Getting professional help for alcohol use disorder, drug use, and other addictions is possible even if you don’t have health insurance or a lot of money in the bank.
We understand how concerns over the cost of rehab may still prevent you from working toward recovery. Keep reading to learn how much rehab costs and what financing options might be available to you.
1. Price Levels of Addiction Treatment
The variety of treatment options and therapies available in drug and alcohol rehabs is extensive. Because of this, there’s not really an average cost for rehab and different programs can have vastly different costs.
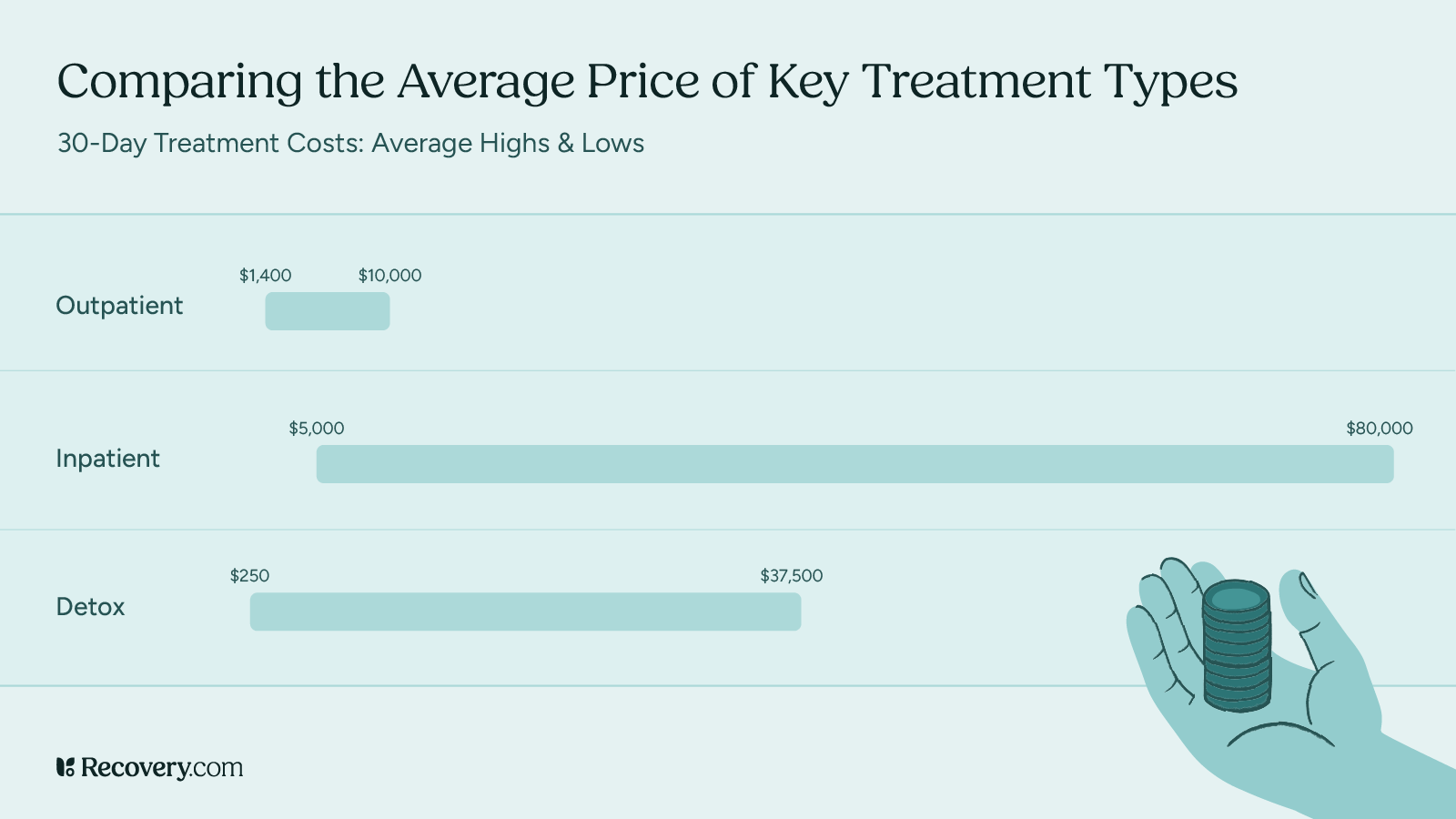
In the U.S., the cost of residential rehab programs can range from more affordable options that cost less than $10,000 to premium, single-client addiction treatment centers that can cost upwards of $80,000.
