The best therapy for you isn’t necessarily the most popular one—it’s the approach that matches your specific needs, goals, and circumstances. Understanding your treatment options can help you make an informed decision about your mental health care, no matter what challenges you’re facing.
Let’s explore these therapies so you can find the best treatment for you.
Commonly Used Therapies in Addiction and Mental Health Treatment
Some of the most common therapies include:
Cognitive Behavioral Therapy (CBT)
CBT is one of the most widely researched and effective1 forms of therapy available today. It focuses on challenging and reframing negative (and often untrue) thoughts, using thought corrections and helpful behaviors to positively affect your emotional state.
Core Focus
- Challenging and reframing negative (and often untrue) thoughts
- Using thought corrections and helpful behaviors to positively affect your emotional state
Typically Used For
- Depression
- Anxiety disorders
- Trauma
- Suicidality
- Eating disorders
- Substance use disorders
Structure and Format
- Time-limited and goal-oriented: typically 10–20 sessions
- Session length depends on condition severity, insurance coverage, and recovery progression
- Structured sessions include agenda-setting, skill practice, review, and homework planning
Special Features
- Collaborative: clients are co-investigators, not passive recipients
- Includes homework between therapy sessions
- Uses behavior-analyzing exercises, behavior tracking, and worksheets
- Widely effective across multiple mental health conditions
CBT’s structured approach makes it helpful for people who prefer clear goals and measurable progress in their treatment.
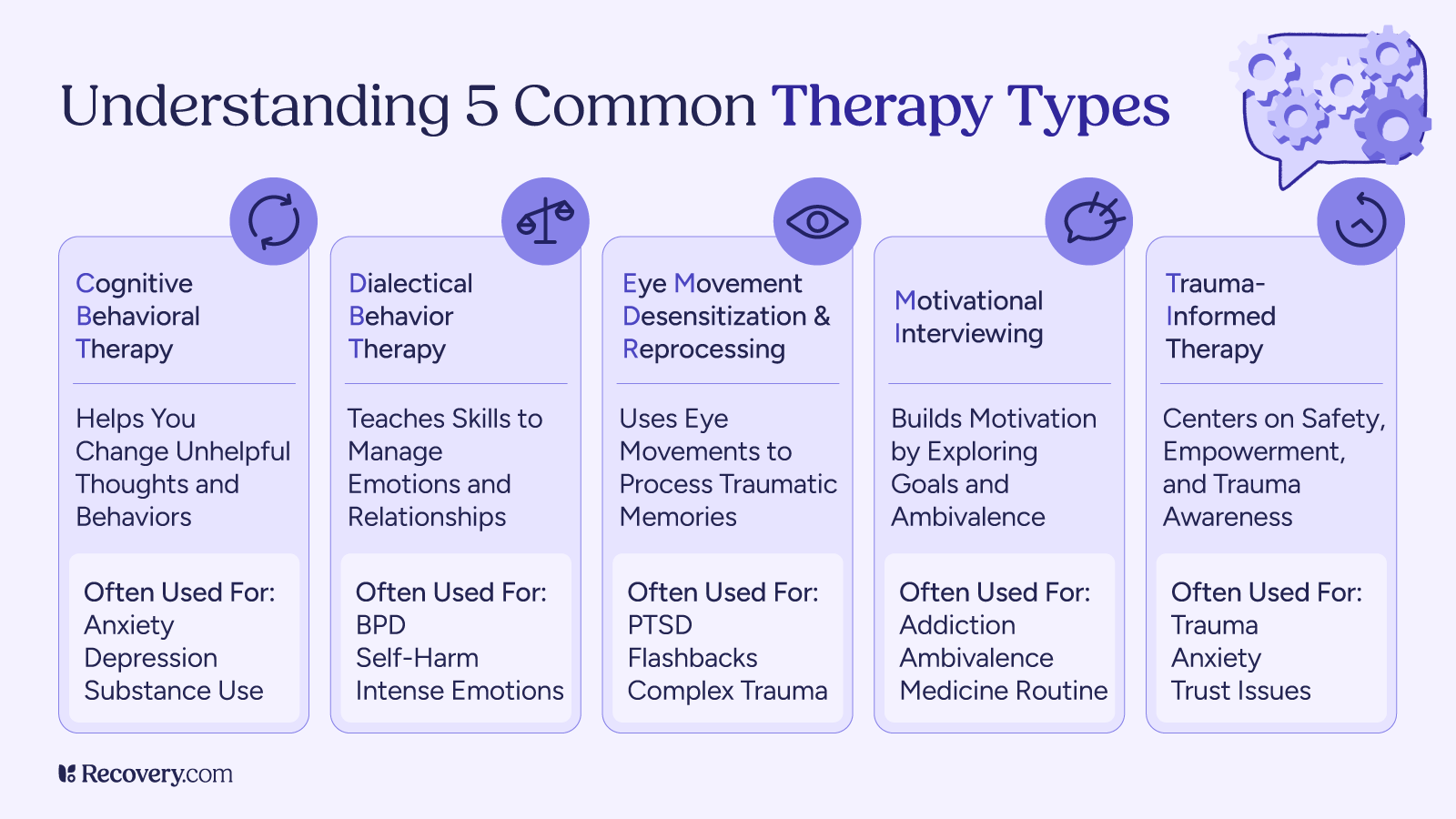
Dialectical Behavioral Therapy (DBT)
DBT centers on being mindful of your thoughts, emotions, and feelings. It’s effective for both mental health problems and substance misuse. DBT was originally created to help people with borderline personality disorder (BPD)2 but has since been used to address mental illness more broadly, focusing on practical skills for communication, emotional regulation, and navigating crises.
