Sober living environments (SLEs)1 provide group housing for individuals recovering from substance use disorders.
These living spaces, also known as sober living homes, halfway houses, or recovery residences, create a structured and supportive atmosphere that helps residents’ transition back into everyday life after completing rehabilitation programs.
Sober living homes are designed to help individuals maintain sobriety by addressing the people, places, and things in their environment. These homes provide a structured setting1 that promotes accountability, peer support, and essential life skills. Below are seven key features that make sober living effective:

1. Substance-Free Environment
Residents must remain abstinent from drugs and alcohol while living in a sober home. This rule allows individuals to recover in a safe space free from triggers. Eliminating access to substances makes relapse more difficult, giving residents the opportunity to focus on their sobriety and coping strategies. Oftentimes, depending on the type of sober living, drug testing may be a part of accountability and maintaining a drug-free environment.
2. House Rules and Accountability
A lack of accountability is a common trait in addiction. Sober living homes enforce specific house rules, such as curfews, mandatory house meetings, and assigned chores, to instill discipline and responsibility. House managers oversee rule enforcement, ensuring everyone stays on track and remains accountable to themselves and their housemates. This can also include monitoring of activities and schedules, support systems, and even testing for drug use.
3. Support System and Peer Encouragement
Residents benefit from a built-in community of individuals2 who are also in recovery. Living with peers who share similar struggles fosters mutual support, encouragement, and accountability. This social reinforcement helps combat feelings of isolation and strengthens one’s commitment to sobriety. Some sober living homes require 12-step meetings or other types of peer support or social support.
How does sober living support long-term, sustained recovery?
Recovery housing can solidify someone’s journey in their recovery either post-treatment or while someone is attending treatment in an outpatient setting. Recovery housing ideally provides support, structure, community, accountability, and responsibility. Although many people choose not to go into recovery housing and can maintain successful recovery, the relationships and foundation that recovery housing can provide can be invaluable as a contribution to long-term success.
Tanya Kraege LCSW, CSAC, CCAR RC, WI CPS | Ventus Rex
4. Structured Daily Routine
Sober living environments3 emphasize the importance of structure. Residents follow daily routines that may include attending therapy sessions, support groups, exercising, and completing household chores. Establishing a consistent schedule helps individuals develop positive habits and reduce the time spent thinking about substance use. One of the main benefits of sober living is having structure as a next step after more formalized treatment or recovery programs.
5. Transition Assistance and Life Skills Training
Sober living homes often provide life skills training to help residents reintegrate into society. Programs may include budgeting, job searching, cooking, and relationship-building skills. These resources equip individuals with the tools needed to maintain independence and sustain long-term recovery. Depending on the level of care provided in the home, there may be additional options available for life skills or other educational opportunities.
6. Connection to Recovery Resources
Many sober living homes offer access to additional support services, such as therapy, job placement programs, and educational opportunities. These resources help residents continue their recovery journey beyond the sober living environment, ensuring they have the tools to maintain sobriety in everyday life.
7. Affordable Housing Options
Sober living costs vary depending on location, services, and amenities. Monthly expenses typically range from $300 to $2,000. Many homes operate on a sliding scale or offer financial assistance for those in need, making sober living an accessible option for individuals from different financial backgrounds. Some homes are credentialed and some operate like the Oxford House4 model.
Optimizing the Recovery Experience
Addiction impacts all aspects of a person’s life, requiring a holistic approach to recovery. For individuals with severe substance use disorders or co-occurring mental health conditions, sober living can provide a stable and supportive environment while they continue treatment. Programs such as cognitive behavioral therapy (CBT) and dialectical behavioral therapy (DBT) can help address both addiction and underlying mental health issues, improving overall well-being.
Here are some additional types of recovery support services along a path to sobriety and wellness.
How does sober living differ from traditional rehab?
