If you’re feeling overwhelmed, hopeless, or unsure how to keep going, please hear this: what you’re feeling is real—and your life deeply matters.
Suicidal thoughts can feel isolating and unbearable, but there is help and there is hope.
Whether you’ve struggled in silence for a long time or these feelings are new and frightening, reaching out for support can be the first step toward relief. Reaching out for help, talking to a mental health professional,1 or connecting with a support network2 can make a critical difference.
In your clinical experience, what are the most effective ways to support someone in the midst of a suicidal crisis—and how can everyday people offer meaningful help?
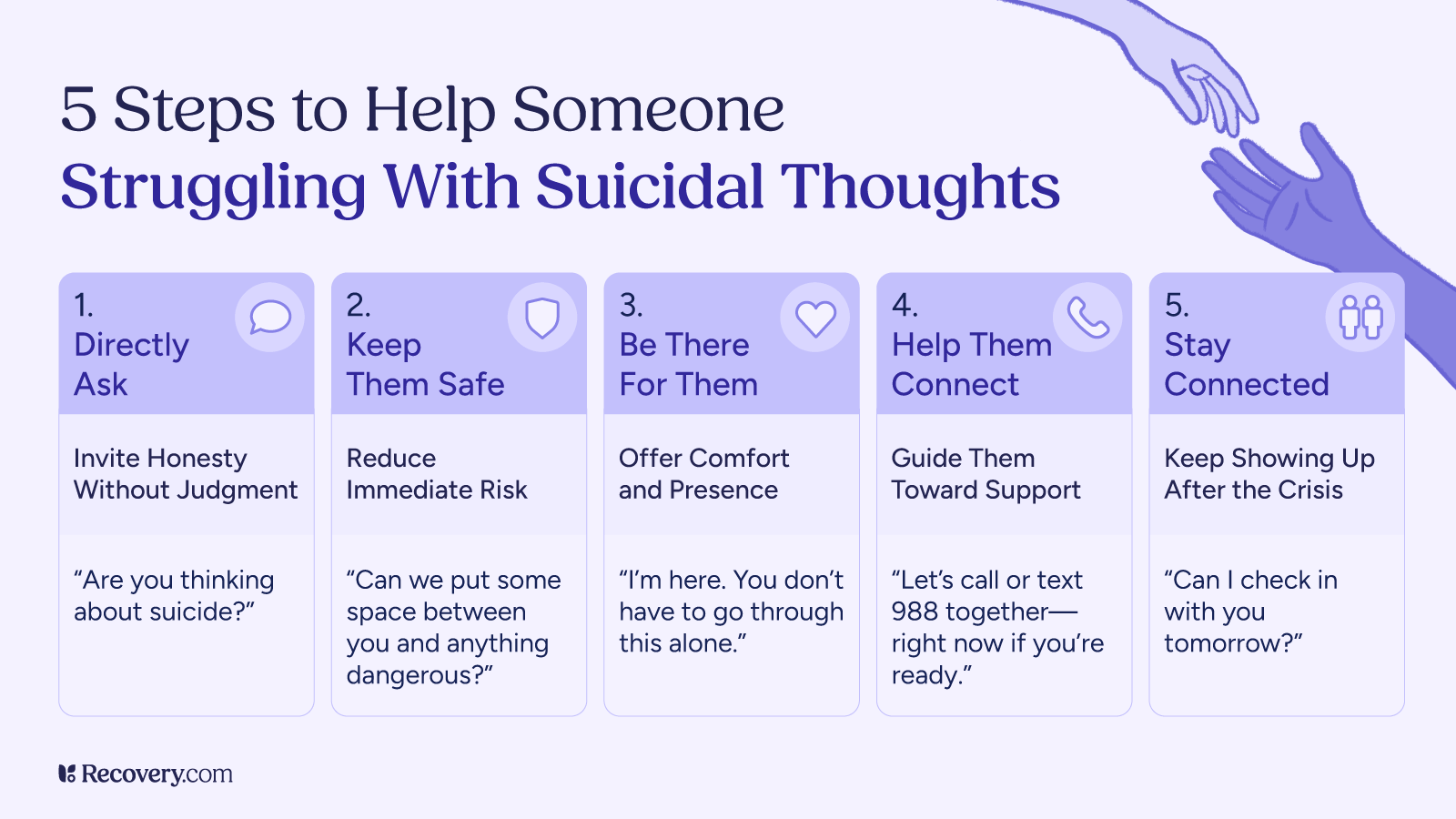
To support someone in a suicidal crisis, it’s most important to help them stay safe and to stay connected. Ask them how they’re feeling, listen to them nonjudgmentally, and talk about their suicidal thoughts openly and clearly. If the person wants professional support, offer to help them call 988, text ‘HOME’ to 741741, or get to the closest crisis center or emergency room. Otherwise, offer to support them in other ways that you feel comfortable—staying with them, going on a walk or watching TV together, connecting them with other loved ones, helping them complete an errand or get something to eat, or continuing to talk about what’s going on—and then follow-up with a caring text, call, or check-in later.