Several elements determine how much treatment at different rehab facilities will cost.
2. Factors That Influence the Cost of Rehab
Type of Treatment
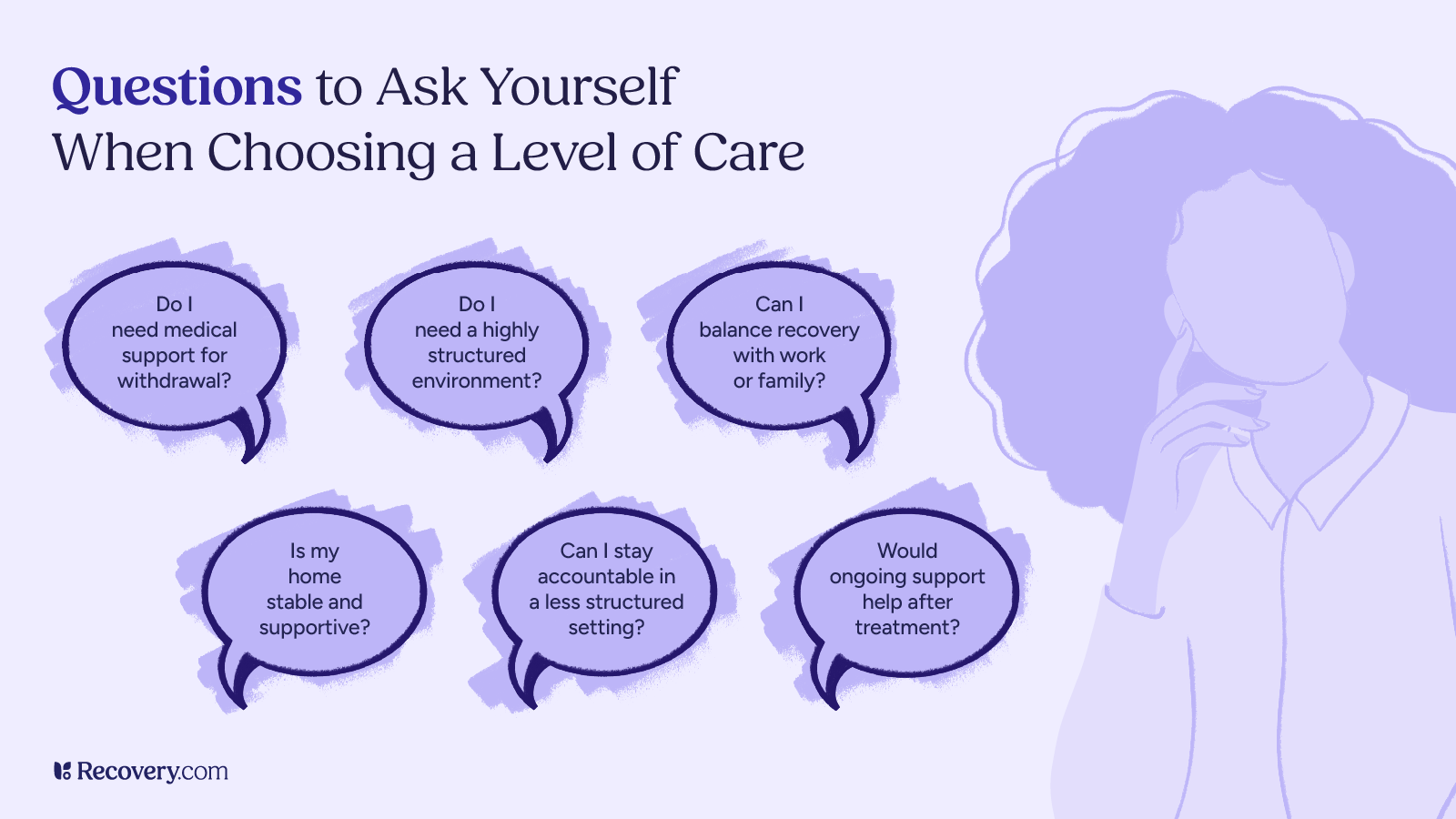
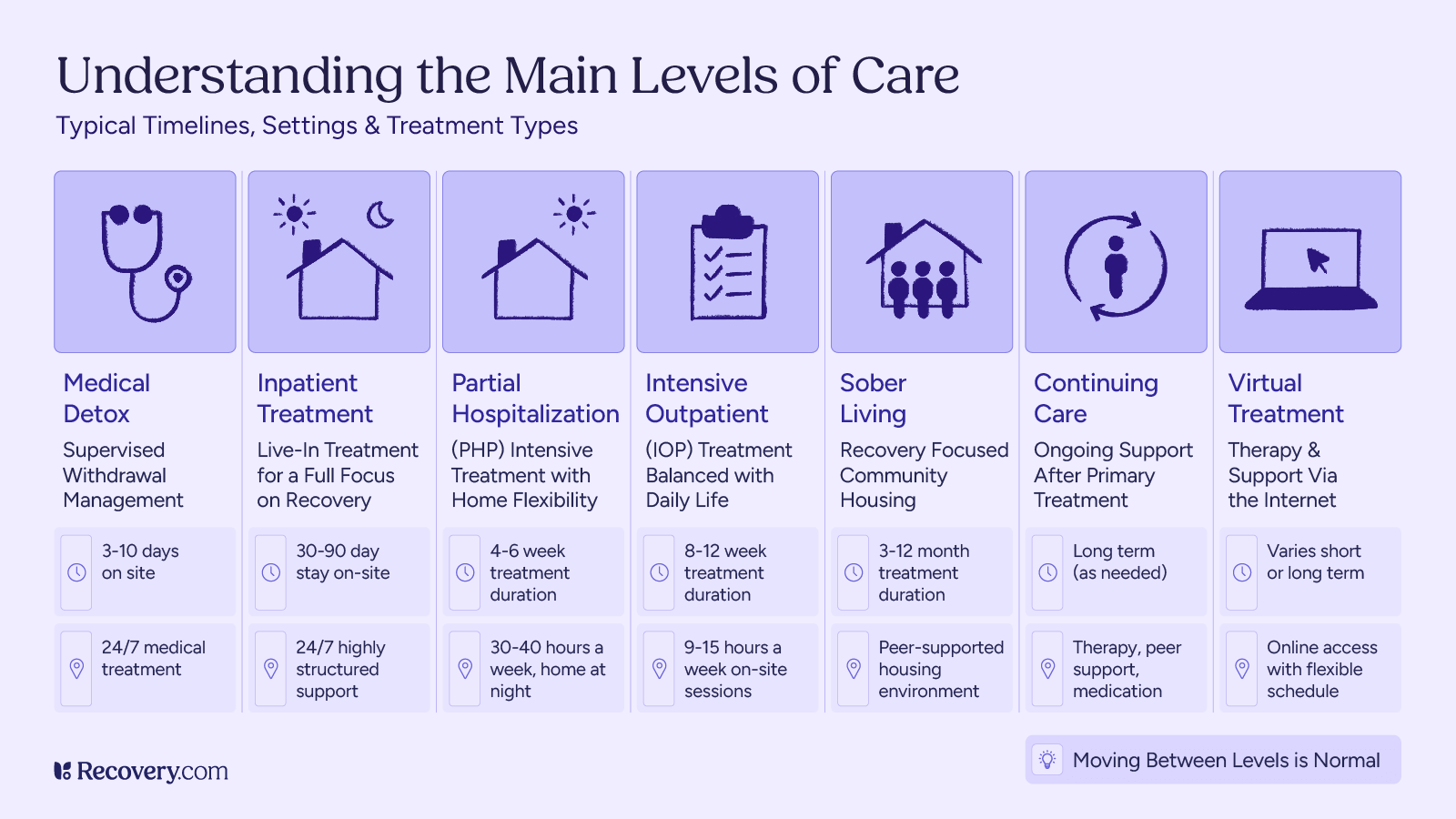
The word “rehab” is an older way to refer to many kinds of treatment programs. The most common of these are detox programs, outpatient treatment, intensive outpatient programs, partial hospitalization programs (PHP), and inpatient treatment, also known as residential rehab. The difference between most of these treatment plans is whether you go home every day after treatment sessions (outpatient programs) or whether you live and receive care 24/7 for an extended amount of time at a facility (inpatient care/residential).