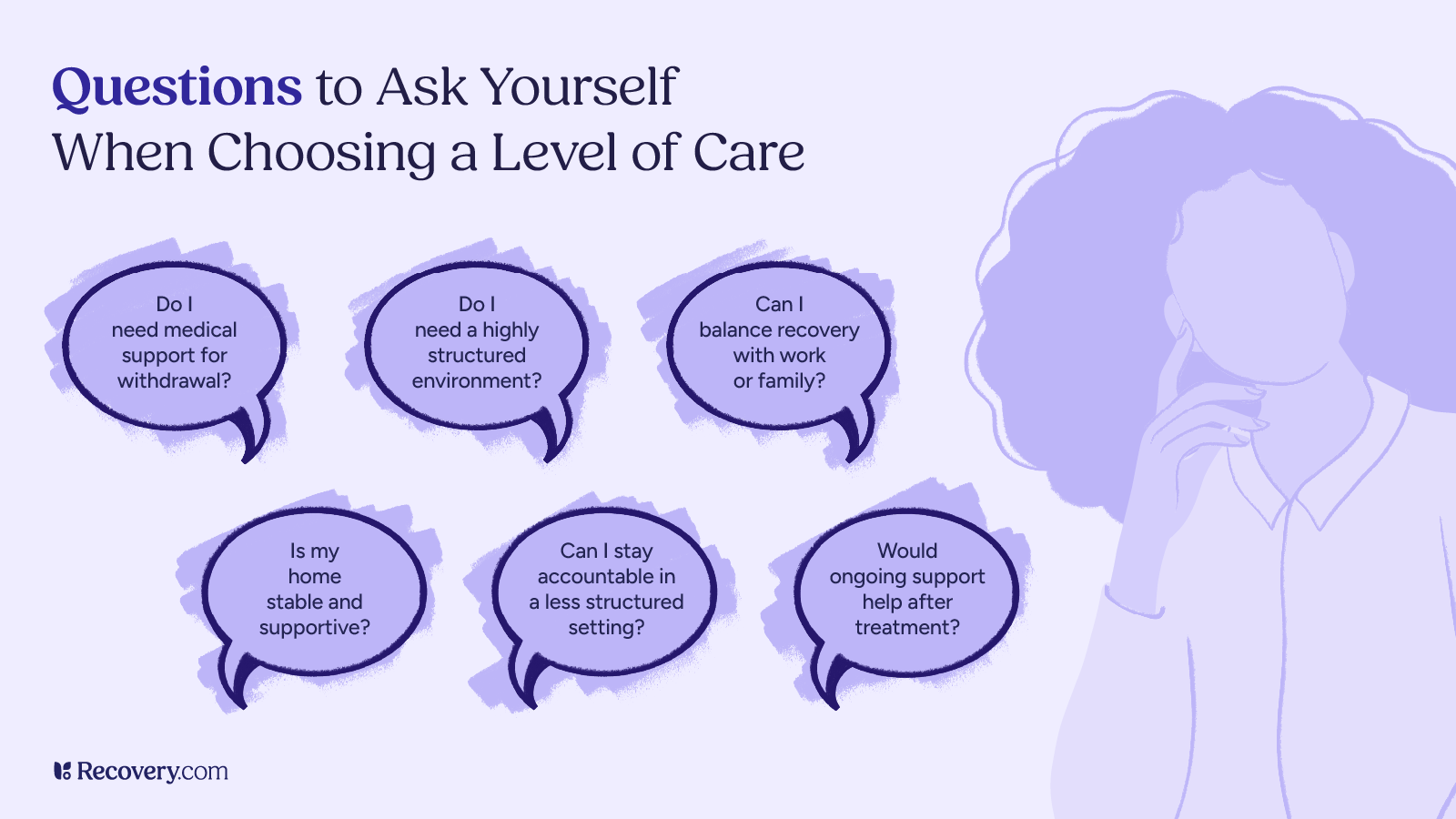
Sober living offers a structured, substance-free environment where individuals can gradually transition back into daily life, often with fewer restrictions than traditional rehab. Traditional rehab, on the other hand, is typically more intensive with structured treatment programs, licensed therapy, other behavioral services, and medical supervision.