Kiki Fehling, PhD, DBT-LBC
Meeting Yourself Where You Are
When experiencing suicidal thoughts, even basic self-care can feel overwhelming. Instead of setting expectations to immediately build a support network, acknowledge where you are right now. Getting through the next hour, or even the next five minutes, is a valid goal. You can meet yourself where you are with grace and acceptance.
Why Do I Feel Suicidal?
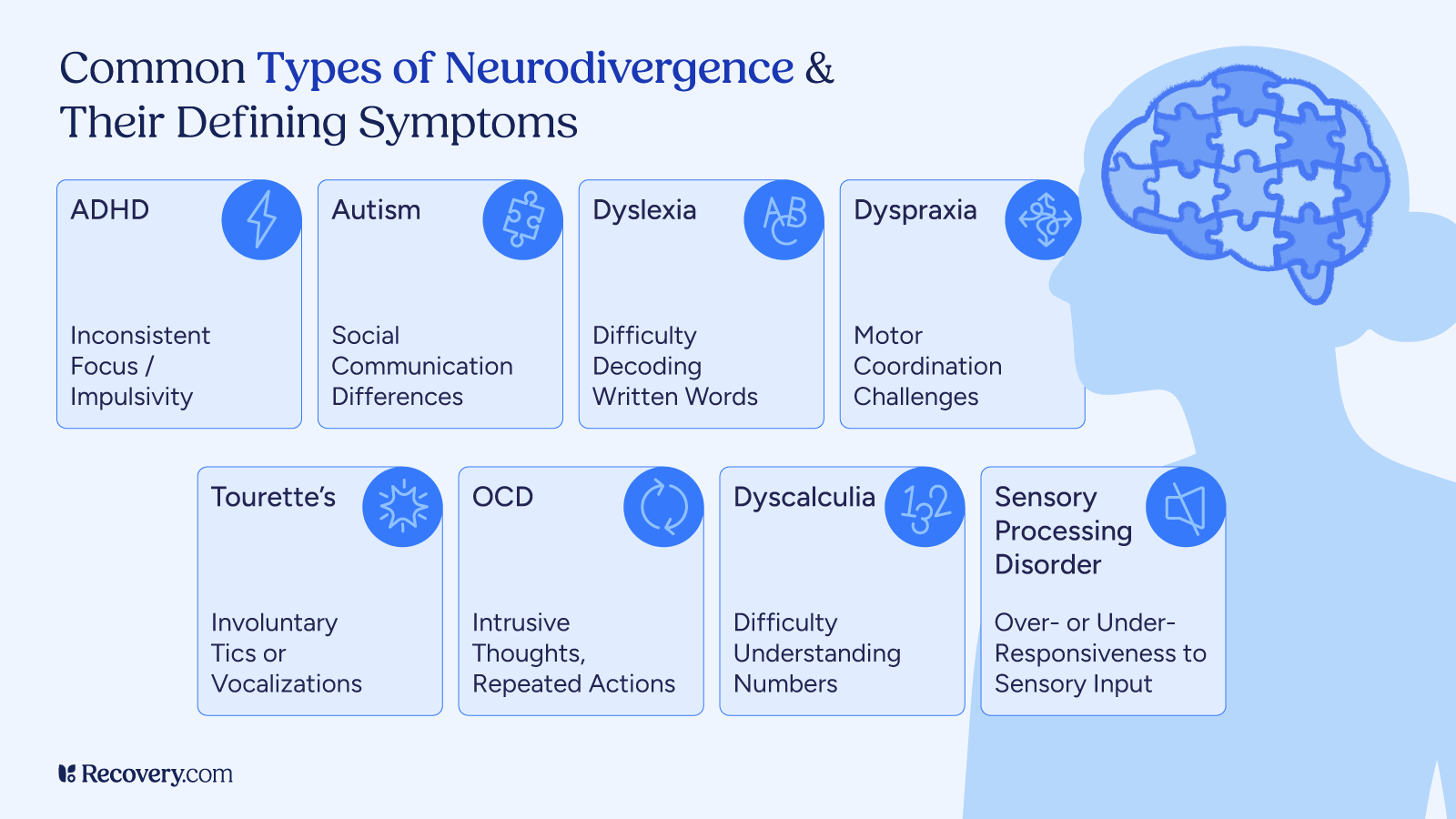
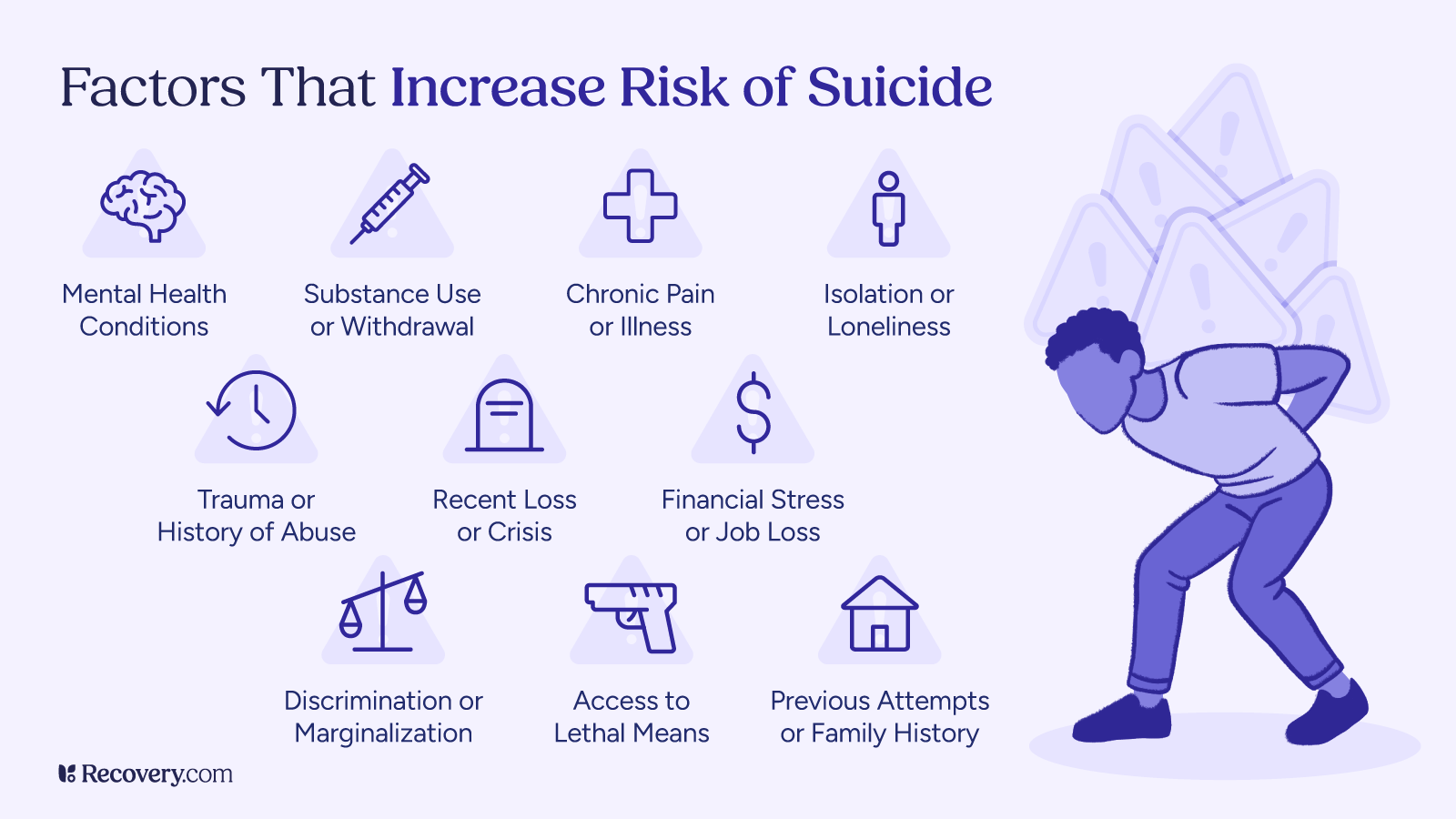
Suicidal feelings often arise from a mix of emotional, psychological, and environmental factors, including:
- Mental health conditions3 like depression, bipolar disorder, or anxiety
- Chronic health problems4 or physical pain
- Substance use or withdrawal
- Isolation, shame, trauma, or identity-based discrimination
Why Suicide Can Seem Like the Only Option
During a mental health crisis, your ability to think clearly or see alternatives may become impaired. Thoughts of suicide can feel like the only escape from emotional pain, but there are other ways to find relief.