These types of treatment often include resources for family members and loved ones, support groups, and connections to various helplines and other resources for when you leave treatment.
Some facilities provide medical detox, which includes medical oversight for detoxification. These programs may use medications to manage withdrawal symptoms, like Methadone for opioid use. Inpatient rehab costs can be higher if the program includes medical detox.
Typically, more time spent at a center results in higher costs for addiction treatment programs. One study by the U.K.’s National Institute for Health and Care Excellence (NICE) reports that “a course of outpatient treatment averaged less than 10% of the cost of inpatient treatment.”1 Though residential treatment programs may be slightly more effective for some people, “preference might still be given to non-residential treatment based on cost-effectiveness.”
How do you pay for rehab?
Paying for treatment can feel overwhelming, but there are many options available that include insurance coverage, sliding-scale fees, state-funded programs, and even community-based resources like churches or nonprofit organizations. It’s crucial to make financial information more available, accessible, and easy to understand so that cost isn’t an immediate deterrent to seeking care. When financial options are difficult to access or navigate, they can become a major barrier, so creating a transparent and supportive process helps ensure that people can get the help they need.
Andrew Schreier, ICS, CSAC, LPC, ICGC-II, BACC
Location
Highly desirable settings, like the beach or mountains, will likely increase the cost of treatment. But, traveling abroad for substance use treatment can sometimes be less expensive than getting treatment locally because of the cheaper costs of operations in different locales, like Thailand or Bali. Garry Irvin, Admissions Manager at The Dawn Rehab describes the cost of drug rehab in Thailand:2
Clients coming from Western countries, from the US, from Australia, UK, would be able to get three or four months’ worth of treatment here for what they would get for a month back at home.
Services Offered
The cost of rehab may increase with additional treatments like detox, medication-assisted treatment (MAT), complementary therapies, outpatient care, or aftercare. These may be offered as optional “add-ons” at an extra cost depending on the treatment facility.
Program Length
The standard length of say at a residential rehab facility is 30, 60, or 90 days. Program rates generally increase according to how long you stay.
Amenities
Treatment at centers with luxurious accommodations and exclusive amenities, like pools and lounges, fully-equipped gyms and sports courts, and business centers or computer labs will likely cost more.