Core Focus
- Being mindful of your thoughts, emotions, and feelings
- Teaching practical skills for communication, emotional regulation, and crisis navigation
- Balancing acceptance and change strategies
Typically Used For
- Mental health concerns
- Borderline personality disorder (BPD)
- Substance misuse (mindfulness techniques can help you manage cravings)
- Self-harming behaviors
- Emotional dysregulation
Structure and Format
Pretreatment (commitment phase): Build motivation and commitment to treatment, orient to DBT principles, and agree on goals
Individual therapy (weekly): Attend one-on-one sessions that focus on your specific challenges, issues that get in the way of treatment, and problems that impact your daily life, using techniques to understand behavior patterns and provide emotional support
Group skills training (weekly): Learn 4 core skill modules in a classroom format:
- Mindfulness
- Distress tolerance (crisis survival skills like TIPP, distraction, and radical acceptance)
- Emotion regulation (understand emotions, reduce vulnerability with ABC PLEASE, build positive experiences)
- Interpersonal effectiveness (ask for needs, say no, maintain self-respect using DEAR MAN, GIVE, FAST)
Phone coaching (as needed): Hold calls with your therapist between sessions for real-time skill coaching in challenging moments
Learn more about these skills and more in our article on what to expect in DBT.
Special Features
- Combines individual and group therapy components
- In-the-moment crisis coaching and skill support
- Emphasizes both acceptance and change
- 4 core skill modules
DBT’s comprehensive approach makes it effective for people who experience intense emotions and need both individual support and community practice.
Eye Movement Desensitization and Reprocessing (EMDR)
EMDR is highly effective for trauma and post-traumatic stress disorder (PTSD),3 as it helps your brain reorganize traumatic memories using bilateral stimulation (like looking left-to-right). The act of tracking an object back and forth, or being touched on your left and right side, allows your brain to recall and process traumatic memories without such strong emotional reactions.
Core Focus
- Processing traumatic memories using bilateral stimulation
- Reducing the emotional intensity of traumatic memories
- Helping the brain naturally heal from psychological trauma
Typically Used For
- Post-traumatic stress disorder (PTSD)
- Trauma and acute stress reactions
- Anxiety disorders related to trauma
- Phobias
- Grief and loss
Structure and Format
- Typically 6–12 sessions for significant improvement
- Sessions involve bilateral stimulation (eye movements, tactile, or auditory)
- Structured, 8-phase protocol4
- Mental health professionals require specialized EMDR training
Special Features
- Does not require detailed discussion of traumatic events
- Can produce profound changes in relatively few sessions
- Uses the brain’s natural healing processes
- Bilateral stimulation helps integrate traumatic memories
- Designed to make trauma processing as comfortable as possible
EMDR’s unique approach makes it helpful for people who want to process trauma without extensive talk therapy or who haven’t found relief through other methods.
Motivational Interviewing (MI)
Motivational interviewing, or MI, is a technique used in talk therapy to motivate someone to change, and then to stay committed to the process. It helps you keep your goals in sight, remember how far you’ve come, and offers inspiration to keep pushing forward in your recovery journey.
