Life isn’t happening to you; it’s just happening. This profound realization, shared by Kori Leigh, a writer, recovery mentor, and host of The Kori Leigh Show podcast, is a cornerstone of her recovery journey. She challenges the common notion that life’s hardships are a personal attack, instead reframing them as neutral events to be navigated. In a powerful conversation on Recoverycast, Kori shared her story of navigating profound childhood trauma, a destructive battle with addiction, and the eventual surrender that led to a life of purpose and faith.
Before she reached sobriety in 2016, Kori’s life was a maelstrom of rage, self-hatred, and chaotic substance use, all stemming from a traumatic childhood. Her narrative isn’t just about overcoming addiction; it’s a testament to the resilience of the human spirit and the transformative power of a 12-step recovery program. Kori’s story is a raw and honest look at how unresolved trauma can fuel addiction and how the painful process of facing one’s past is the only way to build a future worth living.
1. Childhood Trauma as a Catalyst
From a young age, Kori’s world was marked by loss and emotional turmoil. Her older brother died from a heart condition when she was an infant, and her father passed away from a brain aneurysm when she was six years old. The trauma of losing her father, a man she adored, left a deep, indelible mark on her psyche. As a child, she struggled to comprehend the arbitrary nature of his death and developed a deep-seated hatred for God and a profound distrust of life itself.
“I hated God for taking my dad,” Kori shared. This anger became her primary coping mechanism, manifesting as rage, resentment, and a feeling of being abandoned by the very fabric of existence. This early trauma set the stage for a lifetime of seeking escape, a pattern that would later lead her down the path of addiction. The sudden, unexplained loss shattered her sense of safety and made her feel like a “puppy that had fallen off the back of the truck,” left to fend for herself in a world that seemed inherently hostile.
2. The Illusion of Control: The “Perfect” Double Life
Throughout her addiction, Kori maintained a facade of success and normalcy. She was a personal trainer, a marathon runner, and an author. She built a life that, from the outside, appeared to be thriving. This is a classic hallmark of high-functioning addiction—the ability to hide the chaos and destruction behind a veneer of accomplishment. For Kori, her athletic achievements and professional success were not sources of pride but rather tools for denial.
“No one can tell with me,” she stated, reflecting on her ability to mask her struggles. She believed that her outward success was proof that she didn’t have a problem, an idea that many people with substance use disorders cling to. This double life was a way to manage the intense shame and self-hatred that festered beneath the surface. It was a vicious cycle of self-harm, emotional chaos, and intense self-criticism.
This dual existence is a common theme in the lives of high-functioning addicts. They often excel in their careers, maintain social relationships, and engage in physically demanding activities, all while battling a severe addiction in secret. The shame and fear of exposure drive them to work even harder to maintain the illusion of control, making it incredibly difficult for loved ones to recognize the problem. The facade crumbles only when the addiction becomes so severe that it can no longer be hidden.
Explore alcohol addiction treatment centers.
3. The Onset of Addiction: “I Was a Blackout Party Girl”
Kori’s substance use began in her teens, but it didn’t escalate into full-blown addiction until her mid-twenties. Her drug of choice wasn’t a daily habit but a weekend-long bender, a pattern of “blackout party girl” drinking that she believed absolved her of having a problem.
“I always thought an addict, an alcoholic was like daily. They drank in the morning, they drank like warm, cheap beer under a bridge,” Kori explained, highlighting a common misconception about alcoholism. “I was like a blackout party girl on the weekend, but my weekend was like Thursday to Sunday.”
This pattern of binge drinking, despite not being a daily habit, is a dangerous form of addiction that can cause significant physical and mental health issues. It’s a form of high-risk drinking that can lead to alcohol poisoning, accidents, and a host of long-term health problems.
Kori’s story is a powerful reminder that addiction doesn’t always fit the stereotypical mold. It can be a series of blackouts, a cycle of shame and denial, and a desperate attempt to escape from an inner world of pain and self-loathing. The chaotic lifestyle, losing her car, and the constant fear of what she had done the night before became her new normal.