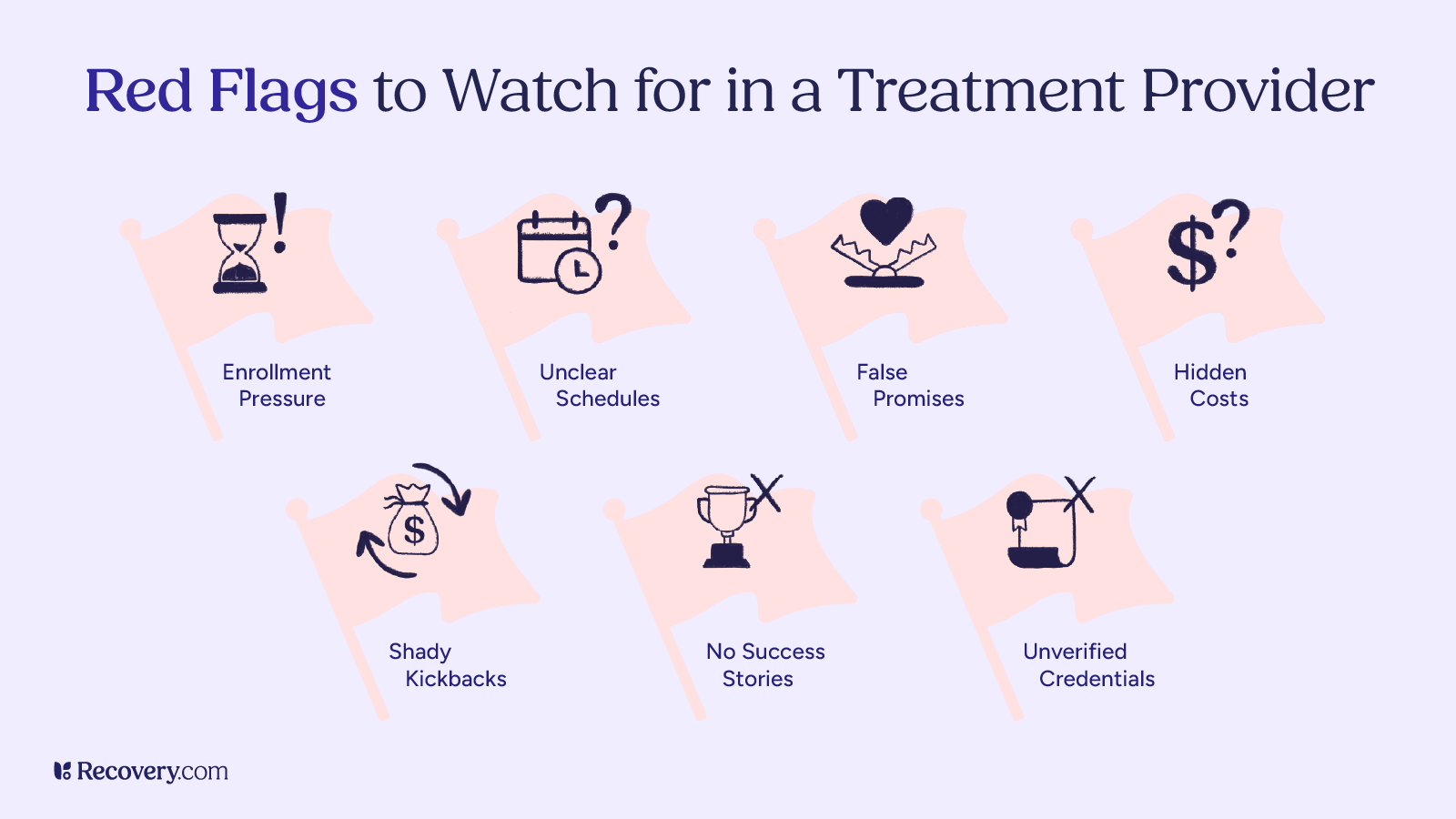
It’s important to remember that the cost of a treatment program doesn’t always correlate with the quality. In other words, just because you’re paying top dollar for a program doesn’t mean you’re necessarily getting the best treatment, and vice versa.
There are many factors to consider, other than cost, that can help you determine the quality of drug and alcohol treatment programs and facilities. If you’re interested in a particular location or facility, the best thing to do is to call and talk to their admissions team to learn more about any specific benefits, prices, and payment options.
Most clients at All Points North Lodge use insurance; “the rest either choose not to use it or don’t have it.”
3. Using Insurance to Pay for Addiction Treatment
Before you can use insurance to pay for addiction treatment, you need to know the following:
- Does your insurance plan cover the type of treatment you’re considering, and the level of care you’re wanting?
- Does the center you’re considering accept insurance?
Will My Insurance Cover Rehab Expenses?
Today in the U.S., most private health insurance policies do cover addiction treatment3 costs. In 2014, the Affordable Care Act (ACA) classified addiction and mental health treatment as essential health benefits,4 thus requiring insurance plans to cover treatment for alcohol addiction, drug addiction, and mental health conditions. This includes inpatient programs and outpatient rehab.
Even though having insurance may increase your opportunity to receive treatment, in 2018 only 13.4% of insured adults with a substance use disorder received treatment.5 Additionally, spending on substance abuse treatment6 is just 0.6% of overall private insurance spending.
Understanding what your insurance provider and plan covers can be difficult, but it’s essential to make sure you’re taking advantage of all of your insurance benefits. The best way to know if your insurance plan covers substance use treatment is to call and discuss your plan details with a customer service agent at your provider.
Which Alcohol and Addiction Rehabs Accept Insurance?
Since the ACA was passed, most US rehab centers will accept insurance in addition to offering multiple payment options. If this information isn’t listed on the center’s website, an admissions officer can give you those details when you call. Per Jerry Vaccaro, President of All Points North Lodge in Edwards, Colorado,
Because we’re in the U.S. and we’ve got the Affordable Care Act…the vast majority of people who come to us have insurance. Some choose not to use it for a variety of personal reasons. In the facility, I’d say at any one time, probably 70% to 75% of our clients have insurance and are using it and the rest either choose not to use it or don’t have it.