Core Focus
- Motivating you to make changes and stay committed to the process
- Exploring and resolving ambivalence about change
- Strengthening personal motivation and commitment to your goals
Typically Used For
- Substance use recovery
- Chronic mental health conditions
- Medication adherence challenges5
- Behavioral changes (diet, exercise, lifestyle)
- Treatment engagement issues
Structure and Format
- Can be used as a standalone therapy or integrated with other approaches
- Collaborative, person-centered conversations
- Focuses on your own motivations rather than external pressure
- Session length varies depending on the treatment setting
Special Features
- Helps with medication adherence (continuing treatment even when motivation wanes)
- Effective for medication-assisted treatments6 such as methadone and buprenorphine
- Useful for both addiction and mental health recovery
- Non-confrontational approach that meets patients where they are
- Emphasizes autonomy and personal choice
MI’s collaborative approach makes it helpful for people who feel uncertain about change or have struggled to stick with treatment in the past.
Trauma-Informed Therapy
Trauma-informed therapy7 means the content and setting have been adapted specifically to trauma, and that the therapist is trauma-literate. It acknowledges the pervasive effects of trauma and aims to create a space of safety where you can begin to share your experience with a highly compassionate, competent therapist.
Core Focus
- Creating a safe, supportive therapeutic environment
- Acknowledging the widespread impact of trauma
- Adapting treatment approaches to be sensitive to trauma history
Typically Used For
- All types of trauma (childhood, adult, complex trauma)
- PTSD and trauma-related symptoms
- Anyone with a history of traumatic experiences
- Co-occurring trauma and substance use disorders
- People who’ve had negative therapy experiences
Structure and Format
- Can be integrated into various therapeutic modalities
- Emphasizes safety, trustworthiness, and collaboration
- Flexible pacing based on your comfort and readiness
- Therapist requires specialized trauma training and competency
Special Features
- Prioritizes physical and emotional safety above all else
- Recognizes trauma symptoms as adaptive responses
- Avoids re-traumatization through careful approach
- Emphasizes patient choice, control, and empowerment
- Addresses cultural, historical, and gender-based trauma
Trauma-informed therapy’s safety-first approach makes it essential for anyone whose past experiences may impact their ability to engage in traditional therapeutic settings.
Finding the Right Therapy for Your Needs
What you need help with often determines which therapy will meet your needs. Here’s how different therapies align with specific mental health conditions and concerns.
Depression
In psychotherapy for depression, CBT is often the first choice.8 CBT targets thoughts, emotions, and behaviors, directly addressing the cyclical nature of depression. DBT is also effective for depression9 as it teaches distress tolerance skills and opposite action, which means doing the opposite of an unhelpful behavior—like isolating or ruminating—to end the cycle.
Other therapies that are effective for depression include:
- Interpersonal therapy (IPT)
- Behavioral activation (BA)
- Acceptance and commitment therapy (ACT)
- Mindfulness-based cognitive therapy (MBCT)
- Psychodynamic therapy
- Transcranial magnetic stimulation (TMS)
Anxiety
CBT can be highly effective for anxiety, too. Specifically, the thought-challenging aspect of CBT can help with catastrophizing (thinking the worst possible thing will happen), emotional reasoning (I feel this way, which makes it true), and mind reading (assuming others’ thoughts).
Exposure and response prevention (ERP) is a first-line treatment for obsessive-compulsive disorder (OCD).10 It works by exposing you to something that triggers a compulsion or anxiety, and then you practice not following the compulsion or sitting with anxiety until it passes. This gradually reduces the anxiety these situations cause until they become less distressing and more manageable. Exposure-based strategies are also used to treat other anxiety disorders, like social anxiety and phobias.
Other therapies commonly used to treat anxiety include:
- Acceptance and commitment therapy (ACT)
- Mindfulness-based stress reduction (MBSR)
- Mindfulness-based cognitive therapy (MBCT)
- Dialectical behavior therapy (DBT)
- Psychodynamic therapy
- Interpersonal therapy (IPT)
- EMDR (especially when anxiety is trauma-related)
- Virtual reality exposure therapy (for phobias, social anxiety, and PTSD)
Addiction
Many therapies can help with substance use disorders, and treatment can be tailored based on underlying factors like trauma, grief, or co-occurring mental health conditions like depression.