Depression, trauma, or overwhelming stress can cloud your judgment and make it difficult to see beyond your current suffering. This cognitive distortion, where everything feels permanent and hopeless, is a hallmark of suicidal thinking. In these moments, the brain’s ability to process options narrows, making death seem like the only way out.
But suicidal thoughts are symptoms, not truths. With the right support, your perspective can shift, and you can begin to see other ways to reduce pain and reclaim your life.
A Suicidal Crisis Is Almost Always Temporary
Strong suicidal urges often peak and fade. Many people who survive an attempted suicide later report feeling grateful they did not end their lives. Crisis support can help you move through this moment safely.
Intense emotional pain can convince you that it will last forever, but it won’t. Research shows that suicidal thoughts often rise sharply and then fade,5 much like a wave cresting before it recedes.
Many people who survive suicide attempts report that they felt differently within minutes, hours, or days. They often express deep relief and gratitude for surviving. If you can ride out the storm—even for a few minutes—it opens the door for healing. Reaching out for help, calling a crisis line, or talking to someone you trust can be the first step toward making it through this moment alive and supported.
Even Problems That Seem Hopeless Have Solutions
You may not see it now, but solutions exist—even if they don’t feel immediately accessible. Talk therapy and peer support6 can help uncover new ways of coping.
When you’re overwhelmed, it can feel like your problems are too big or too complex to fix. But even the most painful circumstances like abuse, loss, shame, financial strain, or addiction, can improve with time, care, and support.
Therapies like Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) have helped countless people develop tools to manage emotions and rebuild their lives. Peer support groups, faith-based communities, and crisis counselors can also offer perspective and encouragement. You don’t have to solve everything alone, and you don’t have to do it all at once. Small steps can lead to profound change.
If You’re Feeling Suicidal, Take These Immediate Actions
If you are in immediate danger, please call 988 or visit the nearest emergency room. You can also reach out to:
- A close friend or family member
- A crisis counselor via 988 chat
- A therapist, doctor, or outpatient provider
Small steps can interrupt harmful patterns. Try grounding techniques, journaling, or connecting with someone you trust.