Andrew J. Schreier, ICS, CSAC, LPC, ICGC-II, BACC
Treatment Programs: A Path to Sobriety
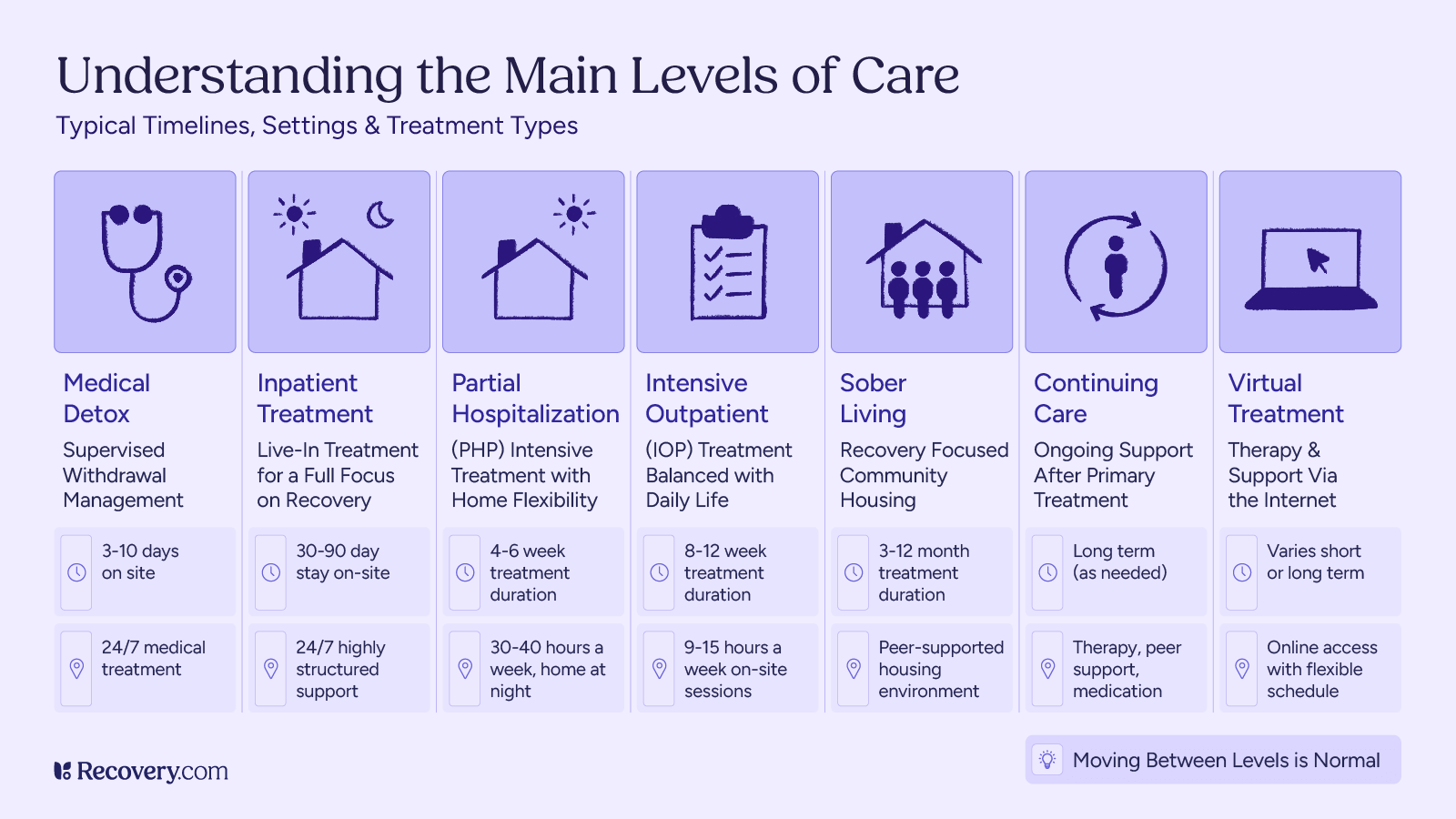
Addiction treatment programs provide structured support to help individuals achieve long-term recovery. These programs vary in intensity and approach but generally include the following components:
- Assessment and Evaluation: Before beginning treatment, individuals undergo a comprehensive assessment to determine the severity of their addiction, identify co-occurring mental health disorders, and develop a personalized treatment plan.
- Detoxification: Detox is a critical first step in recovery. Medically supervised detox programs help individuals safely withdraw from substances while managing withdrawal symptoms. This step is especially important for individuals detoxing from opioids, benzodiazepines, or alcohol, as withdrawal can be life-threatening.
- Inpatient Treatment: Inpatient programs provide 24/7 care in a structured environment. Treatment typically includes individual therapy, group counseling, behavioral therapy, and holistic approaches. This immersive setting allows individuals to focus entirely on their recovery.
- Outpatient Treatment: Outpatient programs offer flexibility for individuals who can maintain independent living while attending scheduled therapy and support sessions. This option is ideal for those with a stable home environment and strong support system.