How Medicaid and Medicare Can Help Cover Treatment Costs
In the U.S., eligible recipients of Medicaid or Medicare can use these federal- and state-funded health insurance programs to also help pay for treatment.
Medicaid is free or low-cost health care for people who meet low-income requirements, whereas Medicare is a US federal health insurance program for adults over 65 or under 65 with a disability, regardless of income. As one report explains, “To more broadly cover uninsured individuals, the Affordable Care Act includes a provision that allows states to expand Medicaid coverage. Benefits include mental health and substance use disorder treatment services6 with coverage equivalent to that of general health care services.”
Each state has different eligibility rules and treatment coverage, which often change annually, and not all facilities accept Medicaid/Medicare as a form of payment.
What is the average cost of rehab?
The average cost of rehab varies widely depending on several factors, such as the type of treatment, location, duration, and whether the facility is inpatient or outpatient. Traditional inpatient stays can range from $5,000 on the lower end to upwards of $80,000 for a luxury site. Although options are more limited for those in financial need, Medicaid, Medicare, government grants, and various managed care (insurance) plans may be able to offset some or even all of the cost, allowing minimal to no charge for the patient.
Matthew Glowiak, PhD, LCPC, CAADC, ACS, NCC | Hazelden Betty Ford Graduate School
4. Paying For Rehab with Grants, Public Funds, and Scholarships
With or without insurance, you may still need additional funding to fully pay for treatment. As the U.S. Surgeon General’s 2016 report on addiction elaborates, although insurance coverage is critical for individuals with substance use disorders,6 “it is unlikely to cover all the services that such individuals may need, such as crisis services (e.g., emergency treatment intervention), housing, supported employment, and many community prevention programs and services (e.g., school-based prevention programs).”
There are public funds available through government organizations like the U.S. Department of Veterans Affairs, as well as grants from private institutions, like SAMHSA, and even scholarships from some rehab centers directly.
It’s historically documented that, in the U.S., state and local governments have been “the largest source of spending on substance use disorder treatment.”7 In 2009, excluding Medicaid expenses, their funds covered $7.6 billion—nearly a third—of total spending on substance use disorder treatment.
These forms of financial assistance to help pay for treatment are available because many institutions, including rehab centers themselves, recognize how vital treatment is and how financially beneficial it is for all of society for people to receive treatment.
“Although the United States spends roughly $35 billion across public and private payers to treat substance use disorders, the social and economic costs associated with these disorders are many times higher: Annual costs of substance misuse and substance use disorders in the United States are estimated at more than $400 billion,” according to the Surgeon General’s report. “Thus, treating substance use disorders has the potential for positive net economic benefits,6 not just in regard to treatment services but also general health care.”
To find out if a particular rehab center offers scholarships and how to apply for the reduced costs, contact the center directly. An admissions specialist can help you navigate the process of getting funding for treatment.
5. Additional Rehab Treatment Financing Options
If you don’t have insurance, or perhaps don’t want to use your insurance coverage for whatever reason, there are other payment options: financing directly from a treatment center, personal loans from family and friends, personal loans from a bank, or paying via credit card.
In general, the main goal of getting financing is to decrease or eliminate your out-of-pocket financial obligations. To that end, choosing a credit card or a loan with low interest rates and manageable payback terms may be preferable.
Some credit card companies offer deferred interest rates for medical-related expenses, including substance and mental health treatment. Furthermore, some centers offer financing options directly from their own funds or work with third-party lenders to create affordable loan packages.
Rehab can be a life-changing (and life-saving) experience, but it does often entail a sizable investment.
Disclaimer: Please note that it’s important to speak with your own financial advisor before taking action that will financially affect your future.
Using Your Own Money to Pay for Treatment
Another way to fund treatment is to self-pay using savings or other assets. In fact, this is one of the most common ways to pay for rehab. Do note that many rehab centers require full payment upfront. Alternatively, you can ask about any payment plan options such as putting down a deposit to secure your spot and then paying off your treatment in increments or monthly payments. Heather Charlet, Director of Admissions, explains the process at Gallus Detox Center in Colorado:
We can put clients on a bit of a payment plan to take a percentage of that upfront and then spread the rest of the payment out over several months. We then also work hard for the verification of benefits to be able to reimburse them as much as possible. We do everything we can to try to make it as cost-effective as possible.