When the urge to self-harm feels strong, commit to waiting—even for just 24 hours. This pause gives you time to access coping strategies and reconnect with support systems.
Suicide Crisis Lines Worldwide
- United States: 988 Suicide & Crisis Lifeline7 or call/text 988
- United Kingdom: Samaritans at 116 123
- Canada: Talk Suicide Canada at 1-833-456-4566
- Australia: Lifeline Australia at 13 11 14
- International: Find helplines at Befrienders Worldwide8
Plan Ahead and Create a Suicide Prevention Plan
When you’re struggling with suicidal thoughts—or supporting someone who is—it can be difficult to see a way forward. But creating a suicide prevention plan offers a proactive, lifesaving path through crisis. By identifying support systems, warning signs, and personalized coping tools ahead of time, you can regain a sense of control and safety. The following strategies combine professional care, community support, and daily wellness practices to help prevent suicidal ideation and promote long-term mental health.
- Preventing Suicidal Ideation: Preventing suicidal ideation involves several approaches that address mental health, social connections, and lifestyle factors. Here are some evidence-based strategies:
- Seek Professional Help: Mental health professionals can provide proper diagnosis and treatment for conditions that may contribute to suicidal thoughts, such as depression, anxiety disorders, bipolar disorder, and substance use disorders. This can include therapy, medication, or a combination of both.
- Build a Support Network:9 Maintain regular contact with supportive friends, family members, or support groups who can provide emotional support during difficult times. Having people to talk to openly about feelings can reduce isolation.
- Develop Healthy Coping Skills: Learning healthy ways to manage stress and emotional pain is crucial. This might include mindfulness meditation, deep breathing exercises, physical activity, journaling, or engaging in creative outlets like art or music.
- Create a Safety Plan:10 Having a written plan that outlines warning signs, coping strategies, people to contact for help, and ways to make your environment safe can be invaluable during a crisis. This plan should be easily accessible.
- Limit Access to Means: Reducing access11 to potentially lethal means, such as firearms or large quantities of medication, is an important preventive measure.
- Address Substance Use: Alcohol and drugs can worsen suicidal thoughts and impair judgment. Getting help for substance use issues can reduce suicide risk.
- Maintain Physical Health: Regular exercise, adequate sleep, and proper nutrition can positively impact mental health and reduce symptoms that may contribute to suicidal thoughts.
How to Help Someone Who is Suicidal
Experiencing suicidal thoughts or watching a loved one struggle with suicidal feelings can be frightening and overwhelming. It’s important to know that suicidal ideation is often a symptom of underlying mental illness or emotional distress, and help is available.
If someone is showing warning signs such as talking about ending their own life, withdrawing from others, or engaging in self-harm, they may be at immediate risk and need urgent care.
- Encourage them to connect with a mental health professional or call a crisis line like the 988 Suicide & Crisis Lifeline can be life-saving. Trained counselors can provide compassionate, non-judgmental support and guide them through mental health crisis situations.
- Offer alternatives like creating a safety plan, joining a support group, or just being part of their support network can reduce their risk of suicide. According to the National Institute of Mental Health, asking direct questions like “Are you thinking about hurting yourself?” shows concern and does not increase the chance of a suicide attempt—instead, it opens the door for support.
Continued follow-up after a crisis and access to affordable mental health care are essential, especially for those affected by substance abuse or facing barriers to mental health services. Whether you’re a family member, a friend, or a peer, knowing how to help someone by recognizing the signs and connecting them to professional help like Samaritans or 988 can truly make a difference.
No matter how dark things feel right now, this moment does not define your future.
What do you wish more people understood about the nature of suicidal thoughts, and how can early intervention or mental health literacy reduce stigma and save lives?