- Aftercare Planning: Long-term recovery requires ongoing effort. Aftercare planning includes continued therapy, support groups, and recovery resources to help individuals transition back into daily life while maintaining sobriety.
- Support Groups: Participation in 12-step programs, such as Alcoholics Anonymous (AA) or Narcotics Anonymous (NA), provides peer support, accountability, and encouragement from others who understand the challenges of addiction.
Bridging the Gap: Integrating Sober Living with Treatment
Sober living homes serve as a vital link between inpatient treatment and full independence. By combining structured treatment with sober living, individuals receive comprehensive support that enhances their recovery journey. This approach fosters long-term sobriety, equipping individuals with the tools and resources needed to reintegrate successfully into society.
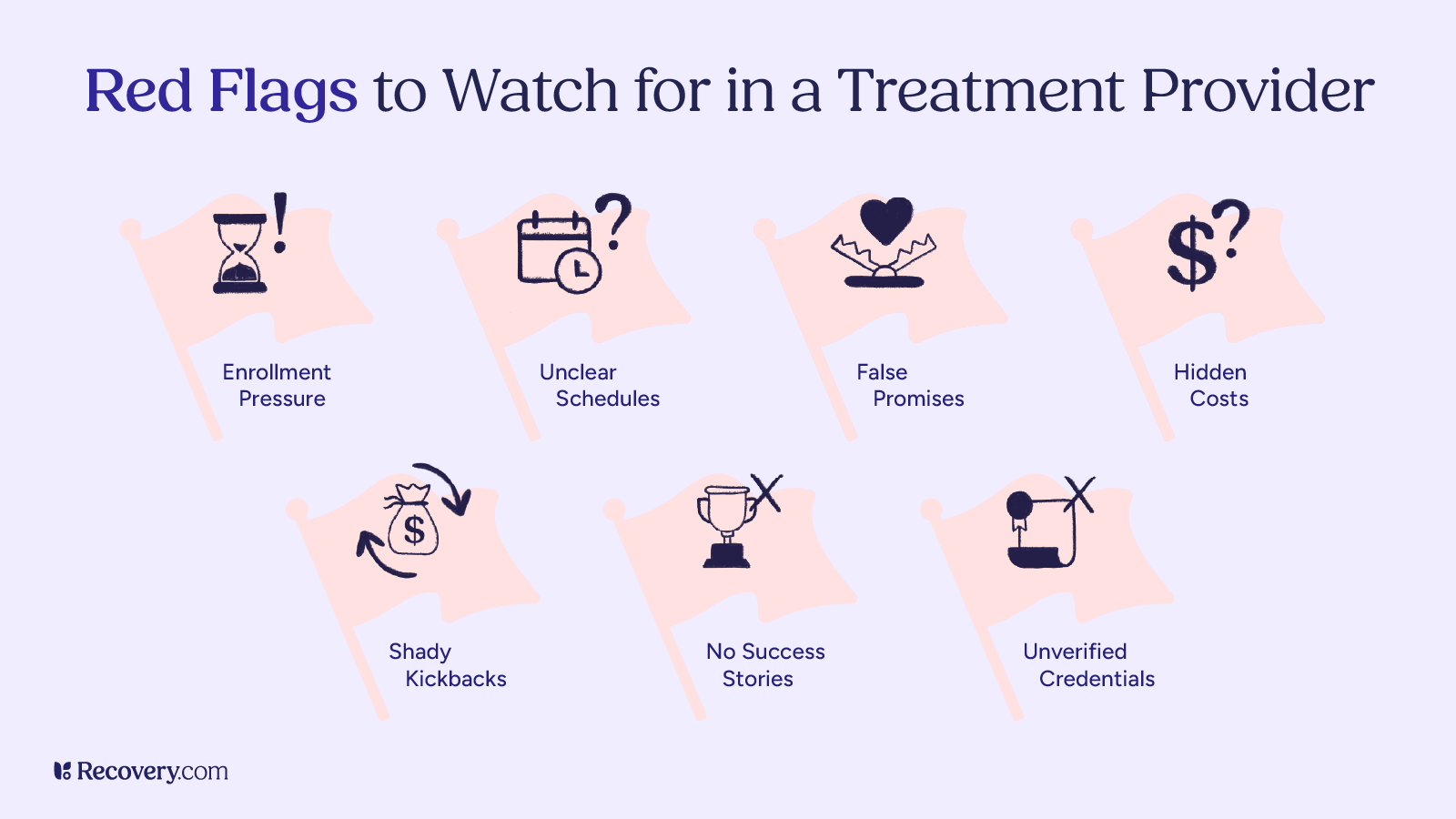
If you or a loved one are seeking the best sober living environment, consider researching reputable options to find the right fit for your recovery needs.