Again, the best way to know what options your rehab center offers is to call them directly.
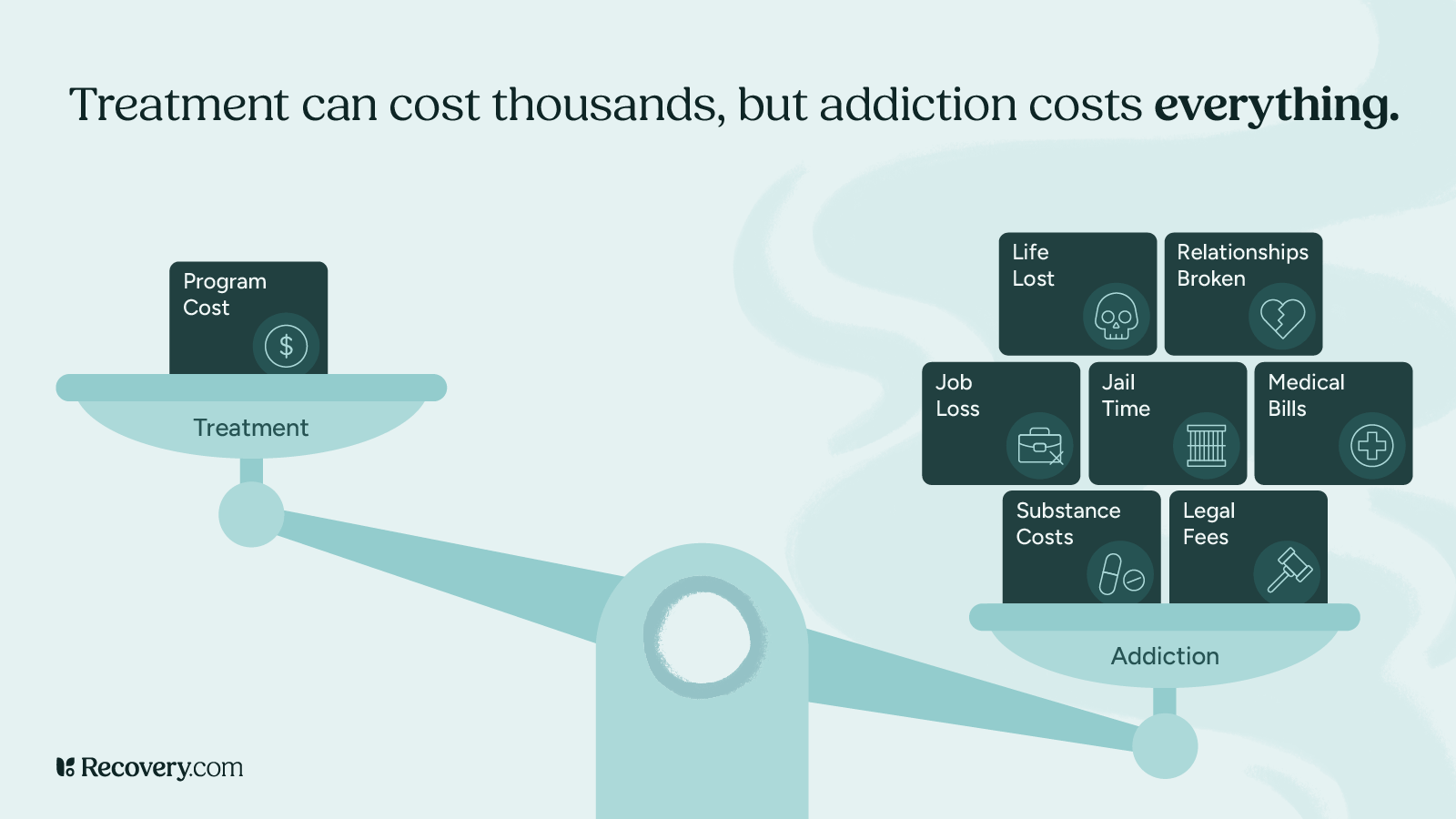
Is going to treatment or rehab worth it?