4. The Rock Bottom: A Spiritual Breaking Point
The path to recovery often begins with a moment of profound crisis, a “rock bottom” where the illusion of control shatters completely. For Kori, this moment was not a single event but a slow, agonizing slide into a level of darkness she could no longer ignore. After a series of destructive relationships fueled by substance use, she found herself in a place of extreme anxiety, depression, and self-harm.
She had a moment of clarity while sitting in a bathtub, fully clothed and without water, where she swore off God. She believes this moment opened a “portal of darkness” that led to a period of severe spiritual and emotional turmoil.
The final descent into recovery came after a period of self-harm and insomnia. She decided to do a “cleanse” from alcohol, a final attempt to regain control. After a brief period of sobriety, she tried to reintroduce alcohol into her life, only to find the darkness returning with a vengeance. She had hit her breaking point.
5. Surrender and the Daily Practice of Recovery
The journey to recovery for Kori was a painful process of surrender. It wasn’t just about giving up alcohol but about surrendering the false narrative she had lived by for so long. She had to face the difficult truth that her life was unmanageable and that she was powerless over her addiction. This admission, she says, was the first step toward true freedom.
She emphasizes that recovery is not a one-time event but a daily practice. It’s about “playing the tape through,” considering the long-term consequences of her actions instead of seeking instant gratification. This is a core principle of 12-step programs, which emphasize the importance of making amends, seeking a spiritual connection, and helping others. For Kori, this meant embracing a life of purpose and faith after a lifetime of feeling disconnected.
“The flip side of recovery is so good,” Kori said, challenging the common misconception that sobriety is a “killjoy” of all fun. “It’s not just a bit better; it’s an entirely different existence.”
Her story is a powerful testament to the idea that recovery is not just about abstaining from a substance but about building a new life, one of meaning, purpose, and genuine connection.
6. The Long Road to Healing: Shame and Forgiveness
Even after achieving sobriety, Kori had to confront the immense shame she carried from her past. The memories of her blackout nights, the lost car, and the destructive behaviors were not erased by her new way of life. She had to work through the shame and forgive herself for the person she was.