As a multi-attempt survivor, I have lived with stigma surrounding suicide my entire life and was always told how it is a ‘sin’ or ‘selfish’ just to have those thoughts. Working in mental health has shown me time and time again how common suicidal ideation is, and how individuals should have the ability to openly talk about and receive care and compassion in response.
When we talk about early intervention, we need to address how the discussion surrounding suicide needs to change, and entire communities need access to resources, such as NAMI, that provide education on suicide & prevention. The more we fight the idea that suicide and suicidal ideation are ‘taboo’ topics, the more we are removing shame and opening the conversation, which will save lives.
Sage Nestler, MSW | Releasing the Phoenix
It’s okay if reaching out feels impossible right now. When you’re in that kind of pain, asking for help can take more strength than most people will ever understand. Suicidal thoughts can cloud your sense of hope, making it feel like there’s no way out. But, it is important to remember that these thoughts are not permanent. You don’t have to face them alone.
Whether it’s calling a crisis line, confiding in a trusted friend, or simply making it through one more day, every small step is a powerful act of survival. You deserve support. You deserve healing.
There are people who care about you, who want to help you, and who believe in your worth—especially when you’re struggling to see it yourself. Treatment is available that meets you where you are, without judgment or pressure.
FAQs
Q: What should I do if someone I know is suicidal?
A: If someone is expressing thoughts of suicide, stay with them and help them feel heard. Encourage them to contact a crisis counselor or call/text the 988 Suicide & Crisis Lifeline. If they are in immediate danger, do not leave them alone—call 911 or take them to the nearest emergency room.
Q: What are the 5 action steps for helping someone in emotional pain?
A: According to the National Institute of Mental Health, the five steps are:
- Ask
- Keep them safe
- Be there
- Help them connect
- Stay connected
These steps can reduce the risk of suicide and make a critical difference in someone’s recovery.
Q: What not to say to someone who is suicidal?
A: Avoid saying things that minimize their pain like “just snap out of it” or “you have so much to live for.” These statements can feel invalidating. Instead, listen without judgment and direct them toward mental health support.
Q: How to deal with a loved one being suicidal?
A: Support them with empathy and without panic. Help them develop a safety plan, remove access to means of self-harm, and stay in close contact. Encourage them to seek professional care, such as talk therapy or outpatient services.
Q: Why does someone have suicidal thoughts?
A: Suicidal thoughts often stem from complex interactions between mental illness, trauma, substance use, physical pain, or intense emotional distress. Life stressors like relationship breakdowns or discrimination can worsen these feelings, especially in marginalized groups like the LGBTQ+ community.
Q: What is suicidal ideation?
A: Suicidal ideation refers to thoughts about or planning suicide. These thoughts can range from passive (“I wish I weren’t here”) to active (“I want to end my life”). Ideation doesn’t always lead to action but should always be taken seriously.
Q: How can I know if they’re in immediate danger?
A: Immediate danger signs include talking about wanting to die, having a plan, giving away possessions, or withdrawing suddenly. According to the 988 Lifeline, any mention of intent or means to attempt suicide requires urgent intervention.
Q: Who is most at risk of suicide?
A: High-risk groups include people with untreated mental health conditions, individuals with a history of trauma or abuse, those with access to lethal means, and members of marginalized communities. LGBTQ+ youth, veterans, and those with chronic illnesses or a history of substance use are especially vulnerable.
Q: Is there a link between self-harm and suicide?
A: Yes. While not all self-harm leads to suicide, individuals who engage in self-injury are at a higher risk of suicidal behavior. Both are serious signs of emotional distress and require compassionate intervention.
Q: What are warning signs for suicide?
A: Warning signs include increased substance abuse, feelings of hopelessness, social withdrawal, changes in sleep or eating, and expressing a desire to die. The CDC provides a comprehensive overview of behavioral risk indicators.
Q: How can I support a friend who is feeling suicidal?
A: Be present, listen nonjudgmentally, and offer to help them access a helpline or mental health professional. Encourage connection to a support group or peer support community. Just knowing someone cares can be powerful.