Therapies like CBT, DBT, and EMDR can address root causes and help you develop healthier coping skills. These approaches are especially helpful for co-occurring disorders, when someone has both a substance use disorder and a mental health condition at the same time.
Evidence-based treatments include (but aren’t limited to):
- Medication-assisted treatment (MAT)
- Contingency management
- Motivational interviewing
Peer support approaches like the 12 Steps of AA provide community support, spiritual principles, and structured recovery steps. These programs involve regular meetings, working with sponsors, and service to others in recovery.
Harm reduction strategies meet people where they are, focusing on reducing risks and improving safety rather than requiring immediate abstinence. This approach recognizes that recovery looks different for everyone and can include diverse paths to wellness.
Trauma
Trauma-focused therapy uses specialized approaches designed to help people heal from traumatic experiences. These therapies are delivered using trauma-informed principles that create safety, build trust, and empower patients throughout the healing process.
Trauma-focused therapies include (but aren’t limited to):
- EMDR
- Cognitive processing therapy (CPT)
- Prolonged exposure (PE)
- Somatic therapy
- Internal family systems (IFS)
- Narrative exposure therapy (NET)
What Is Evidence-Based Therapy?
Evidence-based therapy is exactly what it sounds like: treatment backed by scientific research. When a therapy is considered evidence-based, that means it’s been studied in clinical settings, tested across different populations, and shown to improve outcomes. In other words, there’s real-world data that says it works.
But evidence-based care is about more than just numbers. It combines 3 things:
- The best available research
- The expertise of your provider
- Your preferences, values, and lived experience
That last part matters. Because even the most rigorously studied therapy won’t work if it doesn’t feel right for you.
Some of the most common evidence-based therapies11 include:
- Cognitive behavioral therapy (CBT)
- Dialectical behavior therapy (DBT)
- Eye movement desensitization and reprocessing (EMDR)
- Exposure and response prevention (ERP)
- Cognitive processing therapy (CPT)
- Acceptance and commitment therapy (ACT)
- Interpersonal therapy (IPT)
- Mindfulness-based cognitive therapy (MBCT)
These approaches aren’t one-size-fits-all, but they do give you a solid starting point. If you’re working with a provider who offers evidence-based care, your treatment plan should be grounded in both research and respect for your individual needs.
Individual vs. Group Therapy
Most therapies can be done in a group setting or one-on-one with a therapist. Each setting has its benefits.
Individual Therapy
Individual therapy means meeting privately with a therapist to talk through what’s going on. It’s what many people picture when they think of going to therapy. The one-on-one setting can feel more comfortable, especially for those who value privacy or prefer to go deeper into personal experiences.
This format can be especially helpful for people navigating trauma, since it offers a space to process at your own pace. That said, trauma-informed group therapy can also be effective for many people.
Group Therapy
Group therapy is led by a licensed therapist and usually includes 5–10 participants. Unlike peer support groups, group therapy has a structured format and a clinical focus. The therapist leads discussions, offers guidance, and helps everyone practice coping skills together.
A typical group might start with check-ins and introductions, then shift into learning and applying a therapeutic concept or tool. Participants are encouraged to ask questions and offer feedback to one another.
Group therapy supports 2 key aspects of recovery: structured treatment and connection with others who understand. Still, some people may not feel ready to open up in a group setting—and that’s okay. In those cases, starting with individual therapy might be a better fit.
Inpatient and outpatient treatment programs usually offer both group and individual sessions. Participating in both can offer a more complete healing experience that balances peer support with focused personal work.
Family Therapy
Family therapy can be a vital part of treatment, especially for children and younger adults. But it can support recovery at any age, and in all types of families, including both biological and chosen family.
These sessions create a safe, nonjudgmental space where each person has the chance to be heard, express concerns, and ask questions. This helps in 2 key ways:
- The person in treatment feels better understood and supported.
- Loved ones gain clarity about their role in recovery, which improves communication and interaction.
Family members can benefit from the process, too. It often helps them better understand their loved one’s condition, recognize patterns like codependency, and learn how to care for their own well-being.
Family therapy supports a biopsychosocial approach to healing by improving support systems that improve recovery as a whole.
Short-Term vs. Long-Term Approaches
Some people will go to therapy for years, but not everyone will want or need to. Depending on your needs and condition, a brief intervention (1–5 sessions) may be the best fit. Motivational interviewing is short-term by design; other therapies like CBT can also be adapted to shorter timeframes.