If you or a loved one are seeking the best sober living environment, please consider one of the following that come highly recommended:
If you or a loved one are seeking the best sober living environment, consider ARC Stone Lodge in Louisa, Kentucky, which provides a structured, supportive setting for recovery. The Southeast Addiction Center, with locations in Georgia and Tennessee, offers comprehensive addiction treatment alongside sober living options. The Pennsylvania Recovery Center in Phoenixville, Pennsylvania, is another highly regarded facility for those in need of a supportive transition.
For young men seeking specialized sober living, Sandstone Care Young Men’s Sober Living in Maryland provides tailored support. The Massachusetts Center for Addiction in Weymouth, Massachusetts, also offers structured sober living programs designed for long-term recovery. Additionally, Lantana Recovery Connecticut in New Milford provides a supportive recovery-focused community for individuals seeking a sober lifestyle.
For a broader list of recommended sober living homes that match individual recovery needs, check out the comprehensive sober living directory for more options.
This version integrates the recommended facilities smoothly within the text while keeping it natural and informative. Let me know if you need any further tweaks!
Frequently Asked Questions
Q: What is the meaning of sober living?
A: Sober living refers to a structured, substance-free environment that supports individuals in recovery from addiction. It provides a safe space where residents can rebuild their lives and develop the skills needed for long-term sobriety.
Q: What do you do in sober living?
A: In a sober living home, residents follow house rules, attend recovery meetings, engage in therapy or counseling, complete household chores, and develop essential life skills to maintain independence and sobriety.
Q: How long do most people stay in sober living?
A: The length of stay varies based on individual needs, but most residents stay between 90 days and a year. Some may stay longer if they require extended support before transitioning to independent living.
Q: What does it mean to live a sober life?
A: Living a sober life means abstaining from drugs and alcohol while actively engaging in healthy behaviors, relationships, and coping strategies. It involves maintaining mental, physical, and emotional well-being without substance use.
Q: What is a sober living home?
A: A sober living home is a residential facility that provides a drug- and alcohol-free environment for individuals in recovery. It offers structure, accountability, and peer support to help residents transition from rehab to independent living.
Q: What are sober living house rules?
A: Sober living homes enforce house rules such as maintaining sobriety, attending meetings, adhering to curfews, completing assigned chores, and participating in house meetings. These rules help create a structured and supportive environment.
Q: What is a halfway house?
A: A halfway house is a transitional residence for individuals recovering from addiction or leaving incarceration. It provides temporary housing with structured programs, support services, and supervision to help residents reintegrate into society.
Q: Are you covered for addiction treatment?
A: Insurance coverage for addiction treatment, including sober living, varies by provider and policy. It’s essential to check with your insurance company to determine coverage for treatment, therapy, or transitional housing programs.
Q: Does the sober living home you are considering provide access to mental health resources and community support?
A: Many sober living homes offer access to therapy, counseling, peer support groups, job assistance, and other mental health resources. It’s important to research a home’s available services to ensure they align with your recovery needs.
Q: What are halfway house rules?
A: Halfway houses typically have structured rules, including mandatory sobriety, curfews, participation in treatment programs, job search requirements, and adherence to behavioral guidelines. These rules help residents transition back into society successfully.
Q: How does sober living support recovery from addiction?
A: Sober living homes provide a stable, substance-free environment where residents receive peer support, structure, and access to recovery resources. This setting helps individuals build coping skills, accountability, and a strong foundation for lasting sobriety.
Q: How does sober living differ from traditional rehab?
A: Unlike inpatient rehab, which offers intensive treatment in a clinical setting, sober living provides a less restrictive, transitional environment where residents can practice independent living while still receiving recovery support.
Q: How does sober living help in addiction recovery?
A: Sober living homes foster long-term recovery by reinforcing healthy routines, peer support, and access to therapy and life skills training. They help individuals build resilience, stability, and self-sufficiency after rehab.