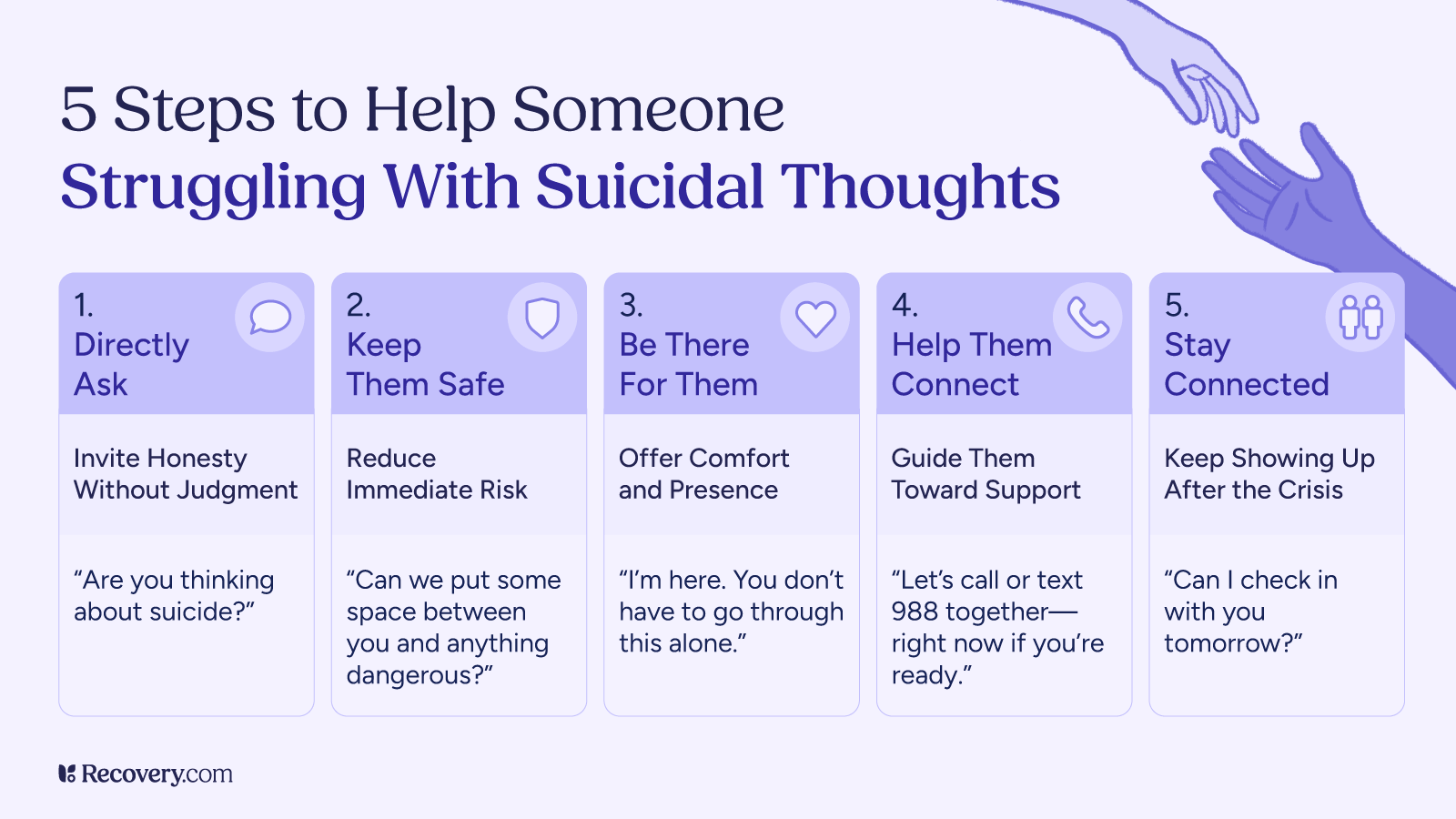
“There’s a lot of shame,” Kori admitted. “I’m not gonna come out and tell people…my best-laid plan is like, oh, I’ll kill myself if this doesn’t work out.”
The shame associated with addiction can be a major barrier to seeking help and maintaining recovery. It keeps individuals isolated and unable to share their struggles. For Kori, it took years of therapy and recovery work to process the shame and understand that her destructive behavior was a symptom of a deeper problem.
The journey to self-forgiveness is an essential part of the recovery process. It involves acknowledging the past without judgment and accepting that addiction is a disease, not a moral failing.
7. The Role of Faith and a Higher Power
A central theme in Kori’s story is her evolving relationship with a higher power. After years of hating God for the trauma she endured, she found a spiritual connection through recovery. She had to learn to trust again, not just herself but a force greater than her own will.
“I hated God, and I didn’t trust God,” she said, recounting her childhood rage. However, when she was at her lowest point, she “prayed to a God that I didn’t believe in,” which led her to a therapist and, eventually, the path of recovery.
This spiritual journey is a core component of many recovery programs. It’s not about embracing a specific religion but about finding a power greater than oneself to help overcome addiction. For Kori, this meant learning that life is not happening to her but is a neutral experience that she can navigate with faith and trust.
8. A New Purpose: Helping Others in Recovery
Today, Kori uses her story and her platform to help others. As a writer, recovery mentor, and podcast host, she shares her experiences to inspire hope and show others that a life in recovery is not only possible but incredibly fulfilling. Her podcast, The Kori Leigh Show, is a space where she continues to explore the themes of healing, faith, and purpose.
The act of helping others is a powerful tool for maintaining recovery. It allows individuals to turn their past pain into a source of strength and meaning. It’s a way of making amends for the past and contributing to the well-being of others.
The journey from a “blackout party girl” to a recovery advocate is a testament to the transformative power of a 12-step program and the courage to face one’s deepest fears. Kori’s story is a beacon of hope for anyone struggling with addiction, proving that a life of chaos can be replaced with one of grace, purpose, and genuine connection.