Being in therapy longer allows you to dive deeper into your patterns, history, and long-term goals. Some conditions benefit from ongoing support—for example, bipolar disorder often requires regular therapy12 to manage symptoms and prevent episodes. Depression related to specific life events (like job loss) may respond well to shorter-term treatment.
You can discuss with your therapist or primary care provider how long they recommend staying in therapy based on your specific situation and treatment goals.
Alternative and Holistic Therapies
There’s so much more to therapy than talking, and there can be much more to healing than conventional talk therapy.
Complementary and holistic therapies broaden your treatment options, offering ways to involve your mind, body, and spirit in your recovery. These approaches acknowledge the interconnected nature of mental, spiritual, and physical wellness. Examples include:
- Somatic therapy
- Sound healing
- Ayurveda (traditional Indian scientific healing system)
- Naturopathy (traditional medicine focusing on natural remedies)
- Psychedelic therapy (currently experimental and conducted in clinical research settings)
- Creative therapies (art, dance, creative writing)
These therapies can be done on their own, or alongside evidence-based therapy like CBT. Some of these therapies have growing research support, but many have not yet undergone the same level of clinical study as evidence-based treatments like CBT or DBT. That doesn’t mean they don’t work. In fact, some people benefit from these complementary options because they connect more to the way they’re healing—like painting what they can’t put into words, moving to release trauma, or tuning into the body to regulate their nervous system.
Addiction and mental health issues can feel overwhelming. But once you start taking steps toward feeling better, you might be surprised at just how good things can be.
How Will You Heal?
Your mental well-being is a vital component of health care. Whether you want the space to talk and be heard, work through trauma, overcome drug or alcohol addiction, or manage symptoms of a chronic mental illness, therapy is an avenue to healing.
One of the best parts about it is that there’s no one, right way to do it. It comes down to what you resonate with and what works for you.