The answer requires careful consideration in terms of my commitment to recovery. Is going to treatment or rehab worth it, especially when considering the financial cost? Substance use invariably results in the loss of one’s identity. When we consider the impact of substances on one’s self-perception, the collateral damage, coupled with the onset of hopelessness, is going to treatment or rehab worth it? Yes, there’s no amount of money I wouldn’t spend to get my life back. The relevant question regarding the financial cost of treatment is, am I committed to the recovery process?
Charles Harris, CADC-II
6. Your Recovery is Worth the Cost of Rehab
No matter how much residential rehab may cost, it is worth it to get the help you need—both in the short term and in the long run. This isn’t just because treatment may save your life, but also because addressing your addictions or mental health conditions now can help reduce your total healthcare costs throughout your lifetime.
As the U.S. Surgeon General’s 2016 Report on Alcohol, Drugs, and Health describes, “Costs associated with substance use disorders6 are not limited to health care. The accumulated costs to the individual, the family, and the community are staggering and arise as a consequence of many direct and indirect effects, including compromised physical and mental health, loss of productivity, reduced quality of life, increased crime and violence, misuse, and neglect of children, and health care costs.”
When viewed from this perspective, you can see how the reduction in your future health care costs that are associated with treatment and recovery “would more than cover the cost of addiction treatment.”
We know the expense of inpatient treatment can seem intimidating at first. But, your financial concerns don’t have to be roadblocks on your path toward recovery. There are many different paths you can take to get the help you need, no matter what your budget or financial circumstances are.
See our collection of rehabs to find centers offering recovery programs in various price ranges, as well as those that accept insurance.
FAQs
Q: What are the price levels of addiction treatment?
A: Addiction treatment costs vary widely based on the type of care provided. Residential rehab can range from under $10,000 for basic programs to over $80,000 for luxury treatment. Outpatient programs are generally more affordable, with costs starting around $1,000 and going up to $10,000 or more for intensive care.
Q: What factors influence the cost of rehab?
A: Several factors affect the cost of addiction treatment, including:
- Type of treatment: Inpatient rehab is more expensive than outpatient programs.
- Program length: Longer stays (60 or 90 days) increase costs.
- Location: Treatment centers in high-demand areas (beachfront or mountain retreats) may cost more.
- Services offered: Medical detox, therapy, and holistic treatments can add to the cost.
- Amenities: Luxury facilities with private rooms, pools, or gourmet meals tend to be pricier.
Q: Does insurance cover addiction treatment?
A: Yes, most private insurance plans cover addiction treatment, including inpatient rehab, outpatient care, and detox. Thanks to the Affordable Care Act (ACA), substance use treatment is considered an essential health benefit. However, coverage varies by provider, so it’s important to verify your benefits with your insurance company.
Q: How can I use Medicaid or Medicare to pay for rehab?
A: Medicaid and Medicare both provide coverage for addiction treatment, but eligibility and services covered vary by state. Medicaid is for low-income individuals, while Medicare is for adults 65+ or those with disabilities. Some rehab centers accept both programs, so it’s best to check directly with facilities or visit Recovery.com to find covered providers.
Q: Are there grants or public funds available to help pay for rehab?
A: Yes, several options can help cover rehab costs:
- State-funded rehab programs: Many states offer low-cost or free treatment for qualifying residents.
- Scholarships from rehab centers: Some private facilities offer financial assistance to those in need.
Q: What financing options are available for rehab?
A: If you don’t have insurance or need additional financial support, you may consider:
- Payment plans: Many rehab centers offer flexible monthly payments.
- Medical loans: Specialized loans for healthcare expenses.
- Credit cards: Some credit cards provide deferred interest for medical expenses.
- Personal savings or family contributions: Self-paying is also an option for some individuals.
Q: Is rehab worth the cost?
A: Absolutely. While rehab can be a significant expense, not seeking treatment often leads to much higher costs, including medical bills, lost income, legal issues, and long-term health complications. Research from the National Institute on Drug Abuse (NIDA) shows that every $1 spent on addiction treatment saves up to $12 in healthcare and social costs.
Q: How do I find an affordable rehab center?
A: You can find cost-effective treatment by:
- Checking insurance-covered rehab facilities.
- Looking for state-funded or nonprofit programs.
- Asking about sliding scale payment options at private centers.
- Applying for scholarships or grants offered by treatment facilities.
If you’re ready to start treatment, reach out to a rehab center’s admissions team to discuss your financial options and find a solution that works for you.