detoxing from marijuana is not just about clearing THC from your body—it’s about reclaiming your mental and emotional well-being. While the withdrawal process can be uncomfortable, it is temporary, and every step you take toward recovery is a step toward feeling better.
Addiction treatment programs and specialized treatment centers can offer tailored guidance to ensure a safer, more manageable detox that provide evidence-based treatment options. No matter where you are in your journey, recovery is possible, and support is available every step of the way.
FAQs
Q: What is the best detox for marijuana?
A: The best way to detox from marijuana is through natural detoxification, which includes hydration, exercise, a healthy diet, and time. While detox products claim to speed up the process, there is little scientific evidence to support their effectiveness. A gradual reduction in use and a well-balanced lifestyle are the safest and most effective natural methods.
Q: How much water should you drink to flush out marijuana?
A: Drinking water does not directly flush THC from your system but staying hydrated supports kidney function and overall detoxification. Aim for 8–12 cups of water daily to maintain proper hydration. Be cautious, as excessive water intake can lead to water intoxication and dilute urine, which may raise suspicion in a drug test.
Q: How is marijuana eliminated from the body?
A: THC, the psychoactive compound in marijuana, is metabolized by the liver and broken down into metabolites. These metabolites are then stored in fat cells and gradually eliminated through urine, feces, and sweat. Since THC is fat-soluble, it takes longer to clear from the system compared to other substances.
Q: What’s the fastest way to clear your system?
A: There is no instant way to eliminate THC, but the following can help:
- Hydration – Supports kidney and liver function.
- Exercise – Burns fat where THC is stored (but avoid intense exercise right before a test, as it can temporarily raise THC levels in blood).
- Healthy Diet – High-fiber foods promote THC elimination through the digestive system.
- Time – The only guaranteed way to clear THC is to wait it out.
Q: How long does it take to detox from cannabis?
The duration of marijuana detox13 depends on frequency of use, metabolism, and body fat percentage. Generally:
- Occasional users (1–2 times a week) – Detox in 3–7 days.
- Moderate users (3–4 times a week) – Detox in 1–2 weeks.
- Heavy users (daily use) – Detox can take several weeks to a month or more.
Read more about THC detox timelines.
Q: What is the duration of marijuana detox?
A: Marijuana detox symptoms can last 7–14 days, with withdrawal peaking within the first 3–5 days according to a typical withdrawal timeline. Symptoms may include irritability, insomnia, mood swings, and appetite changes. Heavy users may experience Post-Acute Withdrawal Symptoms (PAWS) for weeks or months.
Q: How do detox drinks work?
A: Detox drinks typically work by diluting urine to lower THC metabolite concentration. Many contain creatinine and B vitamins to prevent dilution detection. While they may temporarily alter test results, they do not remove THC from the body. Their effectiveness is debated.
Q: How long does THC stay in the body?
A: THC detection depends on the type of drug test:
- Urine test – Detects THC for 3–30+ days (longer for frequent users).
- Blood test – Detects THC for 1–2 days (up to a week for heavy users).
- Saliva test – Detects THC for 24–72 hours.
- Hair test – Detects THC for up to 90 days.
Learn more about THC detection times.
Q: Are you covered for addiction treatment?
A: Many insurance plans cover marijuana addiction treatment, including detox programs, therapy, and inpatient rehab. Check with your provider to see if detox and recovery services are included in your coverage or discuss your options for a treatment plan.
Q: How do marijuana drug tests work?
A: Drug tests detect THC metabolites in urine, blood, saliva, or hair. The most common test is the urine test, which identifies THC-COOH, a byproduct of THC metabolism. Learn more about marijuana drug testing methods.
Q: Can exercise help speed up marijuana detox?
A: Yes, exercise can help reduce THC levels over time by burning fat where THC is stored. Cardio workouts and strength training increase metabolism, but they should be avoided right before a test, as they can temporarily raise THC levels in blood.
Exercise may slightly accelerate detox, but THC still takes time to leave the body. Combining exercise with hydration and a clean diet supports natural detox. However, there’s no quick fix—the most reliable detox method is time and professional support.