Start your journey today: Use Recovery.com to find treatment centers offering the therapy of your choice.
FAQs
Q: What therapy is most effective for addiction?
A: There’s no one-size-fits-all answer, but cognitive behavioral therapy (CBT) is one of the most widely studied and commonly used approaches for treating substance use disorders. It helps people recognize unhelpful thought patterns, develop coping skills, and reduce behaviors linked to substance use.
Other therapies can be just as effective, depending on the person and their needs. These include dialectical behavior therapy (DBT), motivational interviewing (MI), contingency management, and trauma-informed therapies like EMDR. Many people benefit most from a combination of approaches tailored to their goals and circumstances.
Q: What type of therapy is best for mental health?
A: The best type of therapy depends on your goals, preferences, and what you’re experiencing. Cognitive behavioral therapy (CBT), dialectical behavior therapy (DBT), and psychodynamic therapy are commonly used and have strong evidence supporting their effectiveness.
Other approaches—like acceptance and commitment therapy (ACT), interpersonal therapy (IPT), trauma-informed care, or somatic therapies—may also be helpful. What matters most is finding a therapy and therapist that feel like a good fit for you.
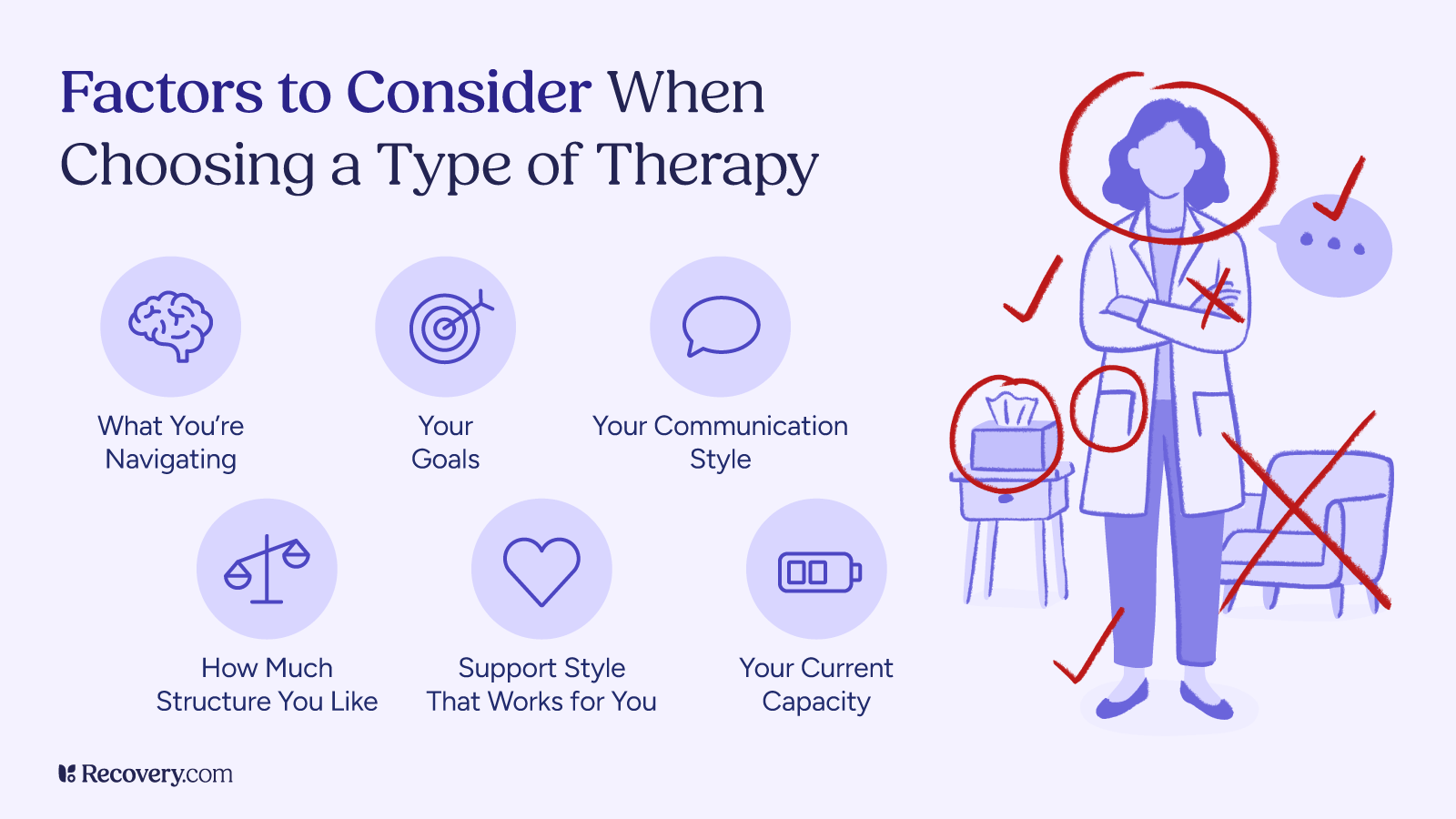
Q: How do I know what type of therapy is right for me?
A: Finding the right therapy depends on what you’re hoping to work on, how you prefer to communicate, and what kind of support feels most helpful. A licensed mental health professional can help you explore different approaches based on your needs, goals, and preferences. It’s also okay to try out a therapy style and switch if it doesn’t feel like the right fit—your comfort and growth matter most.
Q: What is a type of therapy used for both addiction and depression?
A: Cognitive behavioral therapy (CBT) and motivational interviewing (MI) are 2 approaches commonly used to treat both substance use and co-occurring mental health conditions like depression. These therapies help people explore the connection between thoughts, behaviors, and emotions, and support changes that align with their goals. When used together—or alongside other treatments—they can address both substance use and mental health symptoms in an integrated way.
Q: What is psychotherapy?
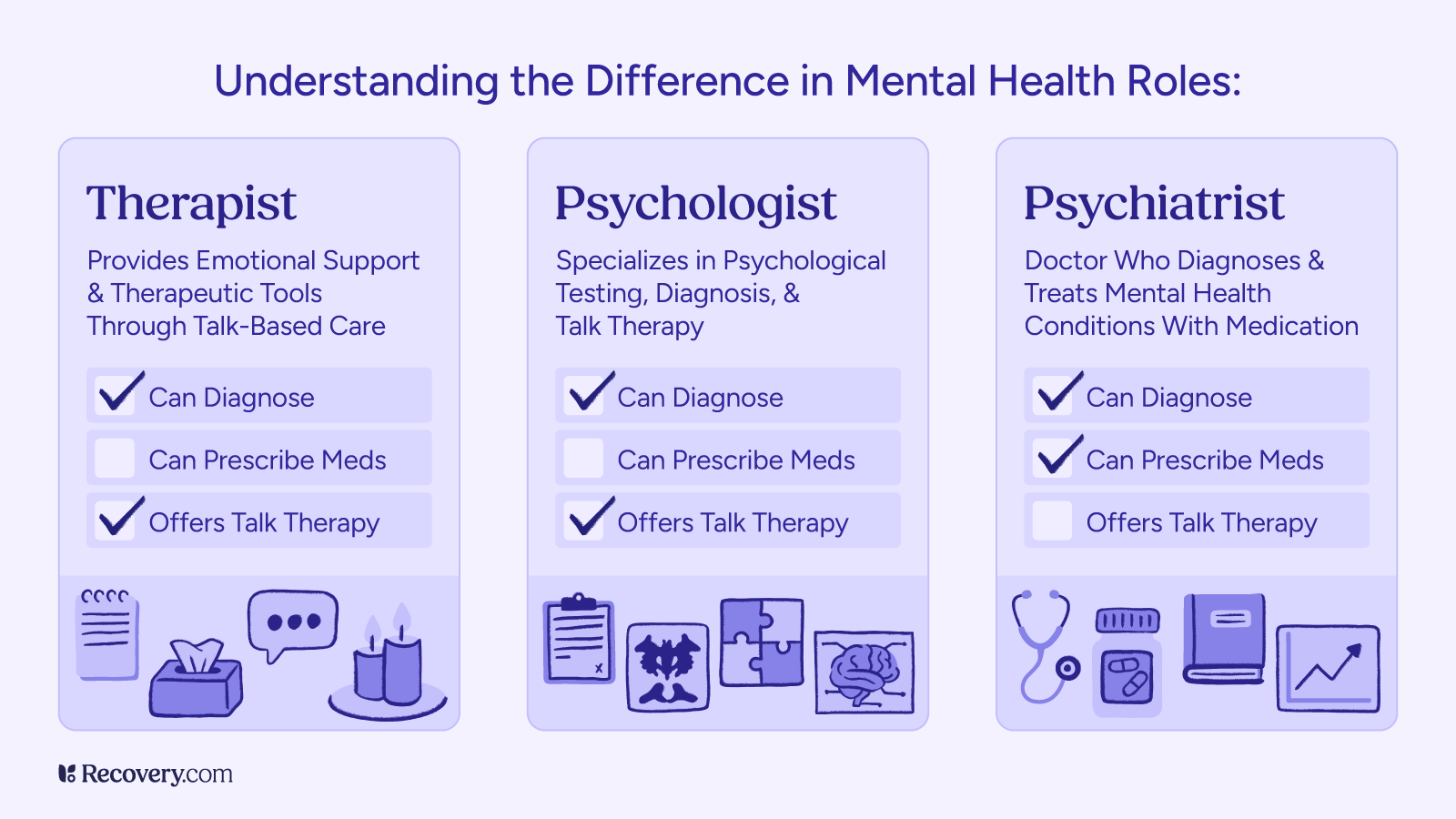
A: Psychotherapy, or talk therapy, involves working with a licensed therapist to explore thoughts, emotions, and behaviors. It helps people manage mental health conditions, cope with stress, and improve relationships.
Q: What is the best therapy for substance abuse?
A: Evidence-based treatments like CBT, Contingency Management, and Medication-Assisted Treatment (MAT) are highly effective for substance abuse. The best option depends on the individual’s substance use and co-occurring conditions.
Q: What are common types of therapy?
A: There are many types of treatment, each with its own approach and focus. Common options include:
- Cognitive behavioral therapy (CBT): Helps you recognize and change unhelpful thoughts and behaviors
- Dialectical behavior therapy (DBT): Focuses on emotional regulation, distress tolerance, and relationship skills
- Psychodynamic therapy: Explores how past experiences influence current feelings and behaviors
- Eye movement desensitization and reprocessing (EMDR): Often used to process trauma and reduce emotional distress
- Motivational interviewing (MI): Helps strengthen motivation for change, often used in addiction treatment
- Family therapy: Supports healthier communication and relationships within families
- Group therapy: Involves learning and healing alongside others with similar experiences, led by a therapist
Q: How can I find the right therapist for mental health and addiction issues?
A: Look for a licensed therapist who has experience with co-occurring disorders—also known as dual diagnosis—which means they’re trained to treat both mental health and substance use concerns. You can start by checking provider directories, asking your primary care provider for referrals, or searching through your insurance network. It’s okay to ask potential therapists about their experience and approach to make sure it feels like a good fit for your